Knowing the physiology and pathology behind wounds is important in surgery since it is a specialty that primarily deals with wounds.
Overview
| Term | Definition |
|---|---|
| Wound | A break in the integrity of skin or tissue, often associated with disruption of structure and function, and is commonly due to external force. |
| Ulcer | A type of wound whereby there is disruption or break in the continuity of any lining (skin, mucous membranes, etc.) |
Phases of Wound Healing
Wound healing is defined as the normal body response to surgical or traumatic injury in order to restore normal structure and function. The normal process of wound healing should occur in 4-6 weeks.
There are three phases of wound healing:
| Phase | Processes involved |
|---|---|
| Hemostasis and inflammation | Hemostasis, chemotaxis, epithelial migration |
| Proliferation | Collagen synthesis, matrix synthesis and deposition, angiogenesis |
| Remodelling | Contraction, scar formation, scar remodelling |
| Term | Definition |
|---|---|
| Regeneration | Perfect restoration of pre-existing tissue architecture without scar formation |
| Repair | Wound healing that occurs by proliferation of connective tissue leading to scar formation |
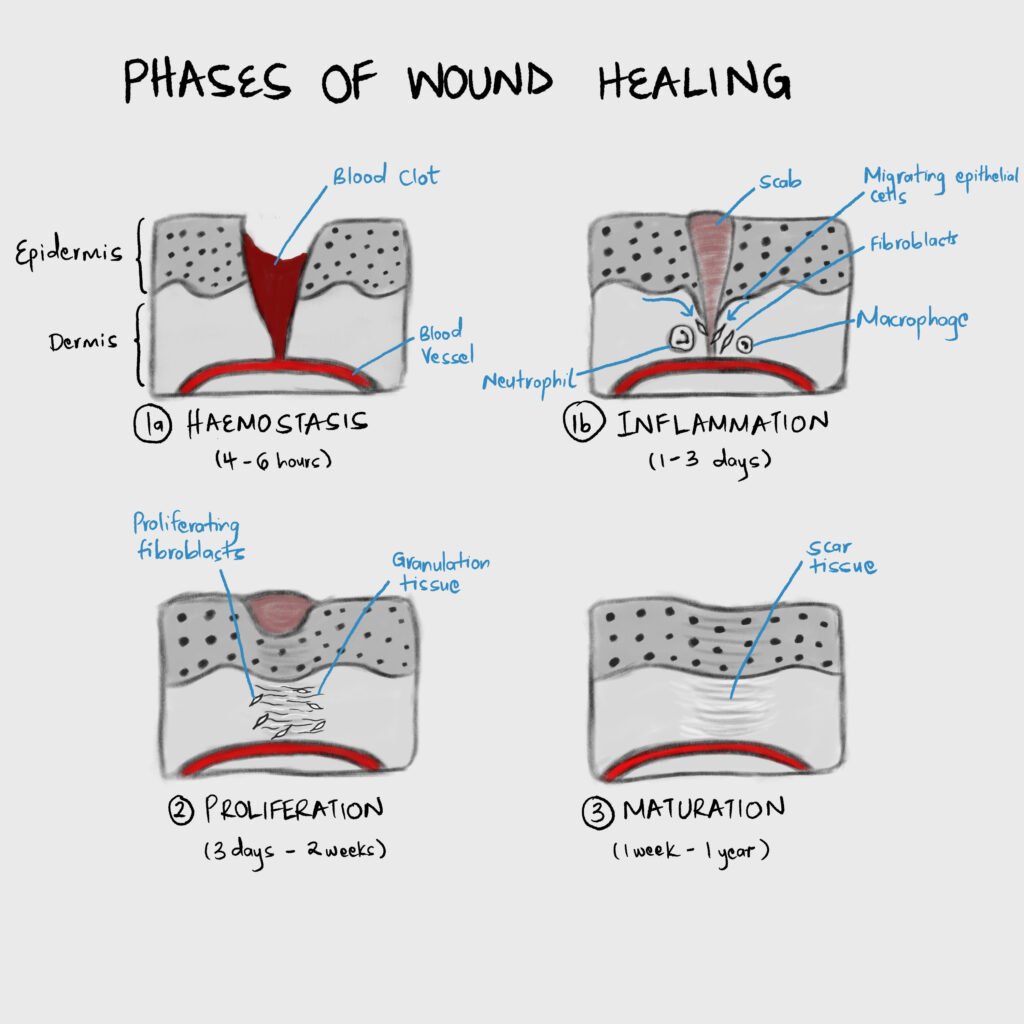
Hemostasis
Damage to tissue causes blood to fill the wound defect. When blood is exposed to collagen and Von Willebrand factor in the extracellular matrix platelets bind, aggregate and degranulate to release preformed granules that activate the coagulation cascade and mediate inflammation. Some of the mediators released by platelets during degranulation include Platelet-derived growth factor (PDGF), Transforming growth factor-B (TGF-B), Platelet-activating factor (PAF), Fibronectin, and Serotonin.
Inflammation
Various cytokines are released which stimulate the movement of cells to the site of inflammation/trauma.
Important Cytokines and Growth Factors
| Molecule | Origin | Effect |
|---|---|---|
| PDGF | Platelets, macrophages, monocytes, smooth muscle cells, endothelial cells | Collagen synthesis, angiogenesis, chemotaxis of fibroblasts, smooth muscle, monocytes, neutrophils |
| FGF | Fibroblasts, endothelial cells, smooth muscle cells, chondrocytes | Angiogenesis by chemotaxis of endothelial cells |
| Transforming Growth Factor-a | Keratinocytes, platelets, macrophages | Chemotaxis of endothelial cells |
| Transforming Growth Factor-B | Platelets, neutrophils, macrophages, lymphocytes, fibroblasts, keratinocytes | Wound matrix synthesis, Regulates inflammation, chemotaxis of neutrophils, macrophages, and lymphocytes |
| Vascular Endothelial Growth Factor (VEGF) | Macrophages, fibroblasts, endothelial cells, keratinocytes | Angiogenesis by mitosis of endothelial cells, pro-inflammatory |
| IL-1 | Macrophages, neutrophils, keratinocytes | Pro-inflammatory, angiogenesis, epithelialization and tissue remodelling |
| IL-4 | Neutrophils | Collagen synthesis |
| IL-6 | Fibroblasts, endothelial cells, keratinocytes | Pro-inflammatory, angiogenesis, epithelialization and tissue remodelling |
Cells involved in the inflammation stage
| Cell | Timeframe | Role | Essential for wound healing |
|---|---|---|---|
| Neutrophil | First to enter the wound within 6 hours due to increased vascular permeability. Numbers peak 24-48 hours from injury | Phagocytosis of bacteria and tissue debris. Also releases cytokines | No |
| Macrophage | Numbers peak within 48-96 hours and remain until the wound is healed | Phagocytosis and wound debridement. Regulates cell proliferation, matrix synthesis, and angiogenesis. Also activates other cells by releasing cytokines. | Yes |
| Lymphocyte | Appears about 5 days post-injury and peaks about 7 days | Not clear. However, decreased number of lymphocytes results in decreased wound strength and collagen content. | Yes |
Proliferation
In proliferation, the continuity of the underlying tissue is re-established through collagen deposition and matrix synthesis, and angiogenesis occurs. This happens over 3 days to 2 weeks post-injury. Characterized by formation of granulation tissue.
