Overview
Trauma is the leading cause of death and disability in pts < 40yo, and is the third most common cause of death overall. The formula patient + mechanism = injury is key in assessing and managing trauma patients .

The philosophy of ATLS is to treat lethal injuries first, reassess, then treat again with its priorities being salvaging life, then limb, then total body function if possible. A deductive approach for classical covert injuries can be done initially to screen at-risk patients before clinical signs swt in. A look everywhere approach is essential, especially in unconscious patients, to exclude further injuries once life-saving assessment and management is achieved. A focused-exclusion approach is mandatory for life-threatening injuries.
The sequence: Primary survey → resuscitation → Secondary survery → Definitive care → Tertiary care
- Immediately life threatening conditions
- Airway
- Airway obstruction
- Breathing
- Tension pneumothorax
- Open pneumothorax
- Massive hemothorax
- Flail chest
- Circulation
- Pericardial tamponade
- Airway
- Potentially life threatening conditions
- Breathing
- Tracheobronchial tree disruption
- Diaphragmatic injuries
- Pulmonary contusion
- Circulation
- Thoracic aortic disruption
- Blunt myocardial injury
- Esophageal injuries
- Breathing
- Signs of life
- Pupillary light reflex
- Spontaneous ventilation
- Palpable carotid pulse
- Measurable blood pressure
- Spontaneous extremity movement
- Cardiac electrical activity
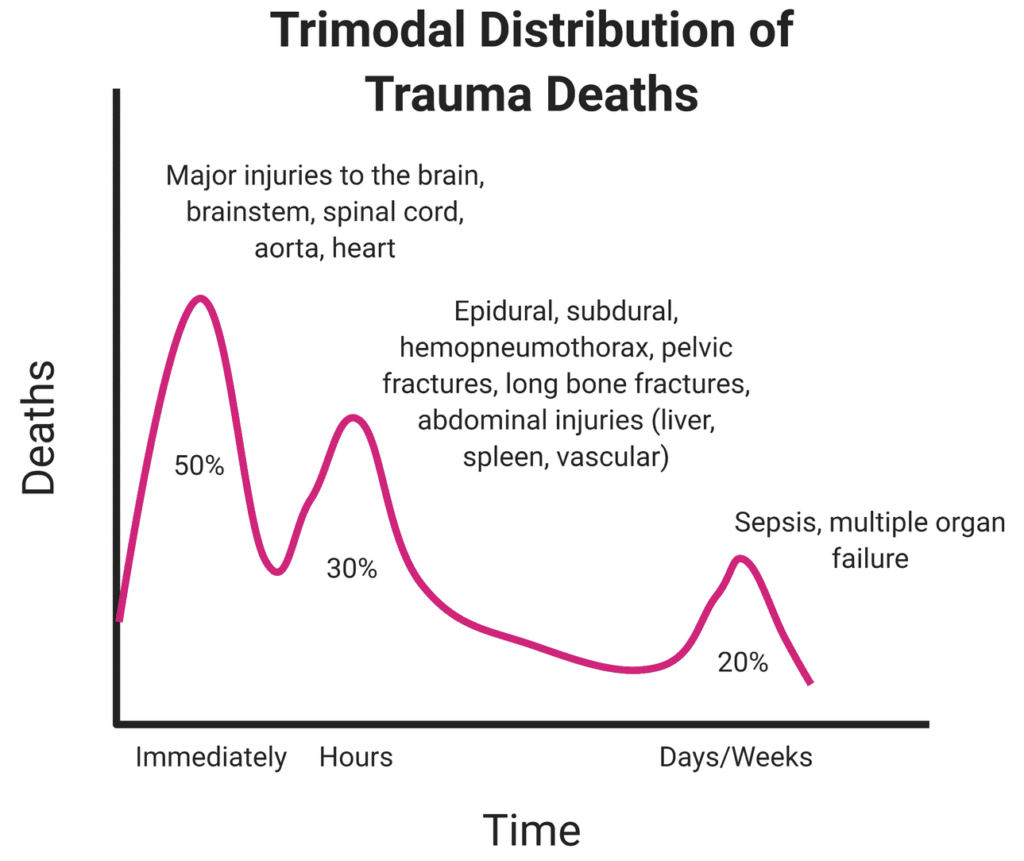
Trimodal distribution of trauma deaths
80% of trauma deaths occur in the first hour (Golden hour). This means that timely intervention saves lives.
