General Principles of Head Injury
Scalp
The Scalp is very vascular and bleeds a lot (messy, but rarely causes shock). The patient’s Hx is very important in making the differentials for a head injury.
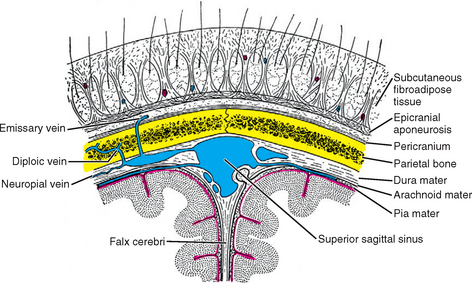
Layers of the scalp
- Layers of the scalp
- Skin
- Connective tissue
- Aponeurosis
- Loose areolar tissue
- Periosteum.
Monroe-Kellie Doctrine
The Monroe-Kellie Doctrine states that the volume within the skull remains constant
- CPP = MAP – ICP
- Bleeding within the skull raises the ICP.
- Raised ICP causes a low CPP.
- The body compromises by raising MAP
Initial Approach
All head injuries are assume to have associated C-spine injury until proven otherwise (5% will actually have concomittant C-spine injury). It is therefore important to rule out C-spine injury before the cervical collar is removed.
Resuscitation
Hypoxia and Hypotension are independent risk factor for mortality in brain injury
- Airway
- Secure airway and provide 100% high flow O2 via NRB mask
- GCS ≤ 8 or other indications should get orotracheal intubation
- Breathing
- Ensure optimal oxygenation and ventilation
- Monitor patient w/ pulse oximetry and frequent checks of respiratory status
- Intubated patients should get an ABG
- Circulation
- Maintain MAP > 90mmHg (MAP directly related to CPP thus hypotension is an independent risk factor for morbidity and mortality)
- Avoid glucose containing fluids (glucose is damaging to the injured brain. Stick to NS)
- Watch carefully for Cushing’s reflex (Increased BP, Decrease HR, Irregular respiration)
- Disability
- Obtain GCS (Helps categorize the head injury. Able to chart how the patient presented and observe any change in status)
- Check pupil size
- Anisocoria = elevated ICP, Dilated pupil is ipsilateral to the lesion
- If there is AMS – Assess for reversible causes (hypoglycemia, hypoxaemia, narcotic overdose, alcohol)
Focused Examination
- Signs and symptoms of raised ICP
- Eye signs: Fixed dilated pupil, Papilloedema, Blurry vision, Abducens Nerve Palsy
- Headache
- Projectile Vomiting
- Seizures
- Altered Mental Status (Drowsiness → cOMA)
- Bulging fontanelles in infants
- Cushing’s triad of raised ICP
- Hypertension (widening pulse pressure)
- Tachypnea (irregular breathing)
- Bradycardia
- Signs and symptoms of basilar skull fracture
- Rhinorrhoea
- Ecchymosis (Battle’s sign, Racoon eyes)
- Otorrhoea
- Hemotympanium
- Hearing loss
- Localizing Signs
- Motor deficits (hemiparesis, hemiplegia)
- Sensory deficits (numbness, tingling)
- Visual field deficits (hemianopsia)
- Asymmetric reflexes
- Speech and language defects (aphasia, dysphasia)
- Other signs to look for
- Scalp Laceration
- Palpate for fractures (not all fractures occur with scalp lacerations)
- Primitive reflexes (Babinski reflex)
Other considerations
- What to do if there is significant head injury
- Consider seizure prophylaxis (Phenytoin, fosphenytoin, carbamazepine)
- What to do if there is post-traumatic convulsions
- Lorazepam or Barbiturates in Children
- Why should narcotics and benzos be started after the initial exam
- Keeps the patient calm
- keeps the patient from moving around
- keeps the ICP low
- What to do if there are signs of raised ICP
- mannitol + IV fluids and maintain serum osmolality < 320 mOSm (don’t dehydrate the patient!)