| Term | Definition |
|---|---|
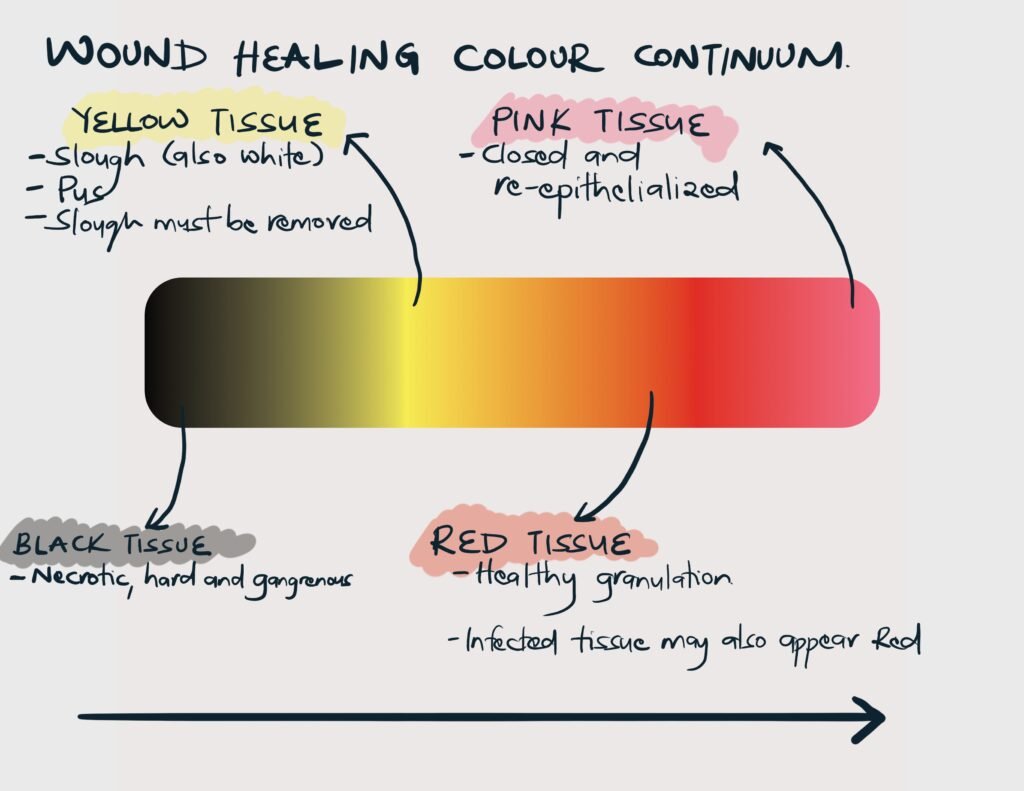
| Granulation tissue | A loose extracellular matrix embedded with fibroblasts, inflammatory cells, and new capillaries. |

Cells involved in the proliferation stage
| Cell | Role | Role |
|---|---|---|
| Fibroblast | Recruited and activated primarily by PDGF, and other cytokines | Matrix synthesis (collagen and glycosaminoglycans) |
| Endothelial cells | Recruited and activated primarily by VEGF, and other cytokines | Migrates from venules near the wound to form new blood vessels (angiogenesis) |
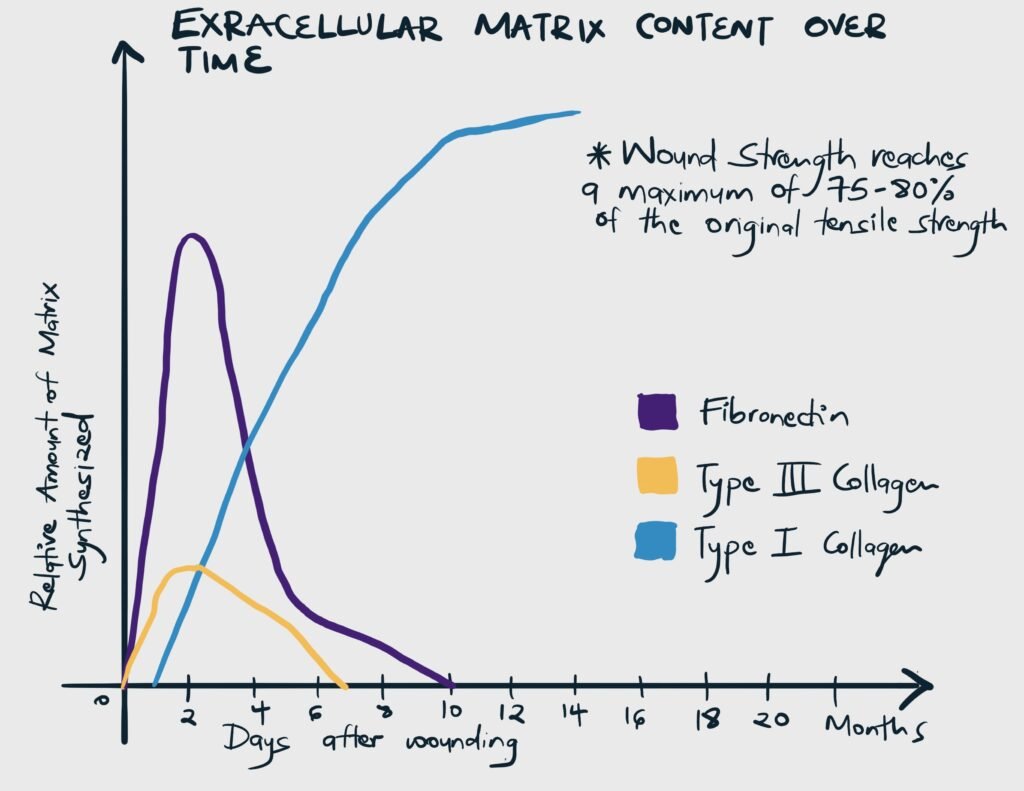
Substances involved in matrix synthesis
| Molecule | Role |
|---|---|
| Type I collagen | Deposition increases throughout the healing process. Responsible for the tensile strength of a scar (strength against tension) |
| Type III Collagen | Deposited early in the healing process and is gradually replaced by type I |
| Glycosaminoglycans (GAGs) | Examples include fibronectin, hyaluronic acid, dermatan, and chondroitin sulfate. They pair with proteins to form proteoglycans. Proteoglycans influence the arrangement and orientation of collagen. |
Remodeling and Scar Formation
Remodelling overlaps with proliferation since collagen reorganization occurs as soon as it is synthesized and deposited.
| Term | Description | Nota bene |
|---|---|---|
| Wound strength | The final tensile strength of the wound is determined by the quantity and quality of collagen deposited and maintained by an appropriate balance of collagen deposition and degradation. | The final strength of injured skin/scar always remains less than that of uninjured skin (on average about 70-80% of uninjured skin) |
| Wound contraction | The inward movement of the wound edge, resulting in reduced granulation tissue required to fill the wound, reduced area requiring re-epithelialization, and reduced scar volume. Primarily mediated by myofibroblasts and is promoted by TGF-B and PDGF. | Occurs to some degree in all wounds about day 5-15 post-injury. It is vital in wounds that heal by secondary intention. Becomes problematic when it impairs cosmesis and function. |
Epithelialization
This is a distinct phase of wound healing whereby the epithelial layer of the skin is restored. It begins within one day of injury and is complete within 48 hours in surgically approximated wounds (but takes longer in wounds left to heal by secondary intention). Basal cells detach from the dermis, enlarge, and migrate across the underlying matrix to cover the defect. Once they defect is bridged the cells rapidly divide and the surface layer is keratinized.
Healing in specific tissue
Healing of Bones
Healing of bones resembles dermal healing with some notable differences and specific terms.
| Phase | Process | Nota bene |
|---|---|---|
| Hematoma and Inflammation | Accumulation of blood, devitalized soft tissue, dead bone and necrotic marrow at the fracture site → Breakdown and liquefaction of non-viable elements at the fracture site → new blood vessels from the adjacent bone grow into the fracture site (analogous to granulation tissue) | Characterized by pain, swelling, and erythema |
| Formation of soft callus (proliferation) | A soft tissue scaffolding forms uniting the fragments and preventing damage to blood vessels | Marked by the end of pain and inflammation |
| Formation of hard callus (maturation) | The soft callus undergoes mineralization and converts to bone | Complete bony union occurs in 2-3 months. The bone is strong enough to bear weight and appears healed on radiograph |
| Remodelling of bone | Resorption of excessive callus and recanalization of the marrow cavity | Remodelling allows physical forces to be correctly transmitted and restores the conture of bone |
Healing of Cartilage
Cartilage has the same phases of wound healing as the dermis. However, it is prone to poor healing since it is relatively avascular. Healing requires the presence of a hypervascular perichondrium and injuries to this may result in permanent defects.
| Depth of injury | Healing | Nota bene |
|---|---|---|
| Superficial cartilagenous injury | Less blood supply to cartilage → less inflammation → slow synthesis of collagen and proteoglycans → slow healing and persistent structural defects | The cauliflower ear is an acquired deformity due to trauma to the ear following boxing, rugby, etc. Trauma shears tissue causing a hematoma to form which disrupts the blood supply to the perichondrium and cartilage of the ear. Cartilage dies and is replaced with fibrosis causing the ear to take on the characteristic appearance. Treatment involved draining the hematoma so that the blood vessels can heal and supply the perichondrium and cartilage. |
| Deep cartilagenous injury | Damage to soft tissue and bone in addition to cartilage exposed blood vessels → follows the typical phases of healing → restoration of structure and function of cartilage |
Healing of tendons and ligaments
Tendon and ligament also have the same phases of healing as the dermis. However, regeneration is slow and results in a fibrous scar at the point of union. Furthermore, collagen fibres orient along the lines of stress. The degree of vascularization is essential in determining healing. Hypovascular tendon and ligaments heal with less motion and more scar than those with better blood supply.
Healing of Nerves
In the CNS, neurons cannot be regenerated. Healing is by proliferation of glial cells which form a glial scar.