50% of trauma deaths occur in the first peak. 30% in the second, and 20% in the third. Immediate response and care of trauma patients is aimed at preventing death from the second peak (1-3 hours)
- First peak: within minutes
- Second peak (Golden hour): 1-3 hours
- Third peak: days to weeks
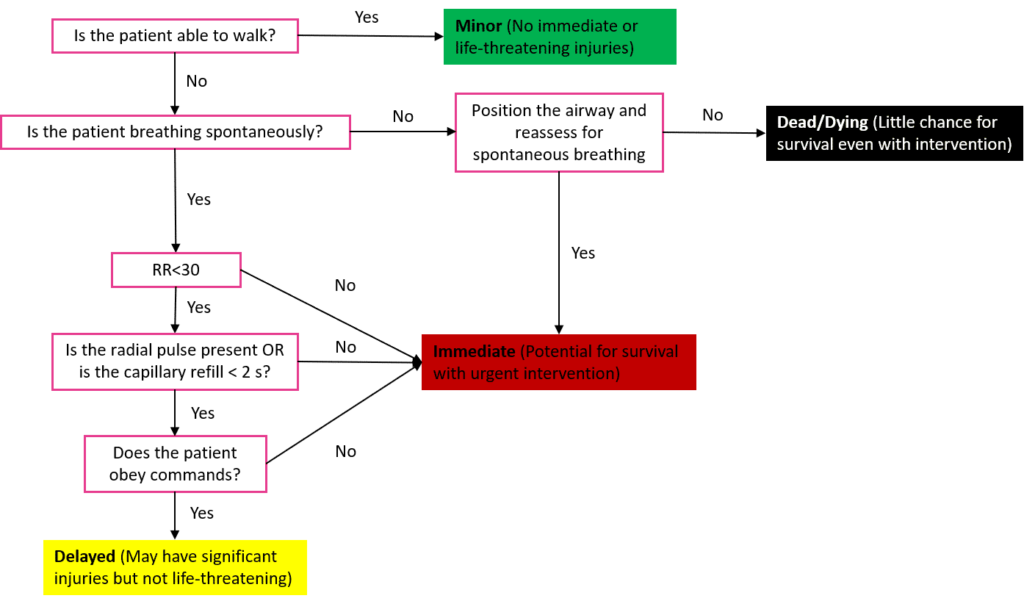
Start System of Triage

Primary Survey
The goal of the primary survey is to identify and treat conditions that constitute and immediate threat to life
- Airway assessment with C-spine stabilization and airway management
- Breathing assessment with ventilatory support and related procedures
- Circulation assessment with immediate hemodynamic support (perfusion) and hemorrhage control
- Disability assessment with TBI management and Neuroprotective measures
- Exposure with environmental survey and Hypothermia management
- Fluid resuscitation
- Glucose (Blood)
Airway Maintenance w/ C-spine Control and airway management
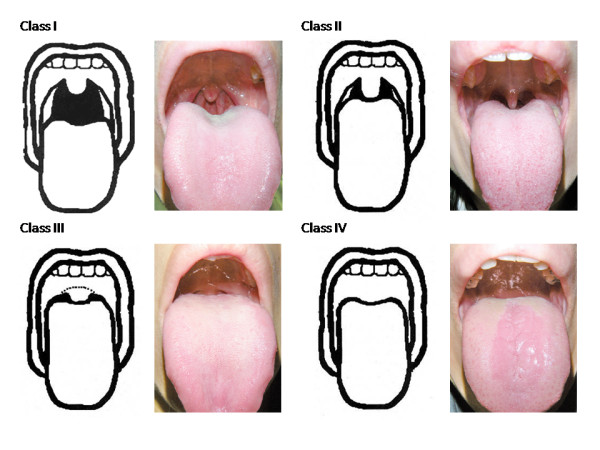
Does the patient need to be intubated?