- What to do if there are signs of basilar skull fracture
- CT scan should extend to include the neck as C-spine injuries are common with Basilar skull fractures
- DON’T forget how to treat causes of AMS
- Dextrose-50 amp (Hypoglycemia – get a bedside RBS)
- Oxygen 100% NRB (hypoxemia – 100% oxygen no matter what)
- Naloxone (Narcotic OD – pinpoint pupils)
- Thiamine with fluids (Alcoholics – Hx, urine tox screen or alcohol smell)
Glasgow Coma Scale
| Best Motor Response | Best Verbal Response | Eye Opening | Points |
|---|---|---|---|
| Follows commands | 6 | ||
| Localized to pain | Oriented | 5 | |
| Withdraws from pain | Confused | Spontaneous | 4 |
| Decorticate posturing | Inappropriate words | To voice | 3 |
| Decerebrate posturing | Incomprehensible | To pain | 2 |
| No response | No response | No eye opening | 1 |
- GCS Eye Opening Response (4 eyes 🤓)
- 4 = Spontaneous
- 3 = To verbal stimuli
- 2 = To pain
- 1 = None
- NT = Non-testable
- GCS Verbal Response (Jackson 5 🎵)
- 5 = Oriented
- 4 = Confused
- 3 = Inappropriate words
- 2 = Incoherent
- 1 = None
- NT = Non testable
- GCS Best Motor response (Inline 6 🏎️)
- 6 = Obeys commands
- 5 = Localizes pain
- 4 = Withdraws from pain
- 3 = Flexion to pain or decorticate
- 2 = Extension to pain or decerebrate
- 1 = None
Grading of TBI
Severe TBI (GCS ≤ 8) requires intubation
| Grade | GCS score |
|---|---|
| Mild TBI | GCS 13-15 |
| Moderate TBI | GCS 9-13 |
| Severe TBI | GCS ≤ 8 |
General Management
Obtain a good Hx of the mechanism of injury and any events surrounding it. Do not remove impaled objects until the patient is in the OR.
- Indications for non-contrast CT-Head
- Loss of consciousness at injury (get a CT even if the patient is lucid)
- Neurological deficit (If GCS is anything less than 15)
