Overview
Antenatal care is the care provided by skilled healthcare professionals to pregnant women and adolescent girls in order to ensure the best health conditions or outcomes for both mom and baby during pregnancy. It is a great opportunity to prevent and manage existing and potential causes of maternal and neonatal morbidity and mortality.
The 2016 WHO ANC model, now entailing 8 contacts/visits, is set to replace the previous focused-ANC model (FANC, WHO 2002) which recommended 4 ANC visits. It has fewer perinatal deaths than FANC, increased frequency of maternal and fetal assessment, and increased contact between pregnant women and respectful knowledgeable health care workers.
- Goals of antenatal care
- Diagnosis of pregnancy (initial visit) AND estimation of the gestational age (Nagel’s rule, assuming 28-day cycle)
- Identification of any potential complication
- Ongoing evaluation of the health status of both mother and fetus
- Anticipation of problems and interventions, if possible, to prevent or minimize morbidity
- Patient education and communication
- Antenatal care profile
- TB screening
- HIV test
- VDRL test
- Random Blood Sugar
- Full hemogram
- Blood Smear for malaria parasites
- Blood group and rhesus factor
- Urinalysis
- Safe vaccines during pregnancy
- Influenza
- HBV
- HAV
- Pneumococcus
- Meningococcus
- Typhoid
- Unsafe Vaccines in Pregnancy
- MMR
- Polio
- Varicella
- Yellow fever
- Danger Symptoms during pregnancy
- Bleeding Per Vagina
- Drainage of liquor (copious drainage that reaches the legs or makes the seat/bedding wet)
- Reduced fetal movements
- Fever
- Convulsions
- Throbbing headache associated with blurry vision
- New severe epigastric pain or Pain in RUQ
- Generalized body swelling
- Danger Symptoms during labor
- Labor for > 12 hours
- Excessive bleeding
- Rupture of membranes for > 12 hours before the onset of labor
- Convulsions during labor
- Loss of consciousness
- Cord or arm or leg prolapse
- Danger Symptoms during puerperium
- Excessive bleeding
- Fever
- Foul-smelling discharge
- Abdominal pain or cramps
- Painful or cracked nipples
- Mental disturbance
- Facial or hand swelling
- Headaches
- Convulsions
- Painful calf muscles
- Symptoms of labor
- Contractions
- Persistent
- Increase in frequency and intensity
- May or may not radiate to back
- Associated with hardening of the abdomen
- May be associated with
- Bloody show
- Drainage of liquor
- Contractions
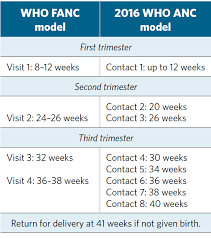
Recommended timings for prenatal care:
Every 4 weeks from diagnosis until 28 weeks
Every two weeks from 28 weeks until 36 weeks
Every week from 36 weeks to birth
Key Interventions
- Nutritional interventions
- Counseling on healthy eating and physical activity (to prevent excessive weight gain during pregnancy)
- Nutritional education on increasing daily energy and protein intake in undernourished populations (to reduce the risk of LBW neonates)
- Balanced energy and protein dietary supplementation (reduce risk of stillbirths and SGA neonates)
- Daily oral iron (60-65mg) and folic acid (400mcg primary prevention, 5mg to prevent recurrence) supplementation (to prevent maternal anemia, puerperal sepsis, LBW, and preterm birth)
- Maternal and fetal assessment
- Complete blood count or Hemoglobin levels
- Hyperglycemia (first detected at any time during pregnancy is classified as GDM)
- Alcohol and Substant abuse (past and present)
- Provider-initiated testing and counseling (PITC, integrated with testing for syphilis and other key viral tests)
- Fetal assessment
- Ultrasound scan before 24 weeks of gestation (Early ultrasound to estimate Gestational age and detect fetal anomalies and multiple pregnancies)
- Preventive measures
- Anti-D immunoglobulin (Given to non-sensitized Rh-negative women at 24-34 weeks of gestation to prevent RhD alloimmunization)
- Antihelminthics (given during the first trimester as part of worm reduction programs)
- Tetanus toxoid (for all pregnant women depending on previous vaccinations to reduce neonatal mortality from tetanus)
- Intermittent preventive treatment with Sufladoxine-pyrimethamine (IPTp-SP; for all pregnant women in the second trimester in malaria-endemic areas, doses given at least one month apart ensuring at least 3 doses are given)
- Oral pre-exposure prophylaxis using Tenofovir disoproxil fumarate (TDF; additional prevention choice for pregnant women at substantial risk of HIV infection)
Patient Education
Reinforce patient education at every visit regarding what to avoid and proper dietary habits. Assure the mother of normal events.
