Overview
Approximately 20% of labour involves dystocia. Labour abnormalities can be classified as disorders of protraction and disorders of arrest. .Remember that Labour is defined as regular contractions (every 5 minutes lasting ~ 30 secs.) accompanied by cervical dilation and effacement leading to descent and expulsion of the fetus. Abnormal labour is the result of one or more abnormalities of the cervix, uterus, maternal pelvis, or fetus (power, passenger, or pelvis)
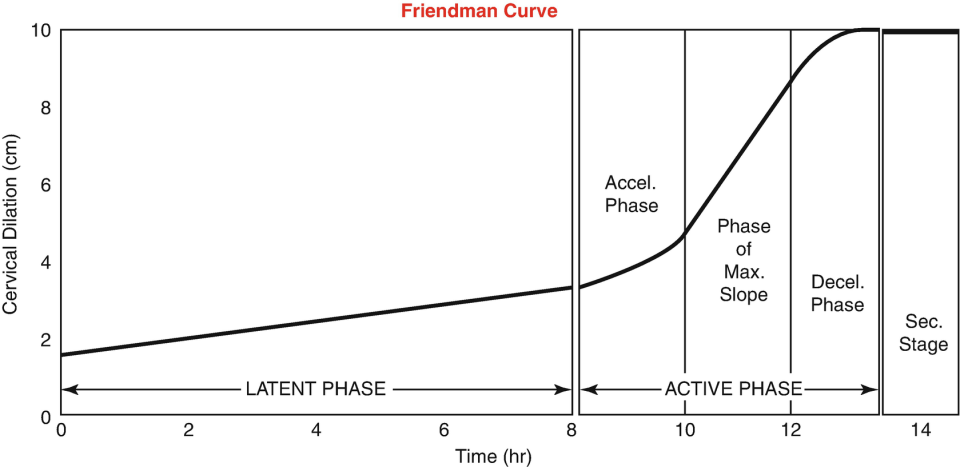
Expected values
| Event | Primipara | Multipara | |
|---|---|---|---|
| Latent stage one | closed to 4 cm dilation | < 20 hours | < 14 hours |
| Active stage one | 4 cm to full dilation | < 5-6 hours | < 4-5 hours |
| Rate of cervical dilation | acceleration of dilation in active stage one | 1.0 – 1.2 cm/hr | 1.2 – 1.5 cm/hr |
| Stage two | full dilation | < 2 hours | < 1 hour |
| Stage three | two hours following | 30 min | 30 min |
The Montevideo Unit
200 MVU over 10 minutes is needed for labour to progress properly. Lower than 200 MVU suggests prolongation or arrest of labour.
Montevideo units = [Peak pressure per contraction (mmHg) – resting tone of the uterus (mmHg)] X Frequency of contractions (in 10 minutes)
- A patient has 5 contractions in 1- minute, each with a peak pressure of 70 mmHg. The resting tone is 13 mmHg. How many Montevideo units are these?