- AMS (or confusion)
- If mechanism of injury was moderate to severe
- Suspected skull fracture on palpation
- What are you looking for on head CT?
- Skull fractures
- Intracranial bleeding
- Contusion
- Axonal injury
- Trauma labs to order
- CBC
- BMP
- GXM or O- blood on hand
- Blood alcohol level or toxicology screen
Soft Tissue and Bone Injuries
Scalp lacerations
The scalp is abundantly vascularized and therefore bleeds profusely. Scalp lacerations often appear with skull fracture. Carefully palpate the surrounding tissue and strongly consider a Head-CT.
- Treatment
- Staples
- Simple interrupted sutures
- Look for other injuries and treat as needed
Skull fractures
Suspect skull fractures based on physical exam (palpable fracture) or presence of scalp laceration. The type of fracture is important for determining how to manage the patient.
- Investigation
- Head CT to determine the type of fracture
- Treatment
- Admit w/surgical consult
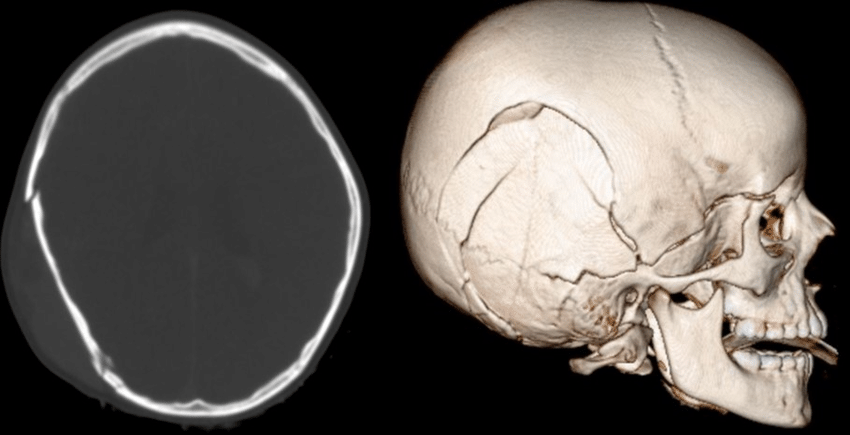
Types of skull fractures
- Closed Skull fracture
- Associated with more serious intracranial problems (hematoma, hemorrhage etc.) that will show up on CT
- Closed fractures need no specific treatment themselves
- Depressed Skull fracture
- Associated with more serious intracranial problems that will show up on CT
- Increased risk of post-traumatic seizure and infection – great indication for Phenytoin. Check with neurosurgeon for antibiotics
- Must be repaired surgically
- Open Skull fracture
- Often associated with scalp lacerations and are easily palpable
- Increased risk of infection
- Must be repaired surgically
- Basilar Skull fracture
- Signs of Basilar Skull Fracture: Racoon eyes, Battle’s sign, Otorrhea, Rhinorrhea, Hemotympanum, Hearing loss
