Overview
Plasma cell disorders involve the abnormal proliferation of plasma cells. These B-cell clones synthesize and secrete a single monoclonal immunoglobulin or its fragments e.g. free light chains, and free heavy chains. These monoclonal immunoglobulins are termed M proteins and appear as the M spike in the gamma region of SPEP. They can accumulate in tissue and are freely excreted in urine in the absence of glomerular damage
Plasma cell dyscrasias account for 15% of malignant WBC neoplasms and 1% of cancer deaths.
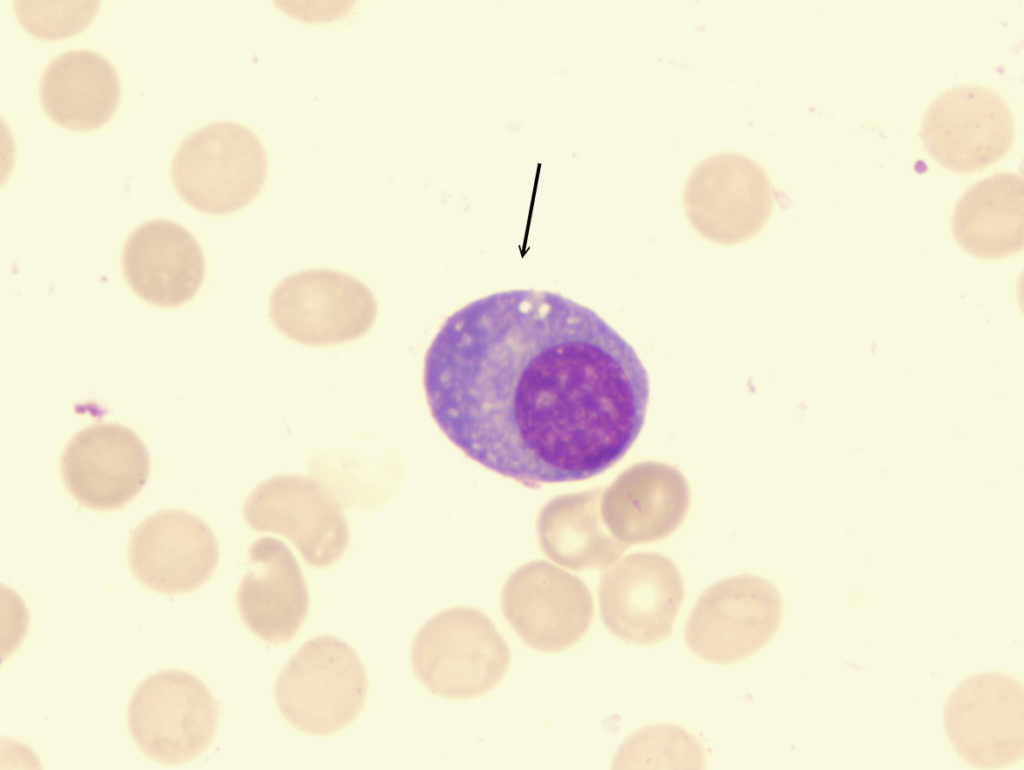
- Normal morphology of plasma cells
- Round Eccentric nucleus, “clock-face” coarse chromatin, Prominent perinuclear hof (clearing- golgi), abundant basophilic cytoplasm- also described as a fried-egg appearance
- Morphological patterns seen in plasma cell dyscrasias
- Flame cells: Variants that overproduce IgA (Vermillion staining, IgA carbs cytoplasmic projections stain red on Wright stain)
- Mott cells/ Morulae cell/ Grape cells: Plasma cells with abundant cytoplasmic inclusions or vacuoles (Russel bodies)
- Russel bodies: Hyaline intracytoplasmic inclusions
- Dutcher bodies: Pale staining intranuclear inclusions, single and large, most common in IgA myeloma
- Plasmablasts
- Plasma cells: with perinuclear hof and clockface chromatin
- Binucleate plasma cells
MGUS Vs. Smoldering Myeloma Vs. Multiple myeloma
| MGUS | Smoldering myeloma | Multiple myeloma | |
|---|---|---|---|
| M spike | Yes | Yes | Yes + UPEP |
| CRAB | No | No | Yes |
| Plasma cells on Bone marrow biopsy | < 10% | ≥ 10% | ≥ 10% |
Waldenstrom Vs. MGUS Vs. Multiple Myeloma
| Waldenstrom | MGUS | Multiple Myeloma | |
|---|---|---|---|
| Sx | Bleeding, Hyperviscosity, Hepatosplenomegaly | None | CRAB |
| Age | 60-70s | ||
| Labs | Normocytic anemia | None | Normocytic anemia, hYPERCALCEMIA |
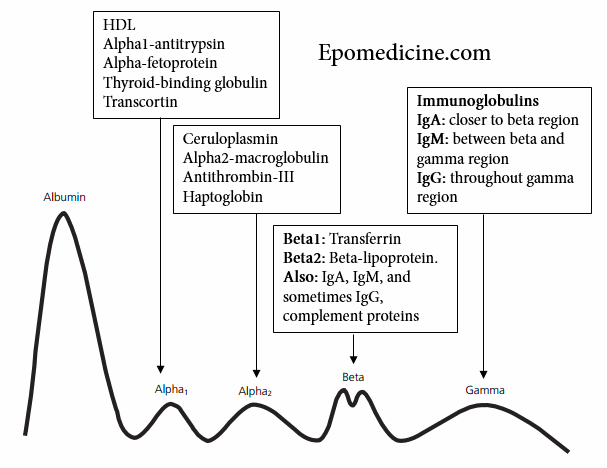
| SPEP | M-spike between beta and gamma region (IgM) | gamma spike (IgG) | gamma spike (IgG) |
| Bone marrow biopsy | Abnormal lymphocytic infiltration, PAS+ | < 10% plasma cells | > 10% plasma cells |
| Tx | Plasmapheresis | Watch and wait | Bortezomib, Thalidomide, Dexamethasone (VTD), then Melphalan → Bone marrow transplant. Other – Daratumumab |
Diagnostic Criteria
- Definition of MGUS