Peripheral nerves contain axons, schwann cells and other non-neuronal cells, and extracellular matrix. Injury to nerves occur in 3 degrees (Seddon’s classification of nerve injury), listed below from mild to severe:
| Type of injury | Description | Function loss | Full recovery |
|---|---|---|---|
| Neuropraxia | Focal demyelination with no loss of nerve continuity | Motor disruption. Minimal sensory or autonomic disruption. | Results from transient pressure, and once this pressure is resolved the injury resolves |
| Axonotmesis | Interruption of axon with preserved perineurium and epineurium. | Motor, sensory, and autonomic disruption | Depends on the length of involved segment and how quickly compression is relieved |
| Neurotmesis | Complete transection of the nerve | Motor, sensory, and autonomic disruption | Rare |
For peripheral nerves to recover function:
- Cell bodies of the neuron must survive
- The axon has to regenerate, grow across the transected nerve and reach the distal stump. Phagocytes remove degenerating axons and myelin from the distal stump (Wallerian degeneration). Axons sprout from the proximal stump and probe distal stump and surrounding tissue. Schwann cells ensheath and help remyelinate regenerating axons.
- Regenerating nerve ends have to connect to the appropriate nerve ends or organ targets to create a functional unit
Recovery from surgical re-approximation of divided nerves is better in younger patients, in pure motor/sensory nerves, and in injury where the site is closer to the target organ. The rate of regeneration is 1mm per day so that the more proximal the damage, the more time must elapse before the functional result can be assessed.
Healing of muscle
| Muscle | Healing properties |
|---|---|
| Skeletal muscle | Has some regenerative ability if the cell membrane (sarcolemma) is intact. Severe injury heals by fibrosis. |
| Smooth muscle | Limited regenerative ability. Heals by fibrosis. |
| Cardiac muscle | No regenerative ability. Heals by fibrosis (permanent scar) |
Healing of the gastrointestinal tract
The GIT undergoes the same phases as dermal healing. The serosa and mucosa heal without scar formation. However, during the first week, there is decreased anastomotic strength due to collagenase activity. Collagenolysis precedes collagen syntheis. It begins day 3-5 while collagen synthesis takes several days to begin.
| Layer of the GIT | Role |
|---|---|
| Submucosa | Has the greatest tensile strength and suture-holding ability |
| Serosa | Healing forms a watertight seal. Highlighted by higher leak rates seen in extraperitoneal tissue (esophagus and rectum) |
Full thickness injury of bowel is common in surgery. Repair begins with surgical reapproximation. To maximize healing, anastomosis should:
- Be tension free
- Have adequate blood supply
- Receive good nutrition
- Be free of sepsis
Post-op over-administration of fluid can affect anastomosis by causing third-spacing (edema of the bowel wall) and increasing intra-abdominal pressure which compromises blood flow to the anastomosis.
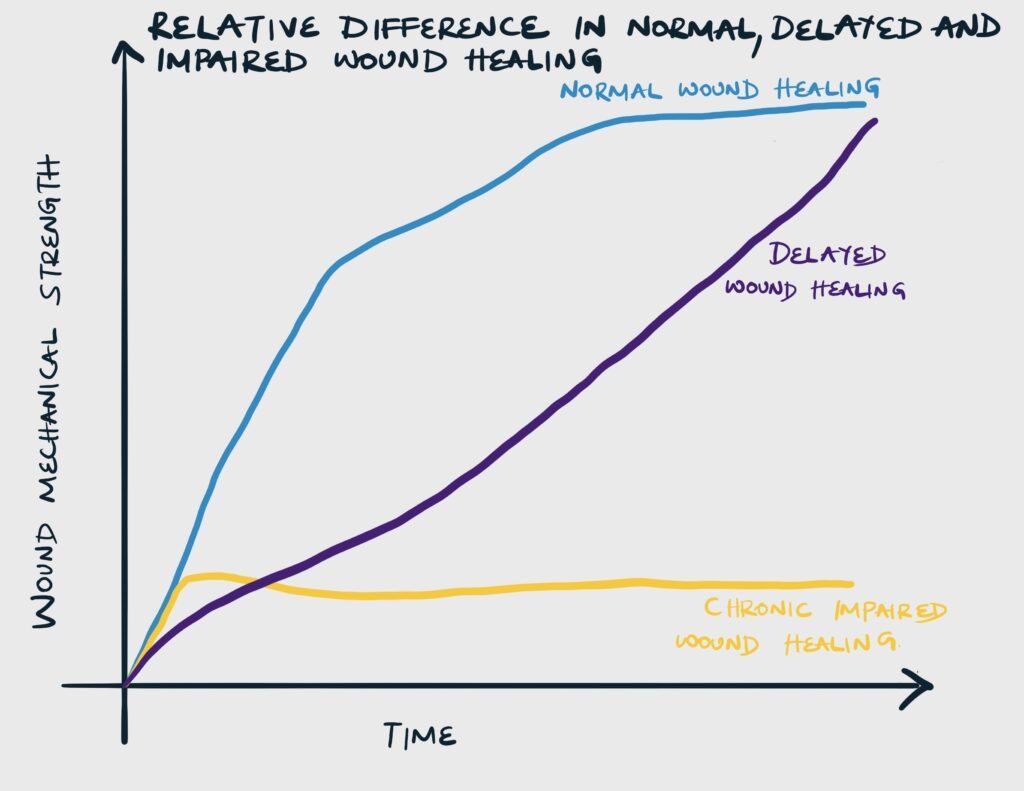
Abnormal wound healing
There are 2 major types of abnormal wound healing: impaired wound healing and delayed wound healing
Impaired vs Delayed wound healing
| Abnormal healing | Description | Cause |
|---|---|---|
| Delayed healing | Though at a slower rate of healing, the wound ultimately achieves mechanical strength as a wound that heals at a normal rate | Reversible underlying pathology, which when corrected allows the wound to heal |
| Impaired healing | The wound never reaches the strength of a wound that has healed normally | Related to immune compromised |
Acute vs Chronic Wound
| Type of wound | Description | Duration | Example |
|---|---|---|---|
| Acute wound | A wound that follows the orderly (continuum) steps of repair to achieve structure and function | Heals within 4-6 weeks | Surgical incision, Laceration e.t.c. |
| Chronic wound | A wound whereby the process of repair has been arrested (at the inflammatory phase) due to multiple reasons, thus failing to achieve the expected structure and function | Takes more than 4-6 weeks to heal | Diabetic ulcer, Decubitus ulcer |
Factors affecting wound healing
Local factors affect wound healing at the level of the wound. Systemic factors are conditions that involve the entire body that affect the ability of the wound to heal.
- Local factors affecting wound healing
- Infection
- Foreign material
- Necrotic or Devitalized tissue
- Hypoxia
- Ischamia
- Ionizing radiation
- Previous trauma
- Repeated trauma
- Venous insufficincy/edema
- Pressure
- Dessication
- Maceration
- Tension on wound edges
- Degree of approximation of wound edges
- Systemic factors affecting wound healing
- Advanced age
- Protein and Energy Malnutrition
- Vitamins and Mineral deficiency
- Metabolic disease e.g. Diabetes, Uremia, Cancer, Obesity
- Immunosuppression e.g. AIDS
- Immunosuppressive medications e.g. Steroids, chemotherapy
- Smoking
- Alcohol
- Cold temperature
- Connective tissue disorders e.g. Ehlers-Danlos, Osteogenesis Imperfecta, Acrodermatitis enteropathica
Infection
Bacteria interfere with wound healing by forming biofilm, producing endotoxin, releasing free radicals and consuming local oxygen. Clincally, an infected wound can be defined as a wound that is draining pus independent of culture results. A more narrow definition is a wound with a bacterial count of 10^5 microorganisms per gram of tissue. The best definition of wound infection, however, is a wound with multiplication of bacteria that overwhelms host defenses and results in wound damage and disruption of the healing process.
To identify wound infection, ask:
- Is the organism cultured normal flora?
- Does the organism typically cause infection of a wound
- Is there inflammation, tissue damage, or signs and symptoms?
- Erythema, pain, swelling, heat fever, and leukocytosis (any make infection more likely)
- Abscess, purulent or abnormal discharge, tissue discoloration or friabiliry, abnormal smell, unexpected wound breakdwon, rolled wound edges, or undermining (3+ make infection likely)
Colonization vs Contamination Vs Infection
| Term | Definition |
|---|---|
| Infection | Bacterial multiplication in a wound with an associated host reaction |
| Colonization | Bacterial multiplication without clinical evidence of infection or impaired healing. May progress to infection. |
| Contamination | Bacteria are present in a wound but are not multiplying and there is no host reaction. They have been introduced from an external source (direct contact, airborne or self-contamination from skin or GI tract) |
Examples of colonization
| Site or prosthesis | Organisms |
|---|---|
| Pressure ulcer | Skin flora (Staphylococcus spp.), Enteric flora (E. coli, Pseudomonas) |
| Skin wound or break | Skin flora (Staphylococcus spp.), Enteric flora (E. coli, Pseudomonas) |
| Upper Respiratory Tract | Mixed enteric flora in patients on antibiotics or those in a healthcare setting for more than 4 days, E. coli, Pseudomonas |
| Endotracheal or Tracheostomy tube | Mixed enteric flora in patients on antibiotics or those in a healthcare setting for more than 4 days, E. coli, Pseudomonas |
| Urinary catheter | Enteric flora (E. coli, Pseudomonas) |
Mechanical barriers, foreign material, and devitalized tissue
Foreign material prolong the inflammatory stage and prevent progression to the proliferative stage of wound healing. These material include necrotic debris (eschar or slough), suture material, retained dressing fibre, prosthesis, dirt, debris, and hematomas. They have to removed for wounds to heal.