- Must be repaired surgically
Diffuse Intracranial Injuries
Concussion (Minimal head injury)
A concussion is a minor diffuse head injury causing transient disturbance of brain function following acute trauma (ranges from altered mental status to loss of consciousness, but has to have transient confusion or altered mental status) Patients are usually lucid and fine by the time they get to the Emergency Department. Commonly occurs in sports. Though to be due to impairment of the Reticular Activating System caused by shear forces. Important to get a head CT in patients who have had a concussion.
- Signs and symptoms
- Brief subtle changes in consciousness (Transient confusion or AMS)
- Other neuro Sx: headache (resolves within hours)
- What is the primary concern in concussion
- More severe underlying intracranial disorder (Hematoma – hence the need for head CT)
- Indications for head CT in concussion
- GCS ≤ 14 after 2 hours
- GCS was ever ≤ 13 (If they were ever knocked out cold they definitely had a GCS < 13)
- Treatment
- Consider admission and CT if patient does not have reliable care
- No CT? Discharge the patient into reliable care of companions with head injury instruction
- Head injury discharge instructions
- Under care of companions until the companions feel that the patient is back to normal
- No driving or operating heavy machinery
- No drinking alcoholic beverages
- Avoid strenuous activity
- Return to ED if: (new neuro symptoms)
- Persistent nausea and vomiting
- Increased confusion
- Worsening headache
- Visual changes
- New dizziness, difficulty walking
- Drainage from eyes or nose
- Any seizures
- Any new weakness
Diffuse axonal injury (DAI)