- Nutrition
- First trimester: 2300 kcal + 55g protein indicated for most women
- Limit caffeine to less than 150-300mg/day (associated with LBW and miscarriage)
- Avoid certain foods: high mercury fishes, liver, anything undercooked, saccharin
- Avoid certain supplements: chamomile, licorice, peppermint, raspberry leaf
- Vitamin supplementation is highly recommended
- Folate 600ug/day
- Iron 27 mg/day
- Weight gain
- Should be about 3-8 kg in the first trimester. Varies depending on the woman’s pre-pregnancy weight
- Safety measures
- Home Safety
- Tobacco cessation and EtOH abstention
- Seat belt use
- Exercise is OK, but avoid strenuous activity if there have been certain complications in previous pregnancies (e.g. >3 SABs, PROM, PTL, Cervical insufficiency, placenta previa, IUGR)
- Avoid contact sports (football)
- Safe vs unsafe OTC meds
- Safe: paracetamol
- Unsafe: NSAIDs (Ibuprofen)
- Social services as needed
- If low social economic status
- Symptoms of infections
- Pyelonephritis
- Fever
- Chills
- Hematuria
- Dysuria
- Pyelonephritis
- Symptoms of threatened loss
- Vaginal bleeding
- Severe cramping (Lower abdominal, Stabbing/Sharp)
- Passage of tissue
- Symptoms of labor
- Spontaneous rupture of membranes
- Contractions every 5 – 8 minutes for 1 hour
- Symptoms requiring prompt evaluation
- Signs of labor
- Rupture of membranes
- Vaginal bleeding
- Worsening edema, headaches, visual changes
- Peripartum and post-partum considerations
- Location of deliver
- Mode of delivery
- Labor analgesia and anesthesia wishes
- Breastfeeding
- Circumcision
- Post-partum contraception
Pre-conception care
Ideally, women planning to get pregnant should be evaluated before pregnancy to ascertain fitness to undertake pregnancy, provide health promotion and education, screen for high-risk pregnancies, and provide interventions to address the identified risks.
- Family History
- Hereditary conditions (Sickle Cell Disease, Mental illness)
- Medical conditions (DM, Gestational DM, HTN, HIV, Cervical and breast Ca)
- Congenital abnormalities
- Obstetric History
- Miscarriages
- Preterm deliveries
- Macrosomia
- Menstrual disorders
- Post-Partum Hemorrhage
- Prolonged subfertility
- Social History
- Exposure to radiation and chemicals
- Physical Examination
- General exam (head-to-toe)
- Vitals
- Systemic examination
- Investigations
- CBC
- RBS
- VDRL
- PITC
- Blood group and rhesus factor
- Interventions
- Health education and counseling
- Life-style interventions
- Assess dietary needs and give advice
- Reduce weight if overweight and gain weight if underweight
- Stop smoking, alcohol, use of drug, traditional herbs, and medications
- Discourage OTCs
- Timed Coitus
- Prophylaxis
- Folic acid started 3 months before conception to decrease the incidence of NTDs. 400ug primary prevention. 5mg to prevent the risk of recurrence.
- Change medications to less teratogenic drugs (Antiepileptics, warfarin, hydroxyurea)
First Trimester Visit
The first trimester includes the time of conception to the completion of the 12th week. Towards the end of the first trimester (1-13 weeks), the patient may be offered the first-trimester screen (U/S along with maternal serum hCG, AFP, and PAPP-A) to look for congenital anomalies. It is important to attain a baseline impression of the patient for which any changes may be compared when evaluating for pregnancy-related disorders.