| Term | Definition |
|---|---|
| Patency | Airway is open and clear and will allow oxygen delivery to the lung |
| Protection | The patient is alert enough to swallow their secretions and not at high risk of aspiration. Depends on mental status |
The easier question should be when doesn’t the patient need to be intubated e.g. conscious, talking normally, normal breath sounds and saturation
Airway obstruction, Loss of airway protective reflexes (AMS or Coma), C-spine injury
- How to assess for airway
- Ask the patient to state their name or ask a question that can be answered easily
- Examine the airway for foreign bodies or injury e.g. secretions, facial fractures, soot, burns
- Evaluate for signs of airway compromise and signs of respiratory distress
- Abnormal voice
- Abnormal breathing sounds
- Tachypnoea
- Initial interventions
- Suction oropharyngeal secretions and/or blood
- Perform airway opening maneuvers: in-line neck immobilization, jaw thrust, and chin lift
- Insert basic airway adjunct e.g. oropharyngeal and nasopharyngeal airway to maintain patency in unconscious patients
Definitive airway
- Indications for intubation
- Patient with declining mental status (GCS ≤ 8)
- Expanding mass (hematoma) in the neck
- Desaturating patient
- Subcutaneous crepitation of the neck or upper chest
- At-risk inhalation injury (moderate to severe facial and oropharyngeal burns, and extensive body burns)
- Methods and techniques for obtaining a definitive airway
- Endotracheal intubation
- Orotracheal intubation: most commonly used; requires expertise; in C-spine injury use bronchoscopy to assist placement
- Nasotracheal intubation: less common; easier to place
- Cricothyroidotomy OR Percutaneous tracheostomy (if facial fractures are present or suspected)
- Surgical tracheotostomy (requires sterile technique hence done in the OR)
- Endotracheal intubation
- Sellick manoeuvre for intubating unconscious patients (in rapid sequence intubation)
- Apply backward pressure on the cricoid cartilage to prevent aspiration of stomach contents
C-spine control
Always assume C-spine injury in patients with significant blunt trauma.
- How to stabilize the C-spine
- Rigid cervical collar and blocks
- Manual stabilization (during intubation)
NEXUS Criteria for clearing the C-spine without imaging
- No posterior midline cervical tenderness
- No evidence of intoxication
- Normal level of alertness
- No focal neurological deficit
- No painful distracting injuries
Breathing and Ventilation
How is the patient breathing?
Assess airflow, breath sounds and the chest regardless of the patient’s intubation status. The lungs, chest wall, and diaphragm should be functioning normally to allow for adequate oxygenation and ventilation.
Good saturation = good airway and breathing
Life-threatening injuries: Tension pneumothorax, Open pneumothorax, Massive hemothorax, Flail chest with underlying pulmonary contusion, Tracheobronchial tree injury
- How to assess for oxygenation
- SpO2
- Continuous pulse oximetry
- How to assess for ventilation
- Observation
- Symmetrical chest rise
- Quality and rate of respiration (increased work of breathing, use of accessory muscles, tachypnoea)
- Neck for JVP and tracheal deviation
- Palpation
- Crepitus or subcutaneous emphysema = rib fracture +/- pneumothorax
- Percussion
- Hyperresonance = Pneumothorax
- Dullness = hemothorax
- Auscultate
- Breath sounds present and equal bilaterally
- eFAST to help ID pneumothorax
- Observation
- Initial interventions
- 100% O2 via NRB
- Emergency chest decompression (for tension pneumothorax)
- Needle thoracostomy in the 4th or 5th ICS MAL in adults and 2 ICS MCL in paediatrics
- Finger thoracostomy in the 4th or 5th ICS MAL
- 3-sided dressing for sucking chest wound
- BMV or mechanical ventilation for respiratory failure
Common presentations
- Tympanic hemithorax, Absent breath sounds
- Pneumothorax
- Hemithorax dull to percussion, distant breath sounds
- Hemothorax
- Paradoxical chest wall movement
- Flail chest
- Palpable crepitations of the chest wall
- Tracheobronchial injury
Circulation w/Hemorrhage Control and hemodynamic support
Is there enough blood being pumped?
Assess BP, HR. Circulatory compromise shows hypotension (<100/60) and tachycardia (>120). Assess pulse at the carotids.