Hypoxia
Oxygen is required in the hydroxylation of proline and lysine during collagen synthesis, and cellular respirationwhich are essential to wound healing. Hypoxia occurs in severe blood loss, hypotension, shock, ischemia, and increased tension on the wound.
Local oxygen can be improved by increasing FiO2 during and after elective surgery and by hyperbaric oxygen therapy, especially for patients with diabetes and radiation injury.
Ionizing radiation
Ionizing radiation causes atrophy, fibrosis, and impaired wound healing by causing DNA damage. DNA damage results in cell death and inhibition of mitosis.
Previous trauma
In previous trauma, there is scarring and fibrosis with reduced vascularization of the wound bed. This leads to decreased inflammation and impaired wound healing.
Venous insufficiency
Edema from hydrostatic pressure causes fibrinogen to leak and hemoglobin to extravasate. This causes skin damage and pruritus. Furthermore, fibrinogen polymerizes causing perivascular cuffing and impedes oxygen exchange. Edema alo dilutes bactericidal fatty acids making infection more likely
Advanced age
Older patients are more susceptible to wound dehiscence with less force than young patients. There is delayed epithelialization, slower wound contraction and higher rate of surgical site infections. Older patients also have a higher rate of comorbidities that independently impair wound healing.
Physiological changes associated with aging that inhibit normal wound healing include:
- Increased rate of collagen degradation due to increasd matrix metalloproteinase
- Increase in non-collagen proteins
- Delayed macrophage infiltration and impaired phagocytosis
Nutritional deficiency
| Nutrient | Role |
|---|---|
| Proteins | Hypoproteinemia causes a lack of critical amino acids required for collagen synthesis |
| Vitamin C | Required for hydroxylation of lysine and proline, and collagen cross-linking. Deficiency leads to decreased collagen synthesis and increased collagenolysis |
| Vitamin A | Vitamin A increased collagen production and epidermal growth factor receptors. Supplementation benefits wound healing in non-deficiency individuals, reverses the inhibitory effects of corticosteroids and promotes wound healing in patients with diabetes, chemotherapy, and radiation exposure. |
| Vitamin D | Essential for bone healing |
| Zinc | Multiple enzymes including DNA and RNA polymerase require zinc. Deficiency inhibits cell proliferation and granulation tissue thus impairing early wound healing. Supplementation is only helpful in deficiency individuals. |
Diabetes
Uncontrolled diabetes impairs wound healing by:
- Reducing host immune response and are 5 times more prone to infection
- Impairing angiogenesis
- Decrease collagen synthesis and increased collagen degradation (brittle collagen due to glycosylation)
- Ischemia due to large and small vessel vascular disease
- Renal failure resulting in ischemia
- Repetitive trauma and pressure ulceration due to peripheral neuropathy
Uremia
Uremia decreases collagen deposition and reduces the strength of collagen
Obesity
Obese patients have a higher risk of wound dehiscence, surgical site infection, incisional hernia, seroma, hematoma, fat necrosis and anastomotic leak. Adipose tissue produces adipokines and cytokines which impair cells necessary for wound healing.
Cancer
Impaired wound healing in cancer is often related to malnutrition which can occur due to:
- Cachexia
- Decreased nutrient absorption
- Decreased oral intake
There is also altered metabolism of nutrients:
- Increased glucose utilization
- Increased protein catabolism
- Inability to utilize fat over other sources for energy
Steroids
Steroids impair wound healing by:
- Impairing the inflammatory phase
- Impairing fibroblast proliferation and collagen syntehsis
- Reducing the amount of granulation tissue formed
Prescribing steroids can be delayed until 3-4 days post-operatively to minimize the impact on wound healing.
Chemotherapy
| Drug | Mechanism |
|---|---|
| Antimetabolites | Inhibit DNA and protein synthesis |
| Doxorubicin | Reduces platelets, inflammatory cells, and growth factors |
| Tamoxifen | Decreases cell proliferation. Increasing the dose decreases wound tensile strength |
| Bevacizumab | Impairs angiogenesis |
Smoking
Smoking impairs wound healing by:
- Impairing chemotaxis and cell migration
- Impairing phagocytosis
- Reducing fibroblast migration and proliferation
- Causing hypoxia
Connective tissue disorders
| Disorder | Effect |
|---|---|
| Ehlers-Danlos syndrome | Tissue friability makes suturing difficult |
| Osteogenesis imperfecta | Results in dermal thinning, increased bruising, brittle bones, and ligament and joint laxity |
| Acrodermatitis enteropathica | Inability to absorb zinc reduces cell proliferation and granulation tissue formation |
Excess wound healing
- Pathophysiology of excess scar production during wound healing
- Excessive scarring results from an overabundance of collagen production by fibroblasts in the wound
- There is increased production of:
- Certain isoforms of TGF-B (Primary mediator) – TGFB1 and B2 increase angiogenesis (proliferation) and collagen deposition (maturation); also prevents collagen breakdown by inhibiting metalloproteinases (collagenase) and upregulating tissue inhibitors of metalloproteinase
- Connective tissue growth factor (downstream signaling factor of TGF-B)
- PDGF
- Tissue inhibitors of metalloproteinases
- Decreased production of
- Fibroblast growth factor (FGF)
- Metalloproteinases (collagenases)
- IL-10
- Treatment options for keloids and hypertrophic scars
- First line: Silicon gel
- +/- pressure garment
- +/- steroids
- Second line: Steroids
- +/- silicon
- +/- cryotherapy
- +/- 5-FU
- Third line: Surgery
- +/- steroids
- +/- radiation therapy
- +/- 5-FU
- First line: Silicon gel
| Excess healing | Description |
|---|---|
| Excessive scarring | Excess proliferation of fibroblasts and collagen due to dysregulation of the proliferative and maturation stage |
| Hypertrophic scar | Excess proliferation of fibroblasts and collagen leading to a raised scar that does not grow beyond the boundaries of the original lesion |
| Keloid | Excess proliferation of fibroblasts and collagen in typically small skin injuries leading to a raised scar that grows beyond the wound margins in a “claw-like” appearance |
| Exuberant granulation tissue | Formation of excessive amounts of granulation tissue (”proud flesh”) |
| Desmoid tumor | Fibrous tumors that occur during healing due to abnormal fibroblast proliferation in response to growth factors |
| Contracture | Contraction of wound edges caused by myofibroblasts. Occurs to a greater extent in healing by secondary-intention than primary intention |
Excessive healing in different tissue
| Site | Excess healing |
|---|---|
| Skin | Excessive scarring, keloids, contracture |
| Tendon | Frozen repairs |
| GIT or Urinary Tract | Strictures or stenosis |
| Solid organs | Cirrhosis, pulmonary fibrosis |
| Peritoneum | Adhesive disease |
Keloid vs Hypertrophic scar
| Hypertrophic scar | Keloid | |
|---|---|---|
| Genetics | Not familial | May be familial |
| Race | Not related to race | Black > white |
| Sex | F = M | F > M |
| Cause | Occur across areas of tension and flexor surfaces. | Abnormal fibroblasts within the wound as compared to normal dermis |
| Common site | Flexor surface, but can appear anywhere | Neck, chest, upper back, shoulders and ear lobes |
| Wound margins | Maintained, but rises above the skin level | Outgrows the wound margin |
| Histology | Increased type III collagen with parallel orientation of collagen fibres | Increased type I collagen with randomly oriented fibres |
| Symptoms | Mild pruritus, but relatively asymptomatic | Pain, pruritus, hyperesthesia |
| Response to treatment | Better | Less |
| Spontaneous regression | Often | Rare |
| Prevention | Preventable with appropriate surgical incision and wound care (for trauma and burns) | No preventable |
Classification of Wounds
Tidy vs Untidy wound
| Type of wound | Characteristic | Examples | Healing |
|---|---|---|---|
| Tidy wound | Incised, Clean, no tissue loss | Surgical incision, Stab, Cuts | Primary intention |
| Untidy wounds | Irregular, tissue loss, devitalized tissue, contaminated | Crush, Avulsion/Degloving, Burn | Secondary intention |
Open wounds
The skin has been breached and underlying tissue is exposed
| Wound | Description |
|---|---|
| Clean incision | Tidy, simple, clean cut wound with linear edges |
| Cut | Wound with uneven edges due to a combination of sharp and blunt forces |
| Abrasion | Shallow, irregular wound involving superficial skin layers that results from skin contact with a rough surface or any surface at high speed |
| Laceration | Deeper, tear-like wound, often with irregular edges, typically caused by sharp trauma or focused blunt trauma |
| Avulsion | Tissue is forcibly detached from its normal attachment or insertion |
| Puncture | Small rounded wound that results from thin, pointed objects |
| Penetrating wound | Wound caused by any object that breaks through the skin to underlying tissue or organs |
Closed wounds
The skin is intact, but the underlying tissue has been damaged
| Wound | Description |
|---|---|
| Contusion | Wound caused by direct blunt trauma that causes damage to small vessels and capillaries producing bruising (skin discolouration) in subcutaneous tissue |
| Hematoma | Wound caused by trauma that damages small vessels and capillaries allowing blood to collect in a potential space |
Mechanism of injury
| Mechanism | Examples |
|---|---|
| Mechanical wound | Abrasion, puncture, incision, cut, crush, tear, bite wound, gunshot wound |
| Chemical wound | Due to acids and alkali |
| Radiation wound | Due to radiation exposure |
| Thermal destruction | Burn or frostbite |
Primary, Secondary, and Tertiary intention
Types of wound healing
| Type of healing | Description | Example of wound |
|---|---|---|
| First intention | Wound edges are approximated by suturing, staples, or adhesive | Surgical wound, clean incision |
| Secondary intention | The wound heals slowly by granulation tissue and scar formation and closes by re-epithelialization | Traumatic wound, highly contaminated wound, extensive soft tissue loss |
| Tertiary intention (Delayed primary closure) | The wound is treated by repeated debridement and finally approximated | Traumatic wound with high infection risk |
Healing by primary vs secondary intention
| Primary intention | Secondary intention | |
|---|---|---|
| Tissue deficit | Smaller | Larger |
| Mechanism of healing | Epithelial regeneration | Granulation tissue. Pale, avascular scar formation |
| Myofibroblast contraction | Minimal | Marked |
| Fibrin clot | Smaller | Larger |
| Inflammation | Less intense | More intense |
| Secondary inflammation mediated damage | Less potential | More potential |
| Granulation tissue | Small amounts | Larger amounts |
| Scar tissue | Smaller mass | Greater mass |
| Exudate | Less exudate | More exudate |
| Necrotic debris | Less | More |
Ulcer
An ulcer is a chronic wound that is defined as a break in the continuity of the covering epithelium in either skin or mucous membranes due to molecular death. The most common ulcers are venous, arterial, or mixed ulcers. These three account for 70% of all ulcers while 50% are caused by venous stasis alone.