- Serum monoclonal proteins <30g
- Bone marrow plasma cells <10%
- Absence of myeloma-defining events or amyloidosis (or Waldenstrom macroglobulinemia in the case of IgM MGUS)
- Definition for smoldering MM
- Serum monoclonal protein (IgG or IgA) or urinary monoclonal protein and or clonal bone marrow plasma cells 1-60%
- Absence of myeloma defining events (CRAB) or amyloidosis
- Definition of multiple myeloma
- Evidence of end-organ damage that can be attributed to the underlying plasma cell proliferative disorder, specifically
- CRAB
- Any or more of the following biomarkers of malignancy
- Clonal bone marrow percentage ≥ 60%
- Involved: uninvolved serum-free light-chain ratio ≥ 100
- More than 1 focal lesion in MRI studies
- Evidence of end-organ damage that can be attributed to the underlying plasma cell proliferative disorder, specifically
Waldenstrom Macroglobulinemia (WM)
WM is the clonal proliferation of IgM-secreting plasma cells. Patients commonly present with platelet-type bleeding and hyperviscosity syndrome.
It is rare. Primarily occurs in the elderly at 60-80 years.
- Signs and symptoms
- Petechiae, Purpura, Epistaxis (due to thrombocytopenia)
- Headache, Visual changes, Diplopia, papilledema, Raynaud (hyperviscosity syndrome)
- Hepatomegaly (20%)
- Splenomegaly (15%)
- Lymphadenopathy (15%)
- Diarrhea and malabsorption
- Peripheral neuropathy (54%, symmetrical)
- Investigations
- Complete Blood Count:
- Normocytic anemia (80%)
- Thrombocytopenia (50%)
- Serum Protein Electrophoresis: best first step
- M-spike between the beta and gamma region (IgM is heavier than IgG)
- Bone Marrow Biopsy: most accurate test
- Abnormal lymphocytic infiltration
- PAS+
- Complete Blood Count:
- Treatment
- No medical therapy is asymptomatic
- Refer for Monitoring by a specialist
- Plasmapheresis
- Chemotherapy and immunotherapy for long-term management
Monoclonal Gammopathy of undetermined significance (MGUS)
MGUS is the detection of monoclonal paraproteins without evidence of symptoms. Plasma cells in the bone marrow are normal (<10%). It is usually diagnosed on routine serum protein investigations. There are no clinical complications. 1-2% of patients go on to develop Smoldering Myeloma. Treatment is “watchful waiting”.