- Normal events during the first trimester
- Normal Sx: Nausea and Vomiting, fatigue, breast tenderness, urinary frequency
- Spotting/bleeding (20% of pregnancies, 50% of which progress normally)
- Average weight gain (2-4 kg)
- Common complaints during the first trimester
- Breast enlargment and tenderness (Tx support bra)
- Nausea/vomiting/morning sickness (Tx Frequent snacking – carbs, anti-emetic – doxylamine)
- Fatigue (Tx adequate rest)
- Gingival bleeding
- Migraine-like headache (Tx ice packs)
- Dizziness (Tx adequae hydration, avoid rapid postural changes)
- The most common complication during the first trimester
- Spontaneous abortion
- Patient Biodata
- Name
- Age (issues affecting women at extremes of age)
- Parity and Gravidity
- Physical address (distribution of diseases)
- Marital status, Educational status, and economic resources/status of work (delayed until rapport is developed)
- History of the current pregnancy
- LNMP
- EDD (using Naegele’s formula)
- Quickening (if applicable, > 16 weeks)
- Other Symptoms (Pain, nausea, vaginal bleeding, breast pain)
- Confirmation of pregnancy and date (Ultrasound, Urine PDT)
- Past Obstetric historyProvides clues to potential problems that may develop in the current pregnancy (Miscarriage, Macrosomia, Operative vaginal delivery, HTN and DM in pregnancy)
- Date of delivery
- Length of pregnancy
- Type of deliver (+ indications for C-section and complications thereafter
- Precious C-section, Repeat C-section, and 2nd stage C-section predispose to cervical insufficiency
- Trial of scar (Requires nurse throughout, C/S within 30 minutes of trying a scar, No post C-section infection – >3-4 days in hospital)
- Vaginal birth after C-section (VBAC, 1 previous C-section can undergo VBAC)
- Duration of labor
- Birthweight of pregnancy
- Neonatal complications (NND, anomalies, MAS, Perinatal asphyxia, Macrosomia, SGA, Twinning High-order multiples)
- Sex of infant
- Current status of baby
- Any complications during pregnancy, labor, or puerperium (DM, HTN, DVT, PPH, APH, Sepsis, Obstructed labor, Operative deliver)
- Gynaecologic History
- Menstrual History (Important for understanding how the pregnancy is going to be dated)
- Menarche
- Duration of flow
- Estimation of amount
- Cycle length
- Contraceptive History
- Type
- When used
- Stopped and reason for stopping
- Sexual History (Sniff out STDs)
- Sexual debut
- STI History
- Screening History
- Pap smear
- Self-breast exam
- Mammography
- Gynecological Surgery History
- Cone biopsy or LLETZ (cervical insufficiency → second trimester miscarriages or preterm delivery)
- Myectomy or D&C or Metroplasty or MVA (weakens myometrium hence predisposing to uterine rupture during pregnancy or labor)
- Menstrual History (Important for understanding how the pregnancy is going to be dated)
- Past Medical and Surgical History
- Medical conditions
- Surgical operations
- Blood transfusions
- HIV status if known (and if on treatment, and the latest viral load)
- Duration of subfertility if any and any medication
- Family History
- Family history of diabetes, sickle cell disease, venous thromboembolism
- Siblings with birth defects, perinatal deaths, or miscarriage
- History of twinning (maternal side)
- Hypertension
- Support structure (husband etc.),
- History of physical/sexual abuse (associated with worse outcomes, more likely to be abused during pregnancy)
- Lifestyle and Social History
- Drugs, prescription drugs, EtOH abuse, Travel (Zika virus etc.),
- Teratogenic exposure (e.g. X-rays, toxins, chemicals, Rx drugs
- Physical exam