Location of ulcers based on etiology
| Ulcer | Description | Common Location |
|---|---|---|
| Neuropathic and Traumatic ulcers | Due to loss of sensation → inability to withdraw from painful stimulus or trauma → repeated trauma → ulceration | Pressure bearing regions |
| Venous (Varicose) ulcers | Due to hypoxia. Painful, easily recur and persist for many years. | Medial and lateral malleoli |
| Arterial ulcer | Due to ischemia caused by atherosclerosis or peripheral arteries. Appear punched out and well demarcated with round shape and pale, non-granulating, often necrotic base | Dorsum of the toes, dorsum of the foot, and in-between toes |
| Diabetic ulcer | A mixed ulcer due to ischemia + neuropathic changes + systemic metabolic dysfunction + immune dysfunction causing ulceration and impaired healing | No particular site since any ulcer with imaired healing (neuropathic/arterial/traumatic/varicose) due to diabetes is termed a diabetic ulcer. However bullae tend to appear in the nape and back. |
| Decubitus (Pressure) ulcers | Mechanical pressure compresses arterioles and venules causing ischemia and hypoxia | Back of head, shoulder, elbow, hip, sacrum, ischial tuberosity, greater trochanter, medial and lateral condyles, malleoli, and heels |
- Features suggestive of malignancy in ulcers
- Margins: Irregular with nodules
- Egde: Everted edges
- Floor: red and bleeds easily on palpation
- Surrounding skin: inflammed and indurated (hard)
- Investigations for patients with chronic ulcers
- CBC: look for anemia
- ESR: monitor for infection
- RBS and HbA1C: for glycemic control
- U/E/Cs: for uremia
- VDRL: for syphillis
- HIV: for HIV
- Chest X-ray: for TB
- EKG: to rule out IHD if atherosclerosis is suspected
- Local smear for culture
- X-ray of the affected part
- 4 quadrant edge biopsy
- Stigmata of Tuberculosis to look out for in a patient with an ulcer
- Phlyctenular conjunctivitis
- Matted Lymphadenopathy
- Scars and Sinuses in the neck
- Stigmata of Leprosy to look out for in a patient with an ulcer
- Hypopigmented, anesthetic patches
- Thickened ulnar posterio tibial, and great auricular nerves
- Trophic ulcers (pressure ulcer)
- Deformed phalanges
- Leonine facies (due to collapse of the nasal bridge and lateral 1/3 of eyebrows)
Diabetic ulcer
- 4 ways in which diabetes impairs healing of ulcers
- Hyperglycemia promotes the proliferation of bacteria and glycosylates collagen making it brittle
- Decreases blood supply to the ulcer due to small and large vessel disease
- Ulcer is prone to repeated, unnoticed trauma as a result of neuropathy
- Deficient fibroblast reaction
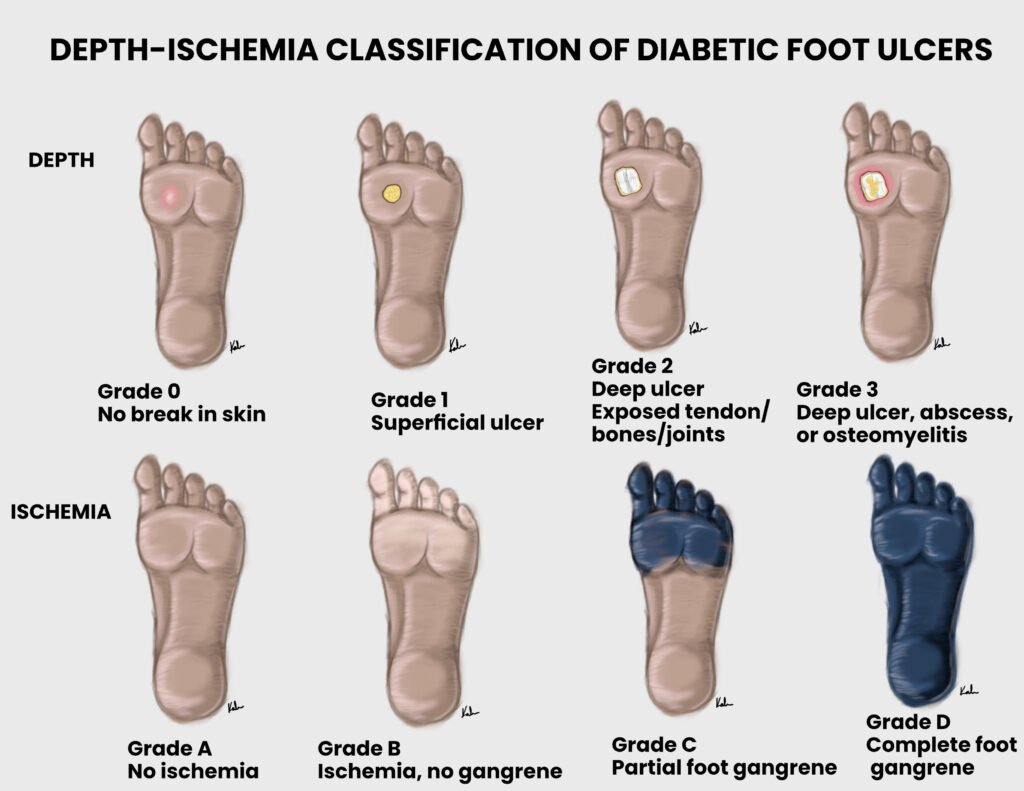
Wagner Grading of diabetic foot ulcers
| Grade 0 | Intact skin |
|---|---|
| Grade I | Superficial ulcer |
| Grade II | Deep ulcer |
| Grade III | Ulcer with abscess or bone involvement or osteomyelitis |
| Grade IV | Forefoot gangrene (localized) |
| Grade V | Full foot gangrene (extensive) |
Decubitus (Pressure) ulcers
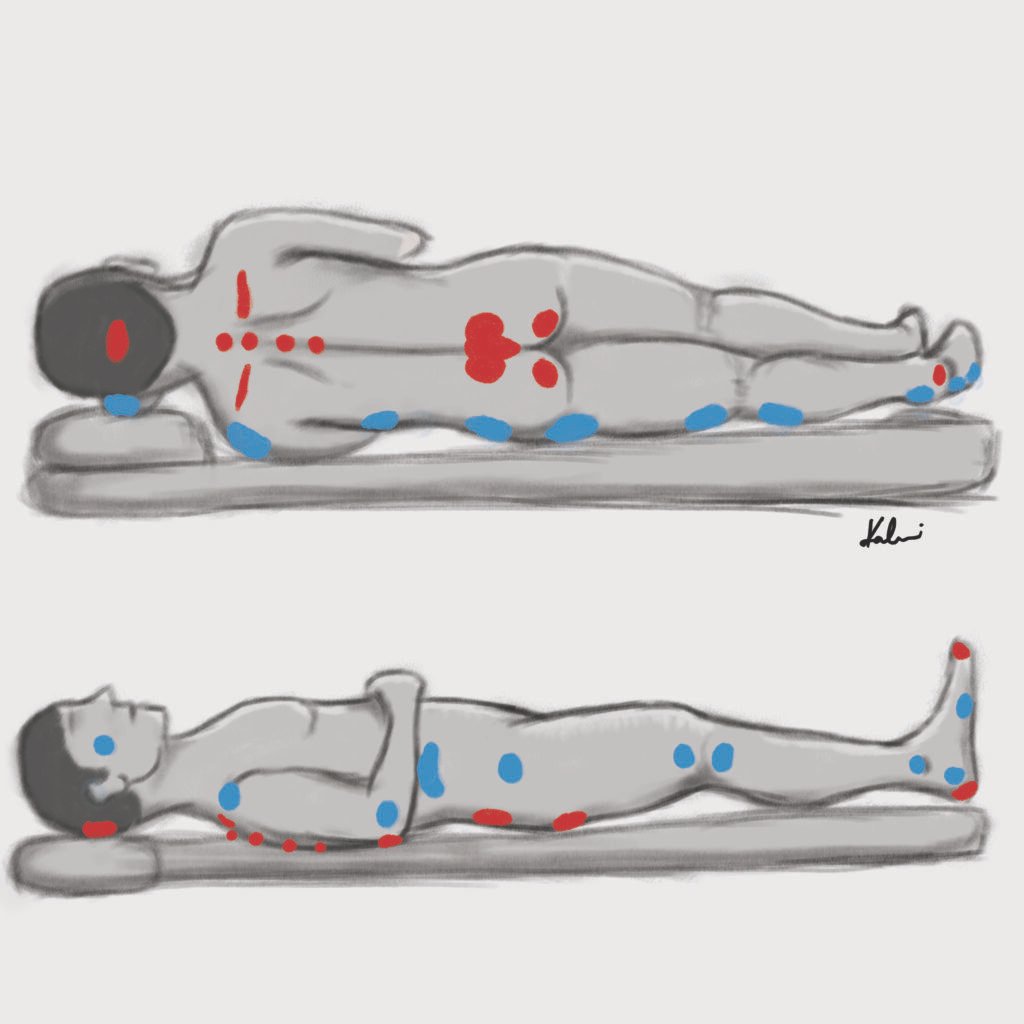
Staging of decubitus ulcers
| Stage | Description |
|---|---|
| Stage I | Intact skin. Change in color, consistency, or temperature |
| Stage II | Partial-thickness loss of skin involving the epidermis and dermis |
| Stage III | Full-thickness skin loss including subcutaneous tissue but not fascia |
| Stage IV | Damage to muscle, bone, and other supporting tissue, may have undermining of tissue |
- Risk factors for development of pressure ulcers
- Sensory deficits
- Moisture
- Immobility
- Inactivity
- Malnutrition
- Friction and shear
- Prevention of pressure ulcers
- Reduce external pressure
- Reposition every 2 hours
- Pillows or thick padding areas at risk
- Keep the skin clean and dry
- Adequate pain relief to allow for activity and mobility
- Manage systemic conditions that place the patient at risk of developing pressure ulcers
- Reduce external pressure
Gunshot Wound (GSW)
The higher the projectile velocity of a missile, the greater the damage. Low velocity missiles from pistols drill only narrow tracks with little damage around them. in addition to causing extensive cavitation, high velocity missiles form a partial vacuum in their path that sucks in debris. Missile wounds may take curious paths. They may be deflected by bone, or be influenced by the position of the patient at the time of injury. A multi-disciplinary care team is required for GSW. GSW should not be closed primarily. Delayed primary closure after initial debridement, or healing by secondary intention is preferred. Bullets and fragments are removed only where indicated.