Diffuse axonal injury is severe, devastating, and diffuse brain injury resulting in coma. Terminal. Patient usually dies. Fewer than 10% regain consciousness and those who do have profound neurologic deficit (vegetative state)
- Mechanism
- Usually the result of deceleration injuries (MVA) and child abuse
- Wide-spread shearing of axons due to translational force
- When to suspect DAI
- Unresponsive pts w/severe mechanism of injury
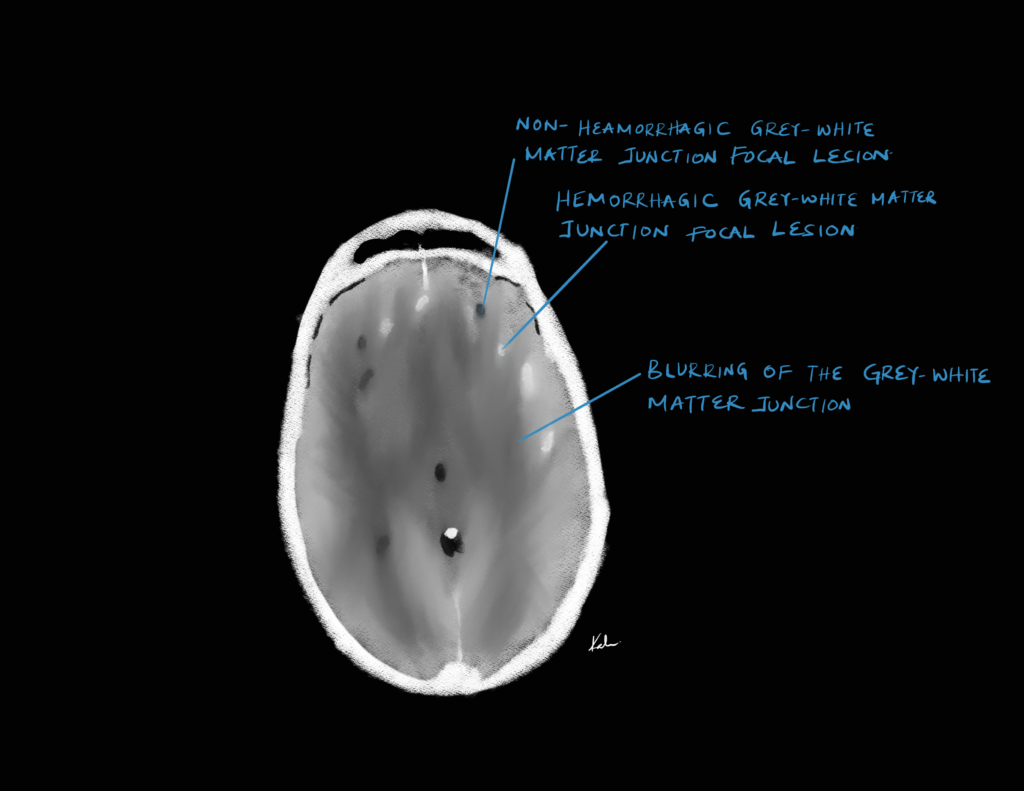
- CT findings suggestive of DAI
- CT-findings in DAI
- Blurring of the grey- and white-matter junction
- Punctate hemorrhages
- Cerebral edema
- Management
- Prevent further damage
Focal Intracranial Injuries
Cerebral contusion
A cerebral contusion is d/t to bruise of the brain tissue. Can be caused by a direct or indirect blow to head resulting in coup, Contre-coup, or coup-contre-coup injury. Diagnosis is via head
CT.
- Coup injury
- Stationary head hit by a moving object
- Direct injury below the skull at the point of impact
- Contre-coup injury
- Moving head hitting a stationary object
- Brain is injured across from the site of blow (forced against the opposite side of the skull during impact)
- Indications for surgical intervention in cerebral contusion
- Significant midline shift (>5mm)
- Severe bleeding
- Severe edema
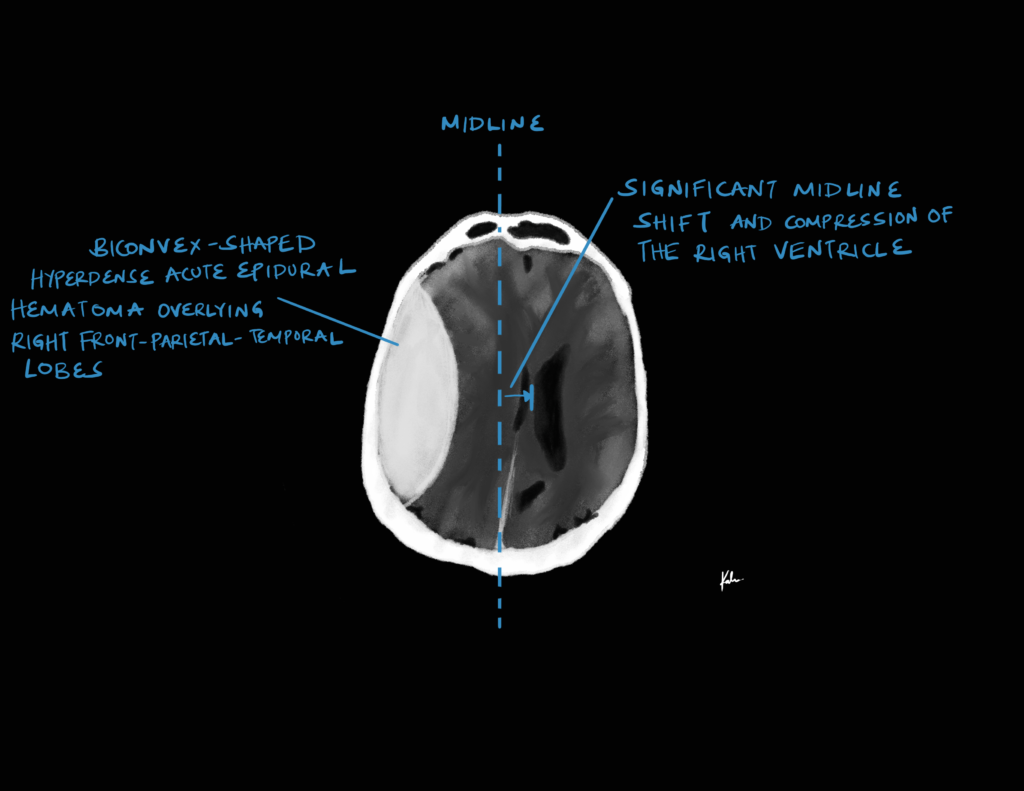
Epidural hematoma
Tearing of the middle meningeal artery causing a bleed between the dura and skull
- Mechanism of injury
- Moderate to severe trauma
- Rapid acceleration/deceleration resulting in high shear forces
- Classic Patient History
- Trivial injury with brief loss of consciousness, followed by a “lucid interval” during which the patient is neurologically intact for up to hours
- The artery continues bleeding → rapid clinical deterioration → coma → death
