Overview
Macrocytic anemia is characterized by Low Hb and High MCV (> 100). B12 and folate are required for the maturation of RBCs. Immature RBCs are larger, hence the increase in MCV in B12/Folate deficiency. A false normal MCV can occur in severely malnourished patients with both B12/Folate deficiency and IDA.
- Causes of macrocytic anemia
- Megaloblastic anemia
- B12 deficiency
- Folate deficiency
- Cytotoxic drugs
- Phenytoin
- Sulfa drugs
- Trimethoprim
- Hydroxyurea
- Methotrexate
- 6-MP
- Non-megaloblastic anemia
- Chronic alcoholism
- Liver disease
- Hypothyroidism
- Diabetes Mellitus
- Megaloblastic anemia
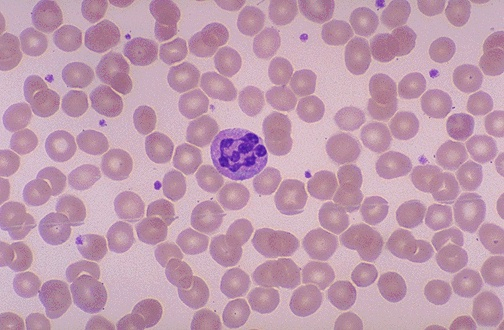
- Characteristic pathologic finding in macrocytic anemia
- Large, immature RBCs (macro-ovalocytes)
- Hypersegmented neutrophils (more than six lobes)
- Investigations
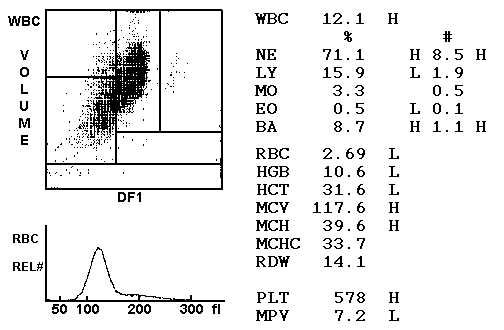
- Complete Blood count
- Decreased Hb
- Elevated MCV (macrocytic > 100fL)
- Decreased HCT
- Increased MCH
- Normal MCHC (Hb count is proportionally increased)
- WBC variable
- PLT variable
- PBF
- RBC – Macro-ovalocytes in megaloblastic, Rounded-macrocytes in non-megaloblastic
- Anisopoikilocytosis
- Hyperchromic red cells
- RBC inclusions: Basophilic stippling and Howell-jolly bodies
- Leukocytes: Polysegmented PMNs (Right-shift neutrophils) and **Leukopenia (**variable)
- Decreased platelets
- Low reticulocytes
- Bone Marrow
- Diserythropoiesis: Nuclear borders, Nuclear bridging, Abnormal mitosis – abnormal erythropoiesis with bizarre bone marrow morphology and ineffective erythropoiesis
- Marrow is markedly hypercellular (mainly due to nuclear proliferating erythroid precursors)
- Reversed M:E ratio (from 1:1 → 1:6; normal 2:1 → 4:1) – marked erythroid hyperplasia
- Intramedullary haemolysis (Ineffective erythropoiesis) – death of developing erythroid cells at the site of production and or production of non-viable red cells
- Megaloblastic changes: asynchrony of nuclear and cytoplasmic development
- Abnormalities in Granulopoiesis: Giant metamyelocytes
- Biochemical tests
- Elevated homocysteine
- Elevated serum bilirubin
- Elevated serum LDH
- Decreased Haptoglobin
- Diagnostic test for B12 deficiency
- Decreased serum B12
- Elevated serum methylmalonic acid
- Elevated urine methylmalonic acid
- Schilling test for B12 deficiency: diff IF Deficiency from other caused of B12 Deficiency
- Diagnostic test for Folic acid deficiency
- Decreased serum folic acid
- Normal methyl malonic acid levels
- Complete Blood count

Differences in clinical presentation of Folate and B12 deficiency
| Folate deficiency | B12 deficiency |
|---|---|