Types of injury
| Type of injury | Weapon | Projectile velocity |
|---|---|---|
| Low velocity | Handgun, some rifles | < 350 m/s (1200 fps) |
| Medium velocity | Shotgun: potential for massive soft tissue destruction. The wad may stay in the wound and form a nidus of infection | 350 – 650 m/s (1200 – 2100 fps) |
| High velocity | Military or Hunting rifles | > 600 m/s (>2000 fps) |
- Complications of GSW
- Compartment syndrome: common after high velocity wounds. More common with proximal fractures of the forearm
- Vascular injury: findings include pulsatile bleeding, absent pulse, bruit, thrill. ABI and angiography can be performed if there is concern.
- Spinal injury: GSW is the 3rd most common cause of spinal injury. Cervical spine GSW can be associated with airway compromise (84%)
- Infection: GSW tracts are non-sterile. 24 hours IV antibiotics (1st gen cephalosporins) for low-velocity injuries (Gustillo I/II) and 72 hours IV antibiotics (1st gen cephalosporin + gentamicin) for high-velocity injuries (Gustillo III)
- Fractures: Low velocity injuries can be treated as Gustilo I/II while high velocity injuries can be treated as Gustilo III. GSW has increased comminution and greater soft-tissue stripping and bone loss.
- Retained projectiles and fragments: retained fragments can be left in situ. Indications for removal include: intra-articular, intra-vascular, subcutaneous, lead toxicity, peri-spinal and peri-neural
- Compartment syndrome
- Common after high velocity wounds due to soft-tissue trauma/bleeding/oedema
- More common with proximal fractures of the forearm
- Vascular injury and hemorrhage
- Findings include pulsatile bleeding, absent pulse, bruit, thrill
- Damage control surgery e.g. shunting can be performed
- ABI and Angiography can be performed if there is concern
- Peripheral nerve injury
- Majority of nerve dysfunction is neuropraxia, particularly in low velocity wounds
- Life-saving interventions in GSW
- Hemorrhage control and resuscitation
- Chest tubes (even bilateral chest tubes)
- Laparotomy
Classification Surgical Wounds
Colonized body cavities = respiratory, alimentary,, genital, or urinary tracts
| Wound | Description | Example | Infective rate | Need for prophylaxis |
|---|---|---|---|---|
| Clean wound | Elective wound. Primarily closed withour drain. No opening of colonized body cavities. No break in sterile technique. | Hernioplasty, Excisions, Thyroidectomy, Brain surgery, Joint surgery, arterial and venous surgery, heart surgery | 1-5% | No |
| Clean contaminated wound | Elective wound. Controlled opening of normally colonized body cavities. Minimal spillage. No break in the sterile technique. | Appendicectomy, Gastrojejunostomy, Pancreaticobiliary surgeries, Lung resection, Cholecystectomy, Gastrectomy, Prostatectomy | 3-11% | Prophylaxis may be required |
| Contaminated wound | Acute, non-purulent inflammation. Break in sterile technique or spillage from hollow organs. Open, fresh accidental wound. | Penetrating trauma < 4h from injury, Chronic open wound, acute abdomen, removal of acute appendicitis, open cardiac massage during a case | 10-17% | Prophylactic antibiotics required – 1 hour prior to incision, 2nd and 3rd dose q8h |
| Dirty wound | Purulent abscess. Traumatic wound from a dirty source with retained, devitalized tissue. Surgical wound involving existing infection or free perforation. | Penetrating trauma > 4 hours from injury, abscess, perforated viscus with peritonitis, fecal peritonitis | 27-40% | Treatment required instead of prophylaxis |
Assessment of a wound
TIME mneomnic for assessment of wounds
Tissue: presence of granulation or hypergranulation tissue, devitalized or necrotic tissue, and surrounding tissue
Inflammation or infection: areas within or surrounding the wound site that may indicate the presence of infection or inflammation
Moisture: moisture balance and whether the wound is dry or macerated
Edge of the wound: assess for re-epithelialization vs non-advancing ages vs epibole. Also assess blood supply to the edges of the wound.
