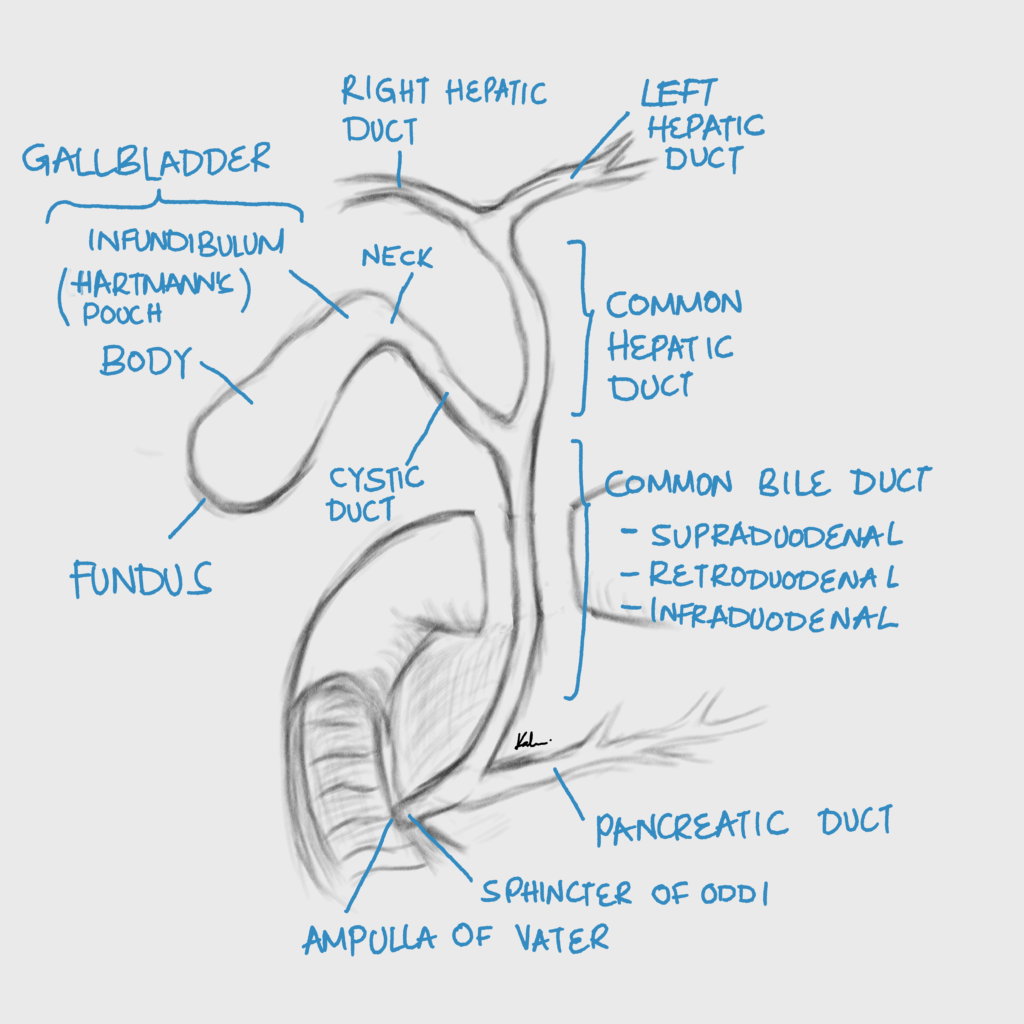