| Peripheral neuropathy absent | Peripheral neuropathy present |
| Ataxia absent | Ataxia present |
| Subacute combined degeneration absent | Subacute combined degeneration present |
| Normal serum and urine methylmalonic acid | Elevated serum and urine methylmalonic acid |
| Elevated serum homocysteine | Elevated serum homocysteine |
Folate Deficiency
Folate deficiency is classically seen in chronic alcohol intake, malnutrition, *and *people who do not eat vegetables. Folate stores last shorten than B12 stores (about 3 months), so it is more common than B12 deficiency
- Absorption of folate
- Folate is absorbed in the Jejunum and Ileum
- Dietary folate is in the polyglutamate form while supplementary folate is in the monoglutamate form
- Conjugase enzyme converts polyglutamate folate to its monoglutamate form
- Absorption is by passive or active transport
- Active transporters include: Reduced Folate carrier (RFC), Proton-coupled folate transporter (PCFT), and Folate receptor proteins (FRa, FRB)
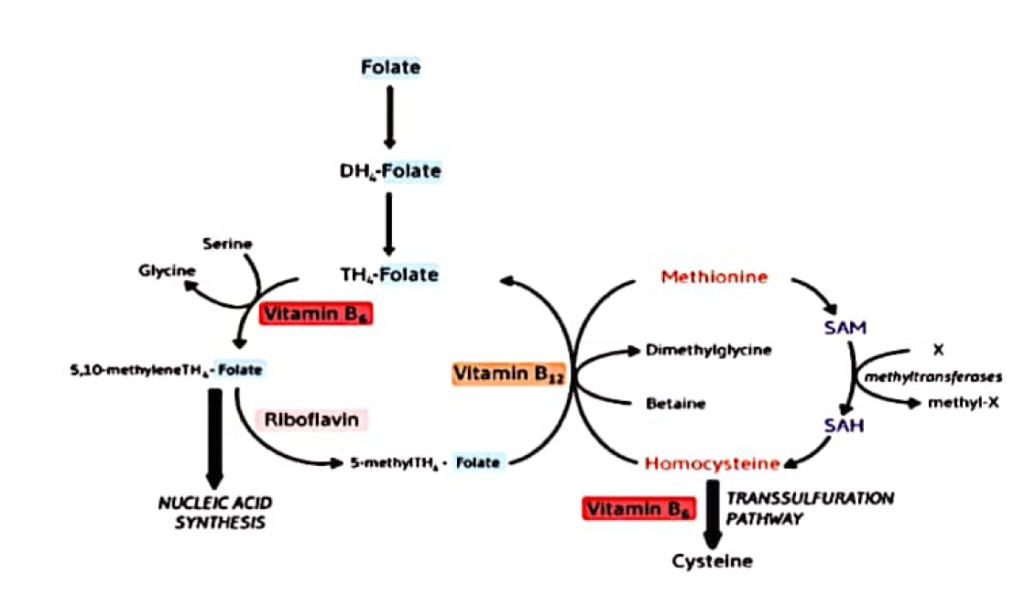
- Physiological role of folate
- Synthesis of DNA (dTMP from dUMP)
- Single carbon-unit transfer (conversion of homocysteine to methionine)
- Role of B12 and Folate in hematopoiesis
- Megaloblastic changes (due to nuclear-cytoplasm asynchrony/dysynchrony)
- Ineffective erythropoiesis (defective DNA synthesis and block in cell division)
- Causes of folate deficiency
- Decreased intake
- Chronic alcohol intake
- Malnutrition
- Overcooked vegetables and people who do not eat vegetables
- Elderly
- Decreased absorption
- Coeliac disease
- Tropical Sprue
- Crohn’s disease
- Short Bowel syndrome
- Drugs
- Phenytoin (inhibits intestinal conjugase needed for folate absorption – this is why we do not give Phenytoin to expectant mothers!)
- Zidovudine
- TMP-SMX
- Methotrexate
- Carbamazepine
- Valproate
- Increased demand
- Pregnancy
- Hemolytic anemia
- Exfoliative skin disease
- Hemodialysis
- Decreased intake
- Treatment
- PO Folate supplementation 5mg qd for 4 months
- B12 supplementation (unless normal B12 levels)
- Discontinue offending medication
- Discourage alcohol use
- Why should patients with severe deficiency receiving folate/B12 supplementation be admitted for observation (at least two weeks)?
- Can precipitate severe Hypokalemia as RBCs are made
B12 deficiency
B12 deficiency is classically seen in chronic alcoholism, malnutrition, and strict vegetarians. Vitamin B12 stores in the liver last about 2-3 years so deficiency is rare. B12 is also required for myelination in addition to hematopoiesis, hence deficiency leads to subacute combined degeneration.