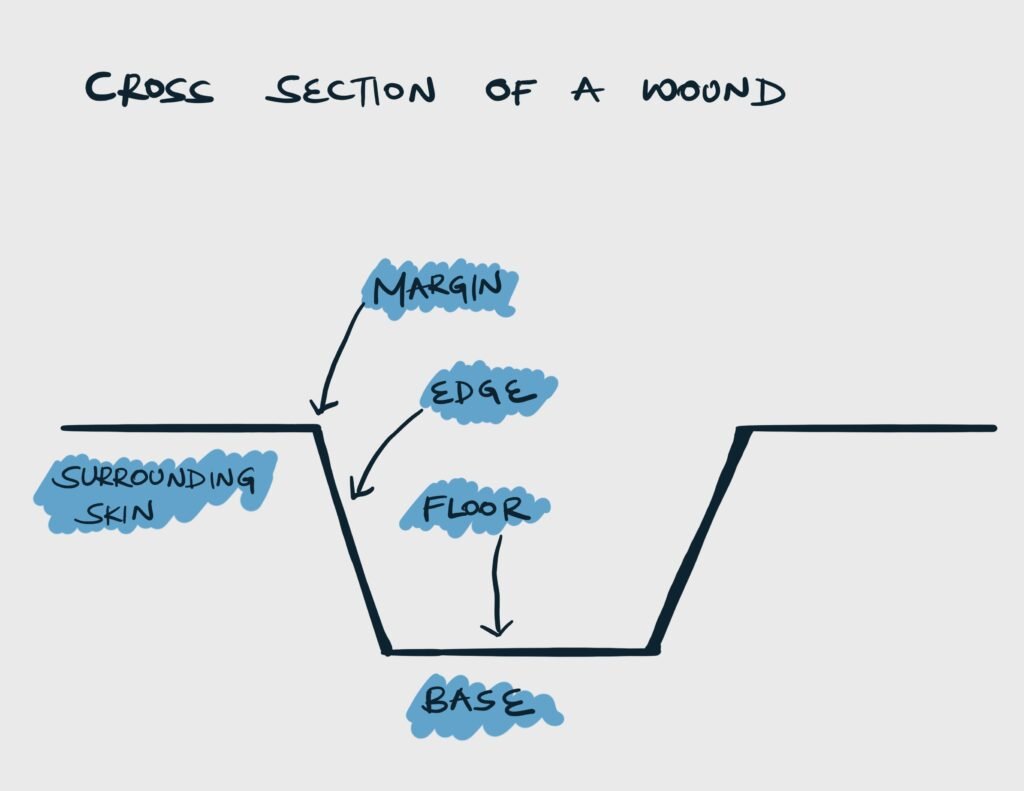
Parts of a wound
| Part | Definition | Description |
|---|---|---|
| Marging | A line that represents the junction between instact skin and the ulcer | Rounded or oval. Regular or Irregular. Well-defined or ill-defined. |
| Edge | The block of tissue that connects the margin and the floor of the ulcer | Sloping, undermined, punched out, raised and beaded, or everted |
| Floor | Visible part overlying the base | Contanins discharge, granulation tissue (red/pink) or slough (yellow) |
| Base | Tissue on which the ulcer rests on | Bone, tendons, or muscle |
Size
Wound size should be measured and documented on first presentation and regularly after that. Dimensions include length, width and depth of tissue planes. Wounds can be measured using a tape, ruler, scalpel handle or gloved finger.
Margin
| Margin | Inference |
|---|---|
| Ill-defined irregular margins | Growing or spreading ulcer |
| Well-defined regular white margin | Non-healing ulcer |
| Well-defined regular margin with white, blue, and red zones | Healing ulcer |
| Nodules on margin | Rodent ulcer (BCC) |
Edges
| Edges | Inference |
|---|---|
| Sloping edge | Healing ulcer, venous ulcer |
| Punched out edges | Aretrial and Gummatus ulcer |
| Raised and everted edges | Malignancy |
| Undermined edges | Tuberculous ulcer, Amoebic ulcer in the intestines |
| Raised non-everted edges | Basal cell carcinoma |
Epibole: a rolled or curled-under wound edge where the epithelial layer fails to advance. The upper epidermal edge moves over the lower edge causing epithelialization down the wound edge rather than across the base. They must be resected or debrided in order for epithelialization to continue.
Floor
| Floor content | Inference |
|---|---|
| Pink with tiny red granules or nodules (capillary “buds”) | Healthy granulation |
| Pale flat granulation, “heaped up” appearance | Unhealthy granulation, exuberant granulation |
| Scanty serous discharge | Can be seen in healthy granulation |
| Yellow, white, or grey slough | Infection has not been controlled and granulation is yet to begin |
| Serosanguinous purulent discharge | Infected ulcer |
| Dry, hard, or leathery, and black | Eschar |
Surrounding skin
Inspect the surrounding skin for cellulitis, maceration, and other peri-wound skin abnormalities e.g. scars, deformities, rashes, and varicosities.
Management of wounds
The goals of wound care include:
- Closure of the wound
- Prevention of infection
- Provision of stable and adequate coverage
- Minimization of the defect
- Maximization of function
The steps in management of wound usually involve assessment → preparation → repair → follow-up
- Wound assessment
- Life-threatening and limb-threatening injuries
- Location, age, depth, width, length of wound, and extent of devitalized tissue
- Degree of contamination (clean or dirty wound) and Sx of infection
- Neurovascular and musculoskeletal injuries
- Radiographs for fractures
- Pulsatile bleeding (arterial) or dark oozing (venous). Assess circulation distal to wound
- Nerve integrity and function
- Preparation
- Tetanus prophylaxis
- Antibiotics as indicated
- Open fractures
- Situations of infection
- Local anaesthetic (Lidocaine or Bupivacaine with or without epinephrine)
- Exploration to examine underlying structures
- Irrigation of wound
- Normal saline (50-100mL per centimeter of wound length)
- High pressure or pulsatile irrigation is effective in remove foreign bodies and reduces the need for debridement
- Cleaning with soap and water
- Povidone-iodine or Chlorhexidine for wounds with risk of viral transmission. May impair wound healing by damaging neutrophils and macrophages
- Hemostasis
- Evacuate hematoma
- Control bleeding with ligature or cautery
- Mechanical hemostasis with local pressure, packing, or torniquet
- Pharmacological hemostasis with Tranexamic acid (systemic) or Epinephrine (local)
- Fluids and Blood products for resuscitation if shock
- Debridement of non-viable tissue
- Mechanical debridement, surgical debridement, biologic debridement, enzymatic debridement, autolytic
- Repair
- Deep fascial layer with absorbable suture
- Superficial layer properlly aligned and non-absorbable suture (monofilament)/staples/dermal glue
- Primary wound closure: close within 6-8 hours of extremity injury and 10—12 hours for injury of the scalp and face (bacteria require 6-8 hours to reach 10^5/gram of tissue, the level necessary for infection)
- Clean wound with low infection risk whose edges can be approximated without tension
- Secondary wound closure: leave the wound to heal by secondary intention via granulation tissue (w/o approximating wound edges)
- Infected wounds (SSI)
- Wound at high risk of infection (with foreign body implanted)
- Bite wounds
- Wounds older than the time frame within which primarily closure can be safely performed
- Large wounds that cannot be approximated without tension
- Delayed primary closure: close wound after secondary intention has began
- Contaminated wounds left to heal by secondary intention with no signs of infection after 3-5 days
- Clean wounds with healthy edges present after the time frame within which primary closure can be safely performed
- Non-primary wound closure
- Skin grafts
- Skin flaps
- Follow-up
- Monitor for signs of infeciton
- Remove suture early (4-5 days for face) or 7-10 days for other parts of skin
Wound preparation
Types of injuries and considerations
| Type of injury | Nota bene |
|---|---|
| Animal bite | Cat bites are deep and are more likely to enter joint spaces and result in infection. Aggressively clean and treat with antibiotics. |
| Human bite | High risk of infection, especially those involving the hands. Aggressively clean, treat with antibiotics, and do not close primarily |
| Crush injury e.g. hippo bite, car tyre | Results in deep tissue injury with skin relatively intact. Rule out deeper injury |
| Dirty wound e.g. firm injury | Aggressive debridement and washout with removal of foreign material |
Tetanus prone wounds
| Wound characteristic | Tetanus prone |
|---|---|
| Time since injury < 6 hours | No |
| Time since injury > 6 hours | Yes |
| Depth < 1cm | No |
| Depth > 1cm | Yes |
| Crush, burn, gunshot, frostbite, penetrating injury through clothing | Yes |
| Presence of necrotic or devitalized tissue | Yes |
| Foreign material (dirt or grass) present | Yes |
Determining appropriate tetanus treatment
| Year since immunization | Wound characteristic | Tetanus treatment |
|---|---|---|
| < 5 years | Clean or tetanus prone | None |
| 5-10 years | Clean | None |
| Tetanus prone | Tetanus toxoid 0.5 mL IM (booster) | |
| > 10 years | Clean or tetanus prone | Tetanus toxoid 0.5 mL IM (booster |
| Never immunized | Clean | Full tetanus immunization regimen: Tetanus toxoid 0.5 mL IM 0 day, 4 weeks, and 6-12 months |
| Tetanus prone | Full tetanus immunization regimen: Tetanus toxoid 0.5 mL IM 0 day, 4 weeks, and 6-12 months. Also give human tetanus immunoglobulin 250 IU, deep iM but not in the same area as the toxoid injection |
Repair
- When closing deep tissue layers:
- Deep fascial layers or deep dermal layers should be closed since they contribute to the structural integrity of the wound
- Closed suction drains can be used to decrease dead space
- Suturing fat adds no benefit to wound strength or structure, so fat should not be closed
Absorbable vs non-absorbable suture
| Absorbable | Non-absorbable | |
|---|---|---|
| Broken down by the body | Yes | No |
| Tissue reactivity | More | Less with timely removal |
| Scarring | Increased risk | Less risk |
| Selection | Under the skin, within the oral mucosa, in children, in patients unlikely to return for suture removal | Skin closure, vascular repair, when permanent reinforcement is needed, history of keloid formation |
Monofilament vs braided suture
| Monofilament | Braided | |
|---|---|---|
| Strands | Single strand | Multiple strands twisted together |
| Friction and trauma to tissue | Less | More |
| Risk of infection | Reduced | Increased |
| Handling and secure knot tying | Difficult since it has ‘memory’ | Easier |
Suture examples and characteristics
| Suture | Characteristic | Complete absorption |
|---|---|---|
| Chromic gut | Braided, absorbable | 10-14 days |
| Polyglactin 910 (Vicryl) | Braided, absorbable | 2 months |
| Dexon | Braided, absorbable | 2 months |
| Polysorb | Braided, absorbable | 2 months |
