Anaemia is defined as a decrease in red cell mass as evidenced by low haemoglobin concentration in blood below the reference range for a given age or sex in a given population or geographic location. WHO gives the reference value for Hb <13g/dL in adult males and <12g/dL for adult females as criteria for anemia. Most patients do not need to be transfused. Chronic anemia is particularly well-tolerated, and iron supplements safely and cost-effectively raise the hemoglobin in IDA. It is still very important to ESTABLISH THE CAUSE in patients with anemia.
Classification of Anaemia
| Hemorrhage | Acute Loss | Trauma |
|---|---|---|
| Chronic Loss | Upper and Lower GI bleed, Menorrhagia, Hematuria | |
| Hemolysis | Inherited Hemolytic Anemia | Membranopathies, Enzymopathies, Hemoglobinopathies |
| Acquired Hemolytic Anaemia | Alloimmune, Autoimmune, TTP, HUS, Malaria | |
| Diminished Erythropoiesis | Microcytic Anaemia | Defective Heme synthesis, Defective Globin Chain |
| Macrocytic Anaemia | Megaloblastic and Non-megaloblastic macrocytic anemias |
- Indications for blood transfusion in anaemia
- Hb < 7 g/dL (especially in acute anemia)
- Symptomatic Anaemia
- Comorbidities e.d. Ischemic Heart Disease
- Treatment of severe anemia with heart failure
- Transfuse with caution to restore Hb to safe levels of 6-8 g/dL
- IV/PO Furosemide 40mg
- Check for signs of worsening congestion (JVP, basal crackles). If present, stop and treat.
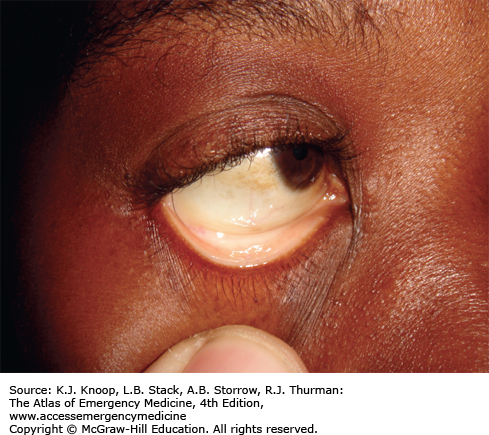
- Signs and symptoms of anaemia
- Fatigue, weakness, pallor, breathlessness
- Pallor: Seen on mucous membranes and conjunctivae
- Jaundice: seen in haemolytic anaemia
- Pica: Craving for ice or dirt. Seen in IDA
- Features of a hyperdynamic state
- Bounding pulses
- Tachycardia/palpitations
- Flow murmur
- Pulsatile sound in the ear
- Possibly heart failure (anaemia-induced heart failure)
- Features of extramedullary haematopoiesis
- Hepatosplenomegaly
- Paravertebral mass
- Widening of diploic spaces of the skull
- Laboratory Investigations for patients with anaemia
- To establish that there is anaemia
- Complete blood count for Hemoglobin and Hematocrit
- To classify the anaemia
- Red cell indices (MCV, MCH, MCHC) and Peripheral blood film
- Size: Normocytic, Microcytic, Macrocytic
- Degree of haemoglobinization: normochromic, hypochromic
- Shape e.g. Poikilocytes
- To establish the cause of anaemia
- Decreased Erythropoiesis
- Bone marrow aspirate or Trephine Biopsy: for bone marrow failure
- Iron, Folate and B12 levels: for hematinic deficiency
- Excessive loss or destruction
- Urinalysis and Serum study (Bilirubin, Haptoglobin, LDH) for hemolytic anaemia
- Stool for ova and cysts
- Gastroscopy and Colonoscopy
- Decreased Erythropoiesis