- Has 285 MVU
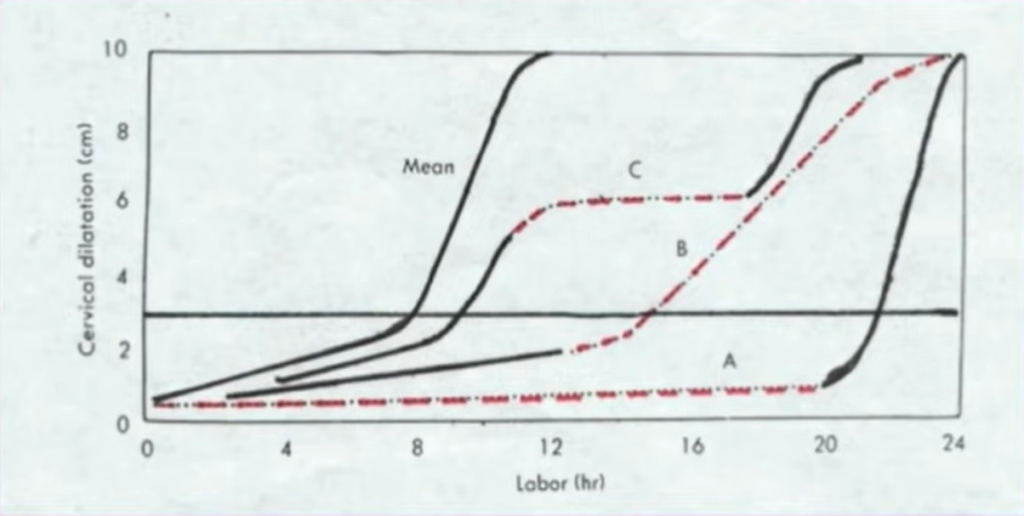
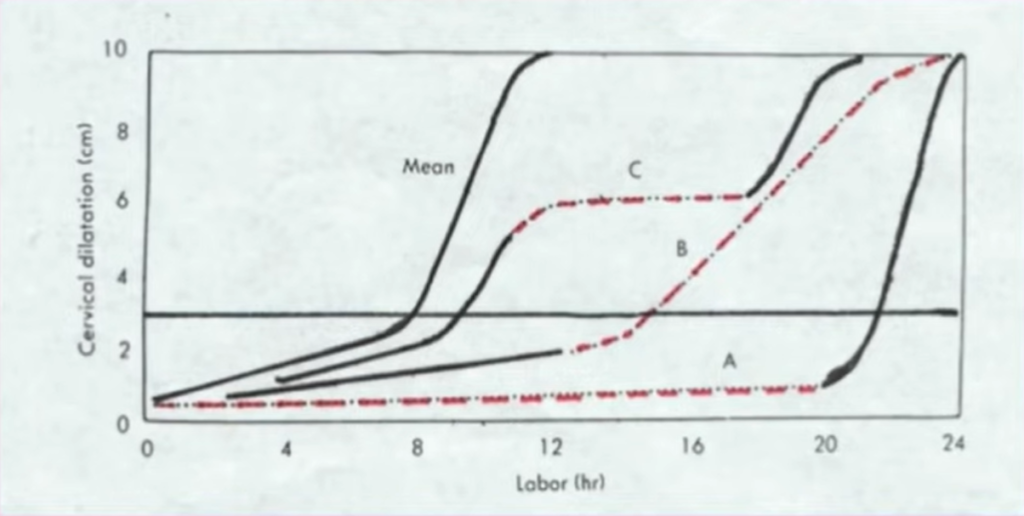
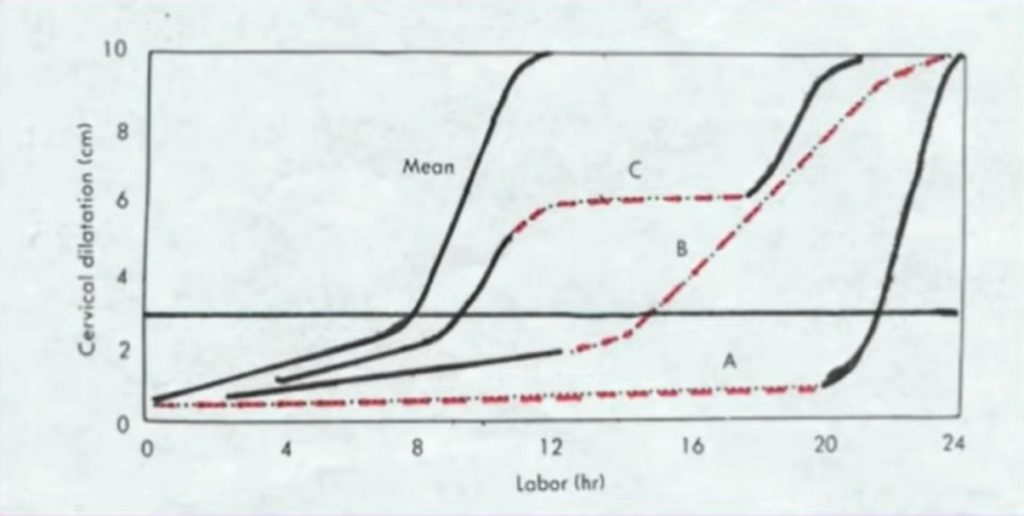
Protraction disorders
Prolonged latent phase
The patient is in labour *and *****remains < 3 cm dilated for > 20 hrs (primip) or > 14 hrs (multip)
- Causes
- Anesthesia (spinal) administered too early
- Irregular contractions
- Hypotonic (infrequent, weak contractions)
- Hypertonic (strong, short contrations)
- Differential
- False labour: cervix of a nullipara is long and closed, or just admitting a finger tip. The cervix of a multipara is not effaced (even if dilated).