- General exam (Appearance and nutritional status, Head-to-toe, Vitals, Weight and BMI)
- BMI: To evaluate how much weight will be gained during pregnancy, being overweight raises the risk for gestational diabetes)
- Blood pressure: BP should go down during pregnancy, and increase may point us towards gestational hypertension, pre-eclampsia)
- Chest exam (Breast exam and heart sounds)
- Abdominal exam
- Inspection: scars, striae gravidarum, linea nigra, visible fetal movements
- Palpation: fundal height, fetal poles and fetal lie, presentation, level of presenting part (descent), estimation of liquor volume, fetal movements
- Auscultation: fetal heat sounds
- Pelvic exam
- Pubic hair distribution
- FGM (esp. type IV FGM – other operations on the external genitalia not for medical purposes)
- Varicosities, warts, and discharge
- Bimanual exam (uterine size, position, and contour at <12 weeks)
- Masses
- Cervical length
- Adnexa for masses
- Thyroid
- Breasts
- Skin
- General exam (Appearance and nutritional status, Head-to-toe, Vitals, Weight and BMI)
- Investigations
- CBC
- Hg and Hct: evaluation for anemia which may precede or arise during the pregnancy
- MCV: if microcytic obtain iron studies
- Platelets: should not change, thrombocytopenia may indicate pregnancy induced thrombocytopenia or ITP
- WBC count: elevated during pregnancy, 16K is upper limit of normal
- Blood Type, Rh factor and Atypical antibody test (AAT) screen
- Rh negative mother: at risk of maternal/fetal anti-D isoimmunization and should be worked up for anti-D antibodies via the atypical antibody test (AAT)
- U/E/Cs**:** Baseline renal function for comparison in the future if there is renal dysfunction
- Urinalysis and culture
- Proteins: 2+ proteins for PET
- Ketones
- Bacteriuria: UTI
- Glucosuria: GDM
- Asymptomatic bacteriuria (ASB): treat it immediately
- Increased risk of UTI and pyelonephritis during pregnancy: urinary stasis, compression of fetal head on bladder
- HBV screen
- All women should be screened for HBV even if they have been immunized (possibility of exposure prior to immunization, may be living with chronic Hepatitis B)
- positive HBsAg: LFTs for mum, and HbIg for baby after birth (increased risk of vertical transmission)
- STD screen (syphilis, GC/Chlamydia, HIV)
- HIV: recommended for all pregnant women as early as possible during each pregnancy
- “Opt-out” approach: signs waiver to decline (preferred)
- “Opt-in” approach: signs waiver to perform
- VDRL or RPR for syphilis
- Cervical swabs for Chlamydia and gonorrhoea: screen women who are 24 years or younger or women who are at “increased risk” (new or more than one sexual partner, History of STD, illicit drug use)
- HIV: recommended for all pregnant women as early as possible during each pregnancy
- Pap smear
- Women due for pap smear should be offered one at their first visit (as part of a well-woman checkup and screen)
- Rubella and Varicella IgG
- Positive Rubella and/or Varicella IgG: indicated of immunity
- The rubella vaccine (MMR) and varicella vaccine are NOT safe during pregnancy (live-attenuated)
- CBC
- Interventions
- Iron and folate supplements
- Tetanus toxoid (5 TT as per guidelines
- Mebendazole 500 mg SAT and S-P if from malaria endemic region (if first visit after 16 weeks)
- Manage or refer in case complications are found
Second Trimester Visits
The second trimester extends from the beginning of the 13th week after conception to the end of the 27th week. Any changes in personal History and Habits should be noted. Two routine tests performed in the second trimester include the triple/quad screen and the fetal anatomy ultrasound.