- Signs and symptoms
- Headache
- Nausea and Vomiting
- Focal Neurological Deficits
- Signs and symptoms of elevated ICP:
- Lateralizing signs: Hemiparesis, Hemiplegia, Asymmetric reflexes, Visual field defects, speech and language defects, ****
- Fixed dilated pupil
- CT finding
- Hyperdense lens-shaped density adjacent to the skull.
- Does not cross suture lines.
- Usually associated with skull fracture.
- Treatment
- Surgical decompression and evacuation if indicated (Burr holes, Craniotomy, Craniectomy)
- Indications for surgical decompression and evacuation
- Midline shift > 10mm
- Hematoma thickness > 5mm
- Intracranial pressure > 20mmHg
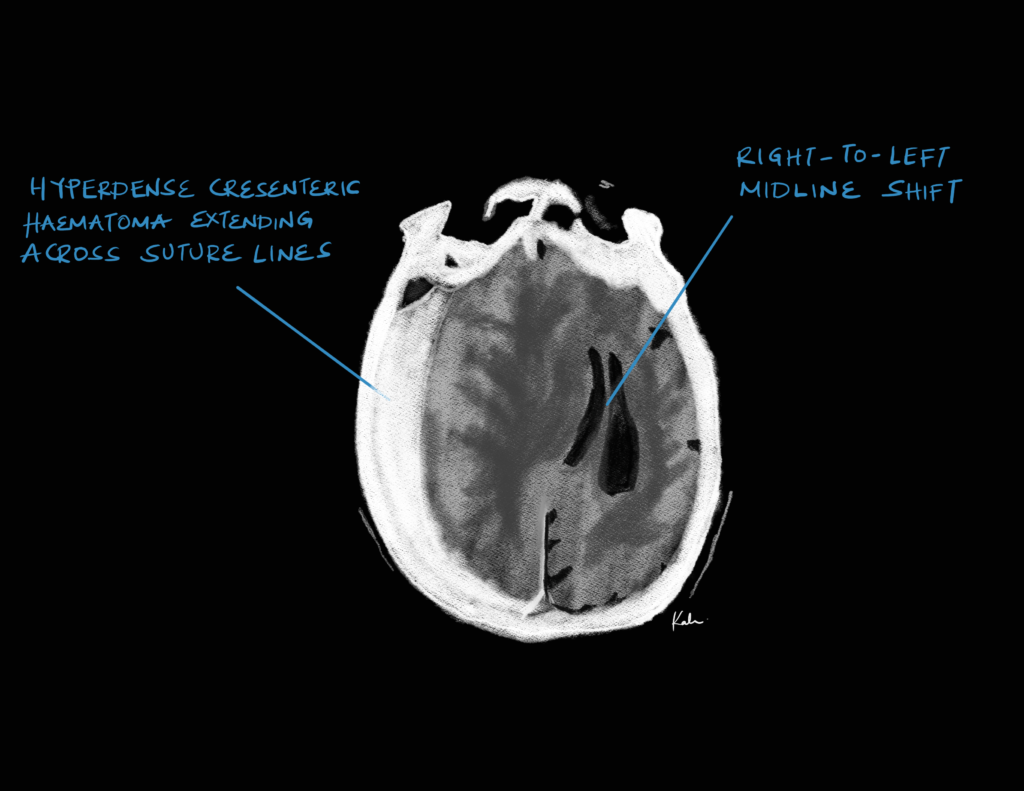
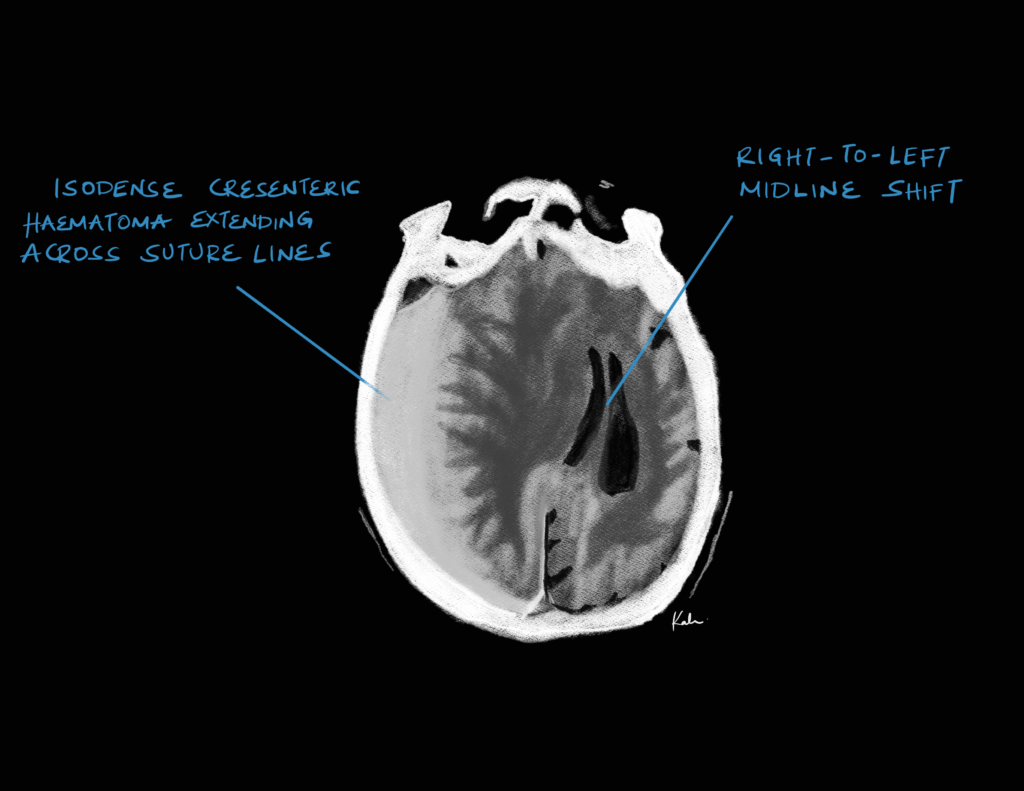
Subdural hematoma
Tearing of bridging veins causing bleed between the dura and arachnoid mater. Veins bleed slower than arteries, hence the insidious onset.
| Acute Subdural Hematoma | Chronic Subdural Hematoma | |
|---|---|---|
| Mechanism | Major trauma e.g. high-energy impact, acceleration-deceleration injury | Minor trauma e.g. fall (the elderly/alcoholic/anticoagulation patient might not remember) |
| Symptom onset | < 3 days of inciting event | ≥ 21 days of inciting event |
| Signs and symptoms | Raised ICP, localizing signs, Fixed dilated pupil | Progressive cognitive decline over weeks to months, ataxia and recurrent falls, personality change, aphasia, memory loss |
- Patients at risk of chronic subdural hematoma
- The elderly
- Neurodegenerative disease (Alzheimer’s)
- Alcohol Use Disorder
- Chronic Diabetes Mellitus
- Precious TBI
- Cerebral irradiation
- CT scan finding
- Hyperdense (acute) or isodense/hypodense (chronic) crescent-shaped density adjacent to the brain parenchyma but not within sulci.