- Treatment
- Rest (Let her sleep)
- Morphine sedation
- Contractions stop after administration in False labour (10%)
- Otherwise, cervical changes will have occurred by the time sedation wears off in True labor (90%)
- Amniotomy in the case of pre-eclampsia, gestational diabetes and sickle cell
Prolonged active phase
The patient is in labour and remains <1.2 cm/hr (primipara) or < 1.5 cm/hr (multipara) Causes are the 3Ps. Treatment relies on the tonicity of the contractions
- Passenger causesObstructed labour d/t
- Increased fetal size
- Abnormal orientation in utero (breech, transverse lie, etc.)
- Pelvic causes
- Cephalopelvic disproportion (If Hx of CPD with similar or smaller babies then it is probably the case. If no CPD with larger babies CPD is unlikely – can feel the promontory when measuring diagonal conjugate, head 4/5 above the brim, marked moulding)
- Power causes
- Dysfunctional or inadequate contractions
- Treatment
- Hypotonic contractions: IV Oxytocin
- Hypertonic contractions: Morphine sedation. Can administer Terbutaline.
- Eutonic contractions: Emergent Caeserean
Prolonged second stage
The patient is 10 cm dilated *and *fails to deliver the infant in ≤ 2 hrs (primip) or ≤ 1 hr (multip) [add one hour if the patient has received spinal anaesthesia]. Causes are also 3Ps. Good contractions are 3-4 in 10 minutes each lasting >40 seconds. No oxytocin for augmentation of labour in multipara unless you supervise it personally. Certainly not oxytocin for multipara >5, and not for longer than 2 hours. A multipara not steadily progressing in the second stage of labour and has started to push but has not delivered in 60 minutes is in great danger of uterine rupture.
- Passenger causes
- Increased fetal seize
- Persistent OT position
- Abnormal presentation (e.g. breech)
- Asynclitism
- Treatment
- Assess contractions
- Correct dehydration and ketosis by IV RL or NS
- Analgesia using Epidural or Pethidine 100mg + Promethazine 25mg IM
- Inadequate contractions → IV Oxytocin 5U in 500ml D5 to augment labor
- Adequate contractions → assess the engagement of the fetal head (if fully dilated you have access to the fetus)
- Engaged → Consider forceps or vacuum delivery attempt
- Not engaged (significant CPD)→ Emergent caesarean
- Indications for C-section in prolonged second stage
- Gross CPD
- Fetal distress
- Malpresentation
Prolonged third stage
Failure to deliver the placenta in ≤ 30 minutes
- Causes
- Inadequate contractions
- Abnormal placentation (accreta, increta, percreta)
Arrest disorders
Arrested active phase
The patient is in labour and has no cervical change for 2-3 hours. Tx is the same as the prolonged active phase.
- Treatment
- Assess contractions
- Inadequate → IV Oxytocin (usually given as prophylaxis)
- Adequate → Attempt manual removal; rarely hysterectomy
- Assess contractions