- Normal events in the second trimester
- Improved sense of well-being
- hCG levels peak around 12 weeks and begin to drop. Reduces Nausea and vomiing
- Mid pelvic pain (stress on the round ligament due to growing uterus)
- Quickening
- 18 – 20 weeks for primigravidas
- 16 – 20 weeks for multigravidas (earlier because they know what baby movements feel like)
- “Contractions” – Braxton Hick’s contractions heraldin the end of the 2nd trimester
- Average weight gain of 0.45kg per week
- Improved sense of well-being
- Common complaints in the second trimester
- Mid-pelvic pain
- Back pain
- Ongoing breast pain
- Unwanted hair growth or hair loss (Tellogen effluvium)
- Skin changes (Melasma/Chloasma, Striae gravidarum)
- Hemorrhoids (due to increased pressure on veins – Treat with Sitz baths , high-fiber diet and symptom control)
- Common complications in second trimester
- Cervical insufficiency (at risk of preterm delivery)
- Preterm premature rupture of membranes
- Preterm labor and delivery
- Miscarriages (much less common)
Quad screen
The quad screen is a maternal blood test that looks for 4 biomarkers – AFP, Estriol, hCG and Inhibin A. It is usually performed between 16-18/40 weeks. The most important biomarker is Maternal Serum AFP (major serum glycoprotein in embryo, MS-AFP peaks at 30 weeks)
| AFP | Estriol | hCG | Inhibin A | ||
|---|---|---|---|---|---|
| Down’s | Low | Low | High | High | HIgh |
| Turner’s | Low | Low | Very high | Very high | HIgh |
| Edward’s | – | Low | Low | – | HEdward’s is low |
| Patau | High | – | – | – | AFPatau’s is high |
AFP concentration in maternal serum
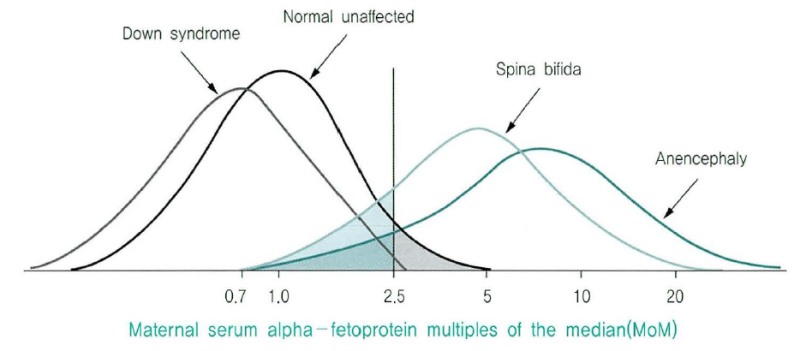
- What is the most common cause of abnormal AFP levels
- Inaccurate dating
- Differentials for low AFP (< 0.85 MoM)
- Inaccurate gestational age (early in pregnancy)
- Down’s syndrome
- Turner’s syndrome
- Investigations for low AFP
- Sonography: confirm gestational age and look for anomalies
- Thickened nuchal translucency
- Thickened nuchal fold
- Amniocentesis: to determine Karyotype
- Sonography: confirm gestational age and look for anomalies
- Differentials for high AFP (> 2.5 MoM)
- Inaccurate gestational age (further along pregnancy)
- Multiple gestation
- Neural tube defect
- Ventral wall defect
- Patau’s syndrome
- Fetal renal disease
- Investigations for high AFP
- Sonography: ascertain multiple gestation, NTD, VWD, or renal anomalies
- Amniocentesis for AF-AFP and AChE
- High levels: open NTD
- Normal levels: Increased risk of IUGR, SGA, Stillbirth, and pre-eclampsia
Fetal anatomy ultrasound
The fetal anomaly scan, AKA 20 week ultrasound, is routinely performed towards the end of the second trimester (18 – 22/40 weeks). It is often the first ultrasound done. Ultrasounds may still be done prior to and after this point for various reasons (including abnormal lab findings)
- What are we looking for on fetal anomaly scan?
- Fetal cardiac activity
- Fetal number/chorionicity
- Fetal biometrics (HC, BPD, FL, AC)
- Anatomy of major organ structures
- Placental appearance and location
- Amniotic fluid volume and index
- Uterine/adnexal anatomy including lower uterine segment and cervix
- What measurements are needed to estimate fetal weight? (used in Shephard’s and Hadlock’s formula)
- Head circumference
- Biparietal diameter
- Abdominal circumference
- Femur length

Third Trimester Visits
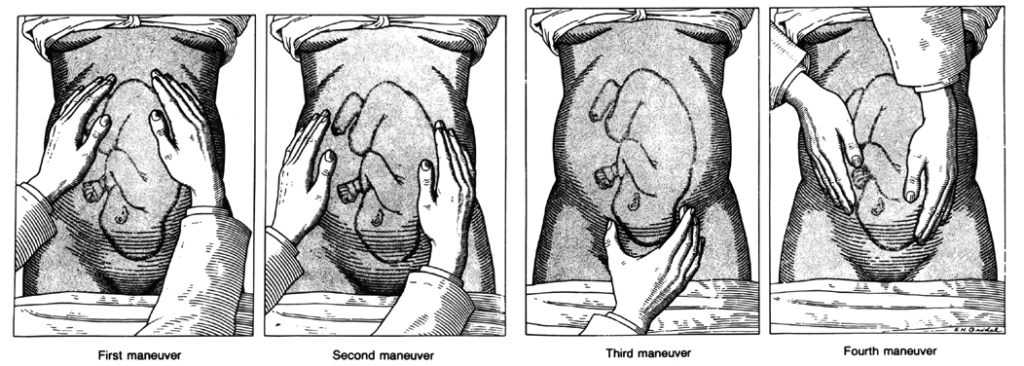
The third trimester extends from the beginning of the 28th week until the end of pregnancy. The fetus is typically viable by this points. The purpose for third trimester visits is to monitor fetal growth, position, and well-being, monitor for maternal complications, and detect issues that will alter the management of labor/delivery.