- Crosses suture lines but not the falx.
- Treatment
- Admit for observation
- Surgical Evacuation if indicated (Craniotomy, Craniectomy)
- Indications for surgical evacuation of subdural hematoma
- Midline shift > 10mm
- Hematoma thickness > 5mm
- Intracranial pressure > 20mmHg
- Chronic subdural hematoma
Subarachnoid haemorrhage
Bleeding into the subarachnoid space.
- Spontaneous subarachnid hemorrhage
- d/t rupture of Cerebral artery aneurysm
- Traumatic subarachnoid hemorrhage
- Occurs near the site of skull fracture or cerebral contusion
- Classic signs and symptoms
- Sudden onset “Thunderclap” Headache (“This is the worst headache of my life”)
- Relentless in pain and Holocephalic
- Meningism (Photophobia, neck stiffness, Nausea and vomiting, Kernig and Brudzinski sign)
- +/- Focal neuro signs
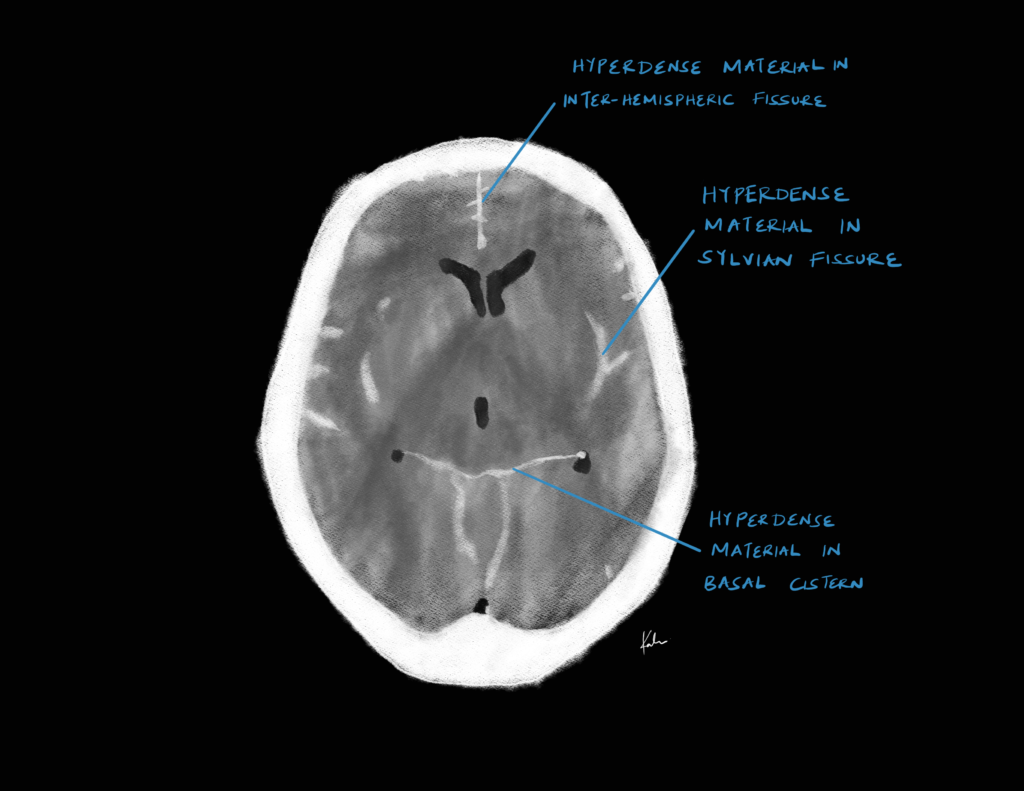
- CT findings
- Hyperdense material adjacent to brain parenchyma tracing along the gyri and sulci.
- Bleeding into the basilar cistern (”Texaco star” pattern)
- Associated contusion or fracture at the site of injury
- Often in coup, contrecoup pattern relative to injury
- Treatment
- Admit to ICU
- ICP monitoring
- Nimodipine (to reduce vasospasms)