- To establish that there is anaemia
Causes of anemia according to morphology
| Normocytic anaemia | Acute blood loss, Anaemia of chronic disease, Bone marrow fialure, Renal failure, Hypothyroidism, Hemolysis, Pregnancy |
|---|---|
| Macrocytic anemia | B12 and folate deficiency, Alcohol excess, Reticulocytosis, Cytotoxics, Myelodysplasti syndrome, Hypothyroidism |
| Microcytic anemia | Iron deficiency anemia, Thalassemia, Sideroblastic anemia |
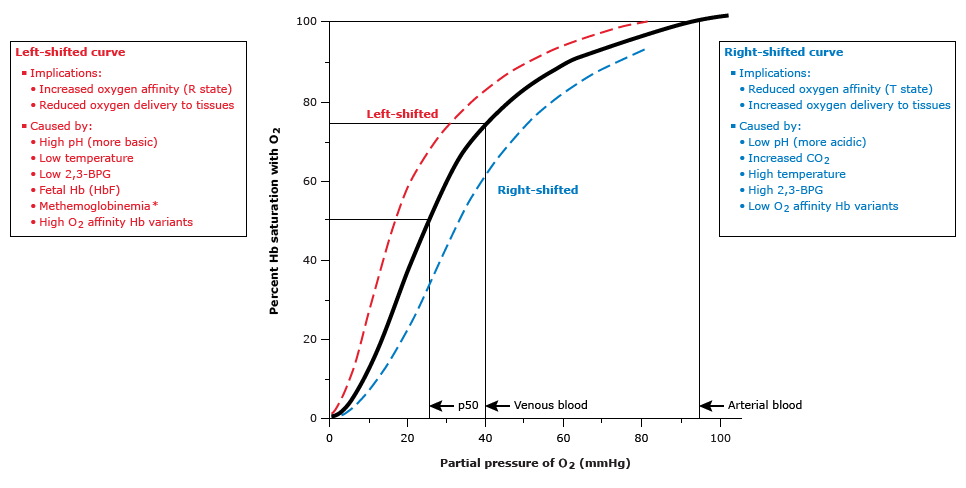
- Oxygen-Hemoglobin dissociation curve ****
- Describes the Oxygen carrying capacity of Haemoglobin at different PO2
- Co-operativity – binding of one O2 molecule facilitates the second molecule binding
- P50 is 26.6mmHg (PO2 at which Hb is half saturated with O2)
- Normal position depends on: 2,3-DPG concentration, H+ concentration, CO2, Hb structure
- Right shift (decreased affinity): High 2,3-DPG, H+, CO2, HbS (Also BAT ACE)
- Left shift (Increased affinity): Low 2,3-DPG, HbF
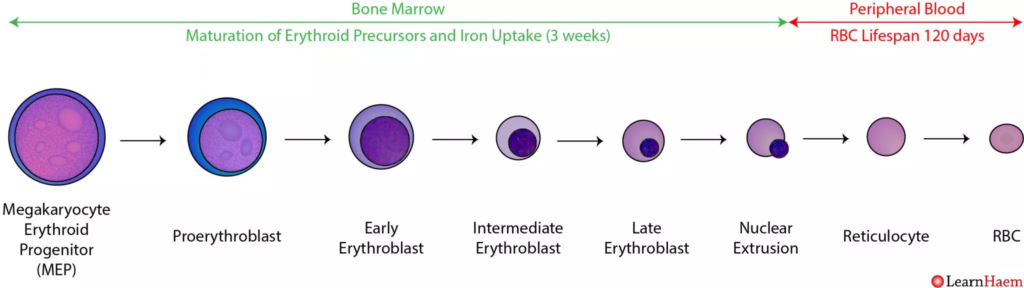
- Stages of erythropoiesis and morphology of precursors
- In Bone marrow
- Hematopoietic stem cell: round, non-adherent, with a rounded nucleus and low cytoplasm-to-nucleus ratio, resemble lymphocytes
- Proerythroblast: Large cells, basophilic cytoplasm, Large nucleus
- Erythroblast: basophilic cytoplasm, Smaller nucleus, no nucleoli
- Normoblast: acidophilic cytoplasm, compact nucleus
- Reticulocyte: acidophilic cytoplasm, granules composed of cytoplasmic ribosomal RNA
- In blood
- Reticulocytes
- Erythrocyte: Eosinophilic, biconcave shape, central pallor no more than 2/3 of diameter, diameter of 7um
- In Bone marrow
- Causes of anaemia of diminished erythropoiesis
- Inherited genetic defects
- Defects leading to stem cell depletion
- Fanconi anaemia
- Telomerase deficiency
- Defects affecting erythroblast maturation: Thalassemia syndromes
- Defects leading to stem cell depletion
- Nutritional deficiencies
- Deficiencies affecting DNA synthesis:
- B12 deficiency
- Folate deficiencies
- Deficiencies affecting haemoglobin synthesis
- Iron deficiency
- Deficiencies affecting DNA synthesis:
- Erythropoietin deficiency
- Renal failure
- Anaemia of chronic inflammation
- Immune-mediated injury of progenitors
- Aplastic anaemia
- Pure red cell aplasia
- Inflammation-mediated iron sequestration
- Anaemia of chronic inflammation
- Primary hematopoietic neoplasm
- Acute and Chronic leukaemias
- Myelodysplastic syndrome
- Myeloproliferative neoplasms
- Space-occupying marrow lesions
- Metastatic neoplasm
- Granulomatous disease
- Infections of red cell progenitors
- Parvovirus B19 infection
- Unknown mechanisms
- Endocrine disorders
- Hepatocellular liver disease
- Inherited genetic defects