Prevalence is highest at > 70 years.
Multiple Myeloma (MM)
Multiple myeloma is characterized by the accumulation of plasma cells in the bone marrow, the presence of M-proteins in serum and urine, and CRAB (Hypercalcemia, Renal dysfunction, Anemia, Bone disease) in symptomatic patients. Myeloma cells arise from post-germinal plasma cells that have already undergone class switching and somatic hypermutation. They localize in the bone marrow (which is the natural “home” of plasma cells) and secrete paraproteins (mostly IgG) which can be detected in serum. Overall, the median survival with non-intensive chemotherapy is 3-4 years.
Multiple myeloma accounts for 1% of all cancers and 10% of hematologic malignancies. 99% of cases occur over 40 years. The median age of diagnosis is 66 years. Kenya GLOBOCAN 2020 reported 707 new cases and 583 deaths.
Smoldering MM: Asymptomatic. Labs show monoclonal gammopathy but there is no end-organ or tissue damage. Some may develop from MGUS. 2% develop into multiple myeloma.
Revised International staging system (RISS) for MM
| Stage I | B2-microglobulin <3.5mg/L AND albumin is 3.5g/dL or greater AND standard genetic AND normal LDH levels |
|---|---|
| Stage II | Not stage I or Stage III (in between) |
| Stage III | B2-microglobulin >5.4mg/L AND high-risk cytogenetics |
- Risk factors for Multiple Myeloma
- Black
- Male
- Family History of MM
- Signs and Symptoms
- Bone paint (70%) and pathologic fractures (due to lytic lesions)
- Neuropathy (due to spinal cord compression)
- Fatigue, pallor, breathlessness (due to anemia)
- Recurrent and/or severe infections (due to defective antibodies and neutropenia)
- Easy bruising and bleeding (due to thrombocytopenia, and interference with coagulation factors and platelet function)
- Polydipsya, Polyuria, Urolithiasis, Anorexia, Abdominal pain, Vomiting, Constipation, and Mental disturbance(due to renal failure and hypercalcemia – stones, bones, abdominal moans and psychiatric overtones)
- Macroglossia, Carpal tunnel syndrome, Subcutaneous nodules, and Diarrhea (due to amyloidosis in 5%)
- Headache, Visual disturbance, Confusion, Neuropathy, and Heart failure (Hyperviscosity syndrome seen in 2%)
- Investigations
- To evaluate for clonal plasma cells
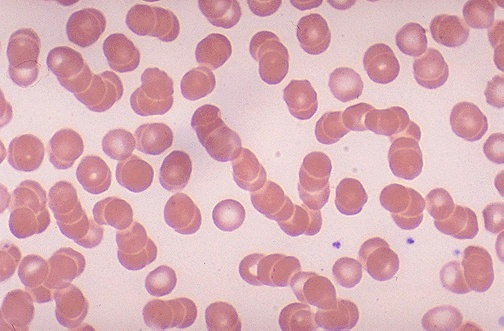
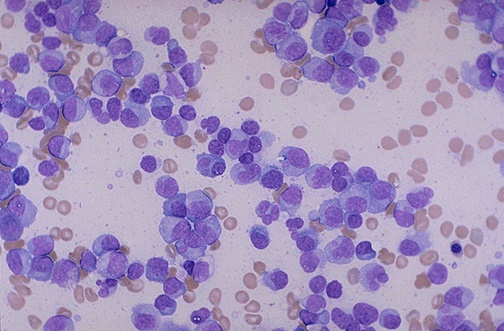
- Peripheral Blood Film