| Poliglecaprone 25 (Monocryl) | Monofilament, absorbable | 3 months |
| Polydioxanone (PDS) | Monofilament, absorbable | 6 months |
| Biosyn | Monofilament, absorbable | 6 months |
| Maxon | Monofilament, absorbable | 6 months |
| Silk | Braided, non-absorbable | Permanent |
| Prolene | Monofilament, non-absorbable | Permanent |
| Nylon | Monofilament, non-absorbable | Permanent |
Suture size
| Size | Use |
|---|---|
| 7-0 and smaller | Ophthalmology, microsurgery |
| 6-0 | Face, blood vessels, ducts |
| 5-0 | Face, neck, blood vessels, ducts |
| 4-0 | Mucosa, neck, hands, limbs, tendon, blood vessels |
| 3-0 | Limbs, trunk, gut, blood vessels |
| 2-0 | Trunk, fascia, viscera, blood vessels |
| 0 and larger | Abdominal wall closure, fascia, drain sites, orthopedic surgery |
Continuos (”running”) stitch: a series of stitches connected in line and only a single suture is use. Variations include simple continuous and locking continuous stitches
- Advantages of continuous stitch
- Quick
- Less suture material used
- Less foreign body in the wound
- Evenly distributed tension
- Disadvantages of continuous stitch
- Too much tension leading to wound ischemia
- Fluid and bacteria can travel along the suture and spread infection
- Entire suture must be removed in case of wound infection
Interrupted stitch: each individual suture is placed, tied, and cut separately from any others. Variations include simple, vertical mattress, horizontal mattress, and many others
- Advantages of interrupted stitch
- Very secure closure (if one stitch fails the others can hold the wound togethre)
- Bacteria are less likely to move along the suture line
- Can remove individual stitches in the event of wound infection
- Disadvantages of interrupted stitch
- Time consuming
- More foreign body in the wound
- Uses more suture
Staples: staples offer rapid closure with less precise tissue approximation. Placing sutures in the dermis can help improve approximation
Skin glue and adhesives: skin glue is ideal in areas of low wound tension (face and neck). It has equivalent results and complication rates as traditional sutures and is more comfortable for patients.
Tape: tape is easy to apply and comfortable. It leaves no skin marks. However, it can easily be displaced with moisture/drainage and can create inverted edges.
Follow-up
The wound should be monitored for signs of infection and sutures/staples left in place until the healing process has created enough strength.
Recommendations for removing sutures
| Location of closure | Number of days for removal |
|---|---|
| Face | 3-5 |
| Scalp | 5-7 |
| Extremity (low-tension closure) | 6-10 |
| Extremity (high-tension closure) | 10-14 |
| Abdomen | 6-12 |
| Chest and back | 6-12 |
Management of chronic wounds
The goal of managing chronic wound is to identify and address the conditions that impair wound healing. By correcting these condition, the wound behaves like an acute wound and can be managed as such through closure, skin graft, or flap.
In addition to correcting these condition, supportive management (proper wound care and dressing) aims to create a wound bed that is sufficient for epithelialization or support a skin graft. This can be done by:
- Reducing infection or colonization
- Maintaining appropriate moisture levels
- Improving oxygen tension in the tissue
- Promoting angiogenesis
Dressing
| Category of Dressing | Characteristic | Use | Example |
|---|---|---|---|
| Non-adherent dressing | Fine mesh gauze with coating (to prevent adherence) | To protect wounds and underlying tissue, maintain moisture | Vaseline gauze, Xeroform, Mepitel, Telfa, Tulle gras |
| Absorptive dressing | |||
| Gauze | Wide mesh gauze | To remove exudate, prevent maceration, and debride (wet-to-dry application) | Wide mesh gauze |
| Foams | Hydrophobic foam sheet | To protect wounds and absorb exudate | Allevyn, Curfoam |
| Occlusive dressing | |||
| Non-biologic | Made of polyurethane, cellulose, among others | To insulate, retain moisture, protect the wound and decrease bacterial contamination | Tegaderm, Opsite, Duoderm, Melgisorb |
| Biologic | Made from cadaver skin, pig skin, and human amniotic sac | To insulate, retain moisture, protect the wound and decrease bacterial contamination | Cadaveric skin, Bovine xenograft, Integra, Alloderm |
| Creams, Ointments, and Solutions | |||
| Antibacterial solution | A variety exist | Use on infected wounds | Acetic acid (gram negatives, Pseudomonas), Dakin’s solution (broad spectrum), Iodine-containing solution (broad spectrum, antifungal), Silve-containig solution (broad spectrum, antifungal) |
| Antibacterial ointments | A variety exist | Use on infected wounds, provides occlusion and soothes the wound | Bacitracin (gram positive), Neomycin (gram negative), polymyxin B (gram negative), Neomycin, Triple antibiotic ointment (bacitracin, neomycin, polymyxin B) |
| Enzymatic | A variety exist | To remove necrotic tissue | Collagenase, papain |
Hyperbaric Oxygen (HBO)
HBO therapy involves inhaling 100% O2 at 1.9-2.5 atm of pressure allowing tissue oxygen tension to be ten times normal. It can be given in an enclosed chamber or through a face mask. The oxygen is used in metabolism, induces the synthesis of nitric oxide synthase, and promotes angiogenesis.
HBO is useful in diabetic ischemic ulcers (reduces the amputation rates)
Negative Pressure Wound Therapy (Wound VAC)
Wound VAC applies negative pressure to the wound to remove chronic edema, increase local blood flow and stimulate the proliferation of granulation tissue. It may be used on acute or chronic wounds.
Unna Boot
An unna boot is made by wrapping the leg in gauze impregnated with zinc, glycerin, calamine, or a mixture. It is used to treat venous leg ulcers and lymphedema-related ulcers. The hardened gauze restricts the outward movement of the calf mucles and promotes edema resorption and venous return.
Complications of wounds
- Early complications of wounds
- Local infection
- Sepsis
- Shock
- Intermediate complications of wounds
- Hematoma
- Seroma
- Local infection
- Late complications of wounds
- Hypertrophic scar
- Keloid
- Contracture
- Marjolin ulcer
- Psychological problems
Wound dehiscence
Wound dehiscence is separation of wound along incision line. Fascial dehiscence is the separation of a fascial closure following abdominal surgery. ****Risk can be reduced by good surgical technique and avoidance of heavy lifting for 4-6 weeks after laparotomy.
Can lead to evisceration. Diagnosis is clinical.
Fascial dehiscence
| Fascial dehiscence | Description |
|---|---|
| Partial fascial dehiscence | Partial failure of sutures e.g. deep sutures have failed but superficial sutures are still intact (or vice versa) |
| Complete fascial dehiscence | All suture layers have failed |
- Risk factors for fascial dehiscenceMost are factors that impair normal wound healing
- Surgical site infection
- Increased intra-abdominal pressure
- Distension
- Valsava
- Chronic cough
- Malnutrition
- Diabetes
- Malignancy
- HIV/AIDS
- Trauma to the incision site
- Emergency surgery
- Anaemia
- Advanced age
- Signs and symptoms
- Seeping of serosanguineous (”salmon-colored”) fluid
- “Popping” or “Tearing” sensation
- Buldge during valsava
- Evisceration in case of complete dehiscence.
- Bleeding
- Pain
- Inflammation
- Rarely fever
- Prophylaxis
- Retention sutures at the time of initial abdominal closure
- Malnourished or hypoalbuminemic
- Immunocompromised
- Massive contaminaiton
- Previous fascial defect or for patients expected to have increased tension on the wound
- Retention sutures at the time of initial abdominal closure
- Treatment
- Place temporary support (sterile tape, mesh)
- Restrict movement until resuturing can be done (under sterile conditions, with debridement and re-approximation of edges)
- Complications of wound dehiscence
- Wound evisceration
- Incisional hernia
- Sepsis
Wound evisceration
Wound evisceration is separation of wound along incision line along with expulsion of internal organs. A complication of wound dehiscence. Diagnosis is clinical. This is a surgical emergency.
- Cause of wound evisceration
- Undiagnosed, unaddressed or poorly addressed wound dehiscence
- Signs and symptoms
- Internal organs are visible…
- Treatment
- Place moist sterile dressing over the evisceration.
- Restrict movement.
- Emergent repair
- Do not attempt to manipulate expulsion until the patient is in theatre