Life-threatening injuries: Massive hemothorax, cardiac tamponade, hemoperitoneum with hemodynamic instubility, unstable pelvic factures with bleeding and hemodynamic instability
- Sources of hemorrhage
- Chest
- Abdomen
- Pelvis
- Long-bones
- External (Floor)
- How to assess hemodynamic status
- Level of consciousness (GCS)
- Adequate communication = adequate perfusion to the brain
- Peripheral pulses
- Central pulses
- Capillary refill time
- Skin
- Cool, mottled skin = shock
- Vitals (HR, BP)
- Continuous cardiac monitoring
- Level of consciousness (GCS)
- Adjuncts for diagnosing sources of bleeding
- Chest radiograph
- Pelvic radiograph
- FAST
- Perihepatic view: fluid in morrison’s pouch (RUQ)
- Perisplenic view: fluid in the splenorenal space (LUQ)
- Pelvic view: fluid in the suprapubic and rectouterine space (pouch of Douglas) in females
- Pericardial view: obtained in the subxiphoid region for fluid in the pericardium
- Lung view: obtained at the highest point of the chest wall when the patient is supine to assess normal pleural movement
- Diagnostic peritoneal lavage
- Initial interventions
- Two Large bore IVs (at least 16G) for IV fluid bolus + Draw blood samples.
- Initial bolus of 1 litre of NS or RL (warmed) followed by blood in patients who need further resuscitations
- Intraosseous access points if peripheral IV cannot be obtained
- Blood tranfusion if unresponsive to IV fluid
- Control of external hemorrhage
- Suture or staple scalp bleeding
- Manual compression of proximal arteries
- Direct pressure to the bleeding
- Clamping visible vessels
- Tourniquet above the injury (mark time of placement to avoid prolonged ischemia)
- Chest tube drainage for hemothorax
- Pericardiocentesis for cardiac tamponade or subxiphoid pericardial window
- Operative management for positive intra-abdominal bleeding
- Pelvic binder or sheet for pelvic fractures
- Two Large bore IVs (at least 16G) for IV fluid bolus + Draw blood samples.
Common presentations
- Hypotension, Tachycardia, AMS, Reduced cap Refill
- Hypovolemic shock d/t severe bleed (external or internal)
- Hypotension, Tachycardia, AMS, Reduced cap refill, JVD
- Pericardial tamponade
- Hypotension, Tachycardia, AMS, Reduced cap refill, JVD, Dyspnea/SOB, Absent breath sounds in affected hemithorax
- Tension pneumothorax
Traumatic circulatory arrest
- Common causes of traumatic circulatory arrest
- Tension pneumothorax
- Cardiac tamponade
- Haemorrhagic shock
- Treatment of traumatic circulatory arrest
- Bilateral chest decompression w/finger thoracostomy (first-line)
- Emergency (Resuscitative or ED) thoracotomy. Indications include:
- Penetrating cardiac trauma with tamponade (on FAST) in a pulseless patients (but with signs of life – pupillary activity and agonal respiration) and received CPR for less than 15 minutes
- Blunt trauma with loss of vital signs (but with signs of life) in a hospital emergency setting
Resuscitative/Emergency thoracotomy
This is a bedside procedure performed in the ER to obtain emergency access to the thoracic cavity in order to provide temporizing lifesaving measures to pulseless patients
- Indications
- Pulseless patient with penetrating thoracic injury
- Pulseless patient after penetrating extrathoracic injury, excluding isolated cranial injuryies
- Pulseless patient with recently documented signs of life in the field or hospital after blunt injury
- Contraindications
- Pulseless patient without any documented signs of life in the field or at the hospital after blunt injury
Advanced Cardiac Life Support
Requires EKG and Established IV line. See Cardiology section
- Cardiopulmonary Resuscitation (CPR; 30/2)
- 30 pumps followed by 2 rescue breaths (pumps at 100 bpm)
- Tilt head back and chin-lift to get good airway (unless there is suspected C-spine injury)
- Allow for chest expansion
- Check for pulse
- CPR modification for peds
- Faster pumping
- Less pressure
- Less breath force
- Pitfalls to delivering CPR
- Insufficient pumping pressure
- Adults: 1.5 – 2 inches
- Peds: 1/3 – 2/3 depth of chest
- Not allowing for recoil
- Recoil allows for the heart to refill
- Not looking at the chest to see if it is rising
- Make sure that you’re getting air into the airway
- Insufficient pumping pressure
Disability assessment w/TBI management and neuroprotective measures
Assess Neurological status
GCS is better to use when you’re dealing with patients with head injury as it will help grade the severity. Remember to remain vigilant for signs of TBI in intoxicated patients
Life-threatening Traumatic Brain Injury
- How to assess disability
- AVPU (quick and easy)
- Calculate GCS
- Assess pupilary light response
- Assess motor and sensory functions
- Initial interventions
- Consult neurosurgeon
- Start neuroprotective measures
- Maintain normoxia, normocapnia, normotension, normothermia (or, in some cases controlled hypothermia), and euglycemia
- Start ICP management if a cerebral herniation syndrome is present
Scoring systems
- AVPU system
- Awake
- Verbal response
- Pain response
- Unresponsive
- GCS Motor response (1-6)
- Obeys verbal command (6), localize to pain to stimulus (5), flexion/withdawal (4), decorticate rigidity (3), decerebrate rigidity (2), no response (1)
- GCS Verbal response (1-5)
- Oriented and converses (5), disoriented and converses (4), inappropriate words (3), sounds (2), no response (1)
- GCS Eye response (1-4)
- Eyes open spontaneously (4), eyes open on command (3), eyes open to painful stimulus (2), no response (1)
Exposure and Environmental Control w/hypothermia management
Expose the patient to assess for injuries, bleeding etc.