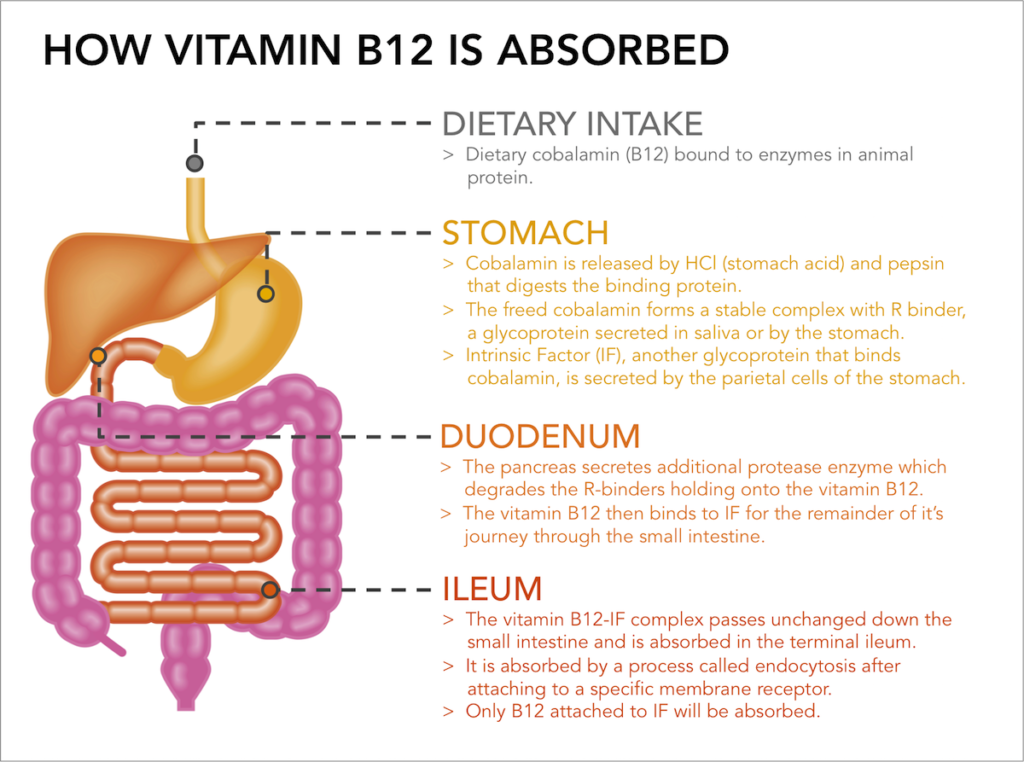
- Absorption of B12
- The salivary gland and fundus of the stomach secrete R-binders/ Transcobalamin-1/ Haptocorrin which binds to free B12
- Dietary B12 bound to proteins is released by enzymes in the stomach and ileum
- Pancreatic proteases release B12 from its R-binders
- Parietal cells secrete Intrinsic Factor which binds to B12 in the intestines
- B12-IF complex is absorbed by receptor- mediated endocytosis ATP-Binding Cassette Protein (ABCC1) or Multidrug Resistant Protein 1 (MDRP1)
- Physiological role of B12
- Folate metabolism (deficiency causes Folate trap and reduced DNA/RNA synthesis)
- DNA/RNA synthesis (through DNA methylation by SAM)
- Succinyl-CoA synthesis (for the synthesis of hemoglobin)
- Causes of B12 deficiency
- Decreased dietary intake (Vegans)
- Pernicious Anemia
- Atrophic Gastritis
- Achlorhydria
- Gastrectomy/ Bariatric surgery
- Pancreatic insufficiency
- Terminal ileal resection
- Crohn’s disease
- Diphyllobothrium latum infection
- The Folate trap
- In B12 deficiency, folate becomes trapped in its inactive 5-methyl-THF form
- Therefore, it cannot be converted to it’s active form, 5,10-methylene TH4-folate, which is required for nucleic acid synthesis
- Signs and symptoms
- Anemia: fatigue, weakness, palpitations, pallor
- Tongue: Red “beefy” tongue, glossitis, atrophy of papillae
- Peripheral neuropathy
- Glove and stocking distribution of pain and numbness (paraesthesia)
- Subacute Combined Degeneration
- Decreased deep tendon reflexes
- Decreased vibration sense
- Positive Babisnki
- Paraesthesia
- Psychiatric manifestations
- Ataxia
- Atherosclerosis: Due to increased homocysteine levels, also increases the risk for thrombosis and myocardial infaction
- Treatment Nerve damage from B12 deficiency is permanent. Supplementation may improve peripheral neuropathy within the first 3-6 months. However, there is little effect on cord signs.
- Monthly Parenteral Vitamin B12 replacement