- Abnormal plasma cells (15%)
- Rouleaux formation (due to increased plasma proteins. Need 10 RBCs in a row)
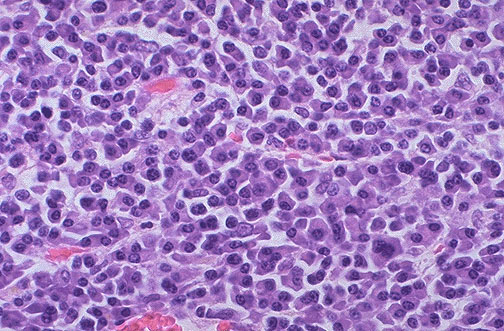
- Bone Marrow Aspirate or Biopsy
- Increased plasma cells with abnormal forms (>10%)
- Immunohistochemistry or Flow cytometry
- CD38+, CD138+, CD45-
- Peripheral Blood Film
- To detect clonal paraproteins
- Serum protein electrophoresis
- M-spike in the gamma region – IgG (60%), IgA (20%), Light chains (Kappa or lambda),
- Immune paresis (reduced normal Ig amount)
- Urine protein electrophoresis: 24 hour urine collection for Bence Jones proteinuria (2/3)
- Serum protein electrophoresis
- To evaluate end-organ damage
- Complete Blood Count: Anemia (NN or macrocytic), Neutropenia, Thrombocytopenia in advanced disease
- Comprehensive Metabolic Panel: Elevated Calcium, Elevated Creatinine (20%), Low albumin (advanced)
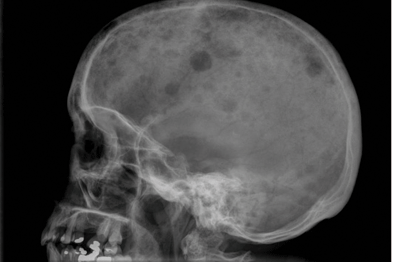
- X-ray and CT-scan for areas with bone pain and fractures + General skeletal survey:
- Lytic bone lesions (’soap bubble appearance”),
- Pathological fractures,
- Vertebral body compression,
- Osteopenia,
- Osteoporosis
- ESR: elevated
- For risk stratification
- B-2 microglobulin: raised
- <3.5 mg = good prognosis
- 5.5 mg = poor prognosis
- FISH: Hyperdiploidy (>50% of tumors)
- ESR: >100
- B-2 microglobulin: raised
- To evaluate for clonal plasma cells
- Candidates for bone marrow transplant
- <65 years
- Without comorbidities
- Treatment for bone marrow transplant-eligible patients
- Primary induction with Bortezomib, cyclophosphamide, and dexamethasone
- Autologous bone marrow transplant
- Maintenance therapy with Lenalidomide
- Treatment for bone marrow transplant-ineligible patients
- Long-term chemotherapy with Melphalan, prednisone, and thalidomide
- Supportive treatment
- Hydration, Furosemide, and Glucocorticoids for symptomatic hypercalcemia Hydration is also useful for renal failure to aid excretion of immunoglobulins
- Bisphosphonates – second-line for hypercalcemia (easy to tip the patient into hypocalcemia)
- Prophylactic vaccination
- Erythropoietin for anemia

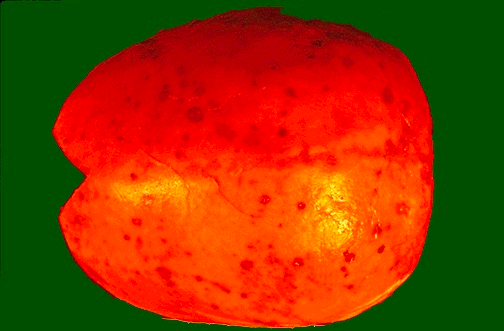
Solitary Plasmacytoma
A solitary plasmacytoma is an isolated plasma cell tumors of bone or soft tissue. It commonly occurs in the Mucosa of the Respiratory tract, Gastrointestinal tract, and Skin.