- How to assess exposure and provide environmental control
- Undress the patient completey (to facilitate a thorough exam and assessment
- Examine the entire patient for signs of occult injury – axilla, groin, and back (by logrolling)
- Keep the patient warm
- Warm trauma bay
- Warm IV fluids (warmer than room temp, about 39 C)
- Blankets
Adjuncts to the Primary Survey
- EKG monitoring possible findings include
- indicators of blunt cardiac injury- unexplained tachycardia, atrial fibrillation, premature ventricular contractions, ST segment changes
- pulseless electrical activity indicate cardiac tamponade, pneumothorax, profound hypovolemia
- features of hypoxia and hypoperfusion- bradycardia, aberrant conduction, premature beats
- dysrrhythmias due to extreme hypothermia
- Vitals and monitoring
- Pulse oximetry
- Ventilatory rate
- Capnography and ABGs
- Trauma series
- CXR (lateral and AP)
- C-spine XR (at least 2 views)
- Pelvic XR
- CT head (if altered neuro status or reported head injury)
- FAST exam
- Pericardium
- Spleen
- Liver/Kidney
- Bladder
- Acute abdominal series
- AP supine XR
- PA erect XR
- PA erect Chest
- Labs
- CBC
- U/E/Cs
- RBS
- ABGs
- B-HCG (PDT)
- Urine toxicology
- PT/PTT
- Tubes
- Foley catheter
- Nasogastric tube
- Tetanus immunization status/ prophylaxis
Secondary survey
Performed after the patient has been stabilized. Involves a thorough history and physical exam + investigations to diagnose other injuries.
“Tubes and fingers in every orifice”
AMPLE History (Pertinent History)
- Allergies
- Medications
- Past medical History, Pregnancy status and comorbidities
- Last meal eaten and when
- Events and Environment related to the injury
Head to Toe Physical examination
Systematically look for injuries
- Head, face, eyes, ears, nose, and throat
- Scalp and oral cavity
- Teeth and jaw alignment
- Vision and extraocular muscles
- CSF or blood drainage from the nose or ears
- Palpate for skull fractures
- Neck
- Midline tenderness
- Step-offs or areas where the bones are not aligned
- Deformities
- Chest
- Crepitus or subcutaneous emphysema
- Chest pain
- Tenderness
- Bruising
- Deformity
- Abdomen and rectum
- Pain
- Tenderness
- Bruising
- Blood in rectum
- Rectal tone
- Position of the rectum in men
- Pelvis and genitals
- Pelvic stability
- Blood at the urethral meatus
- Penile and scrotal bruising
- Vaginal bleeding
- Vaginal exam in patients with pelvic trauma
- Extremities
- Evidence of fracture
- Neurological and vascular exam
- Comprehensive diagnostic studies and imaging
- Supportive care
Adjuncts to secondary survey
- Additional X-rays of Spine and Extremities
- CT head, chest, abdomen, and spine
- Contrast urography and angiography
- Transesophageal U/S
- Bronchoscopy, Esophagoscopy,
Tertiary survey
- Detailed History and Physical exam (focusing on the MSK and neurovascular system) to identify missed injuries
- Additional diagnostic tests
- Quality and safety measures