- Normal events in the third trimester
- Fetus moves into presenting position during the final several weeks of pregnancy
- Detected via Leopold maneuver
- US performed at 35-36 weeks can confirm position
- External cephalic version can be perfomred at 37-38 weeks if fetus is in breech position
- Lightening around 36-40 weeks as the fetal head descend into pelvis making it easier to breath, at the cost of increased urinary frequency and pelvic discomfort
- Mild cramping (Braxton Hick’s contraction, not sharp or persistent)
- Mild lower extremity edema
- Increased urinary frequency
- Fetus moves into presenting position during the final several weeks of pregnancy
- Common complications in the third trimester
- Preterm Prelabour rupture of membranes
- Prelabour rupture of membranes
- Preterm labor and delivery
- Abruptio placenta
- Placenta previa and vasa previa
- Pre-eclampsia
- Maternal complications
- UTI
- Gestational anemia
- Gestational diabetes
- Investigations
- Urinalysis
- Glycosuria (weak indicator for possible GDM)
- Proteinuria (2+ for pre-eclampsia, weak indicator)
- Repeat CBC (24-28 weeks)
- Hb < 10 g/dL for iron deficiency anemia. Tx w/iron.
- AAT (28 weeks)
- Rh negative and AAT negative: give RhoGAM at 28 weeks (calculate using Kleikhauer-Betke)
- GBS (36 weeks)*: Vagina and rectal samples
- Positive GBS screen: IV penicillin G during labor
- Urinalysis
Fetal growth, position, and well-being
- How to monitor fetal growth, position, and well-being
- Fetal Heart Tones
- Fundal height measurement
- Leopold maneuver
- Advanced testing (not routine)
- Non-stress test (NST)
- Biophysical profile (BPP)
- Differentials for uterine height greater than period of gestation
- Dating error
- Multiple gestation
- Polyhydramnios
- Macrosomia
- Pelvic tumor
- Gestational trophoblastic disease
- Full bladder
- Differentials for uterine height lesser than period of gestation
- Dating error
- Oligohydramnios
- IUGR
- IUFD
- Transverse lie
- What is the importance of the second pelvic grip during an obstetric exam?
- To confirm findings of the first pelvic grip
- To know whether the head is engaged
- To know the attitude
- To rule out cephalopelvic disproportion
- How to monitor for maternal compications
- Resting blood pressure (Should not exceed 120/80)
- SBP > 140 or DBP > 90 X 2 in the third trimester suggests pre-eclampsia
- Screening for Gestational Diabetes (24 – 28 weeks)
- Re-test for Gestational Anemia (May redevelop due to increasing fetal iron demand)
- Resting blood pressure (Should not exceed 120/80)
- How to detect issues that will alter the management of labor/delivery
- Repeat STD screening in high-risk pts
- GBS culture screening (36 weeks)
Leopold maneuver (Fundal grip → Umbilical grip → First pelvic grip → Second pelvic grip)
Gestation Diabetes Mellitus (GDM) Testing
1-hr 50g OGTT screening is provided to ALL pregnant women between 24 and 28 weeks gestation. Fasting blood glucose and 3-hr 100g OGTT is performed if the screen is positive.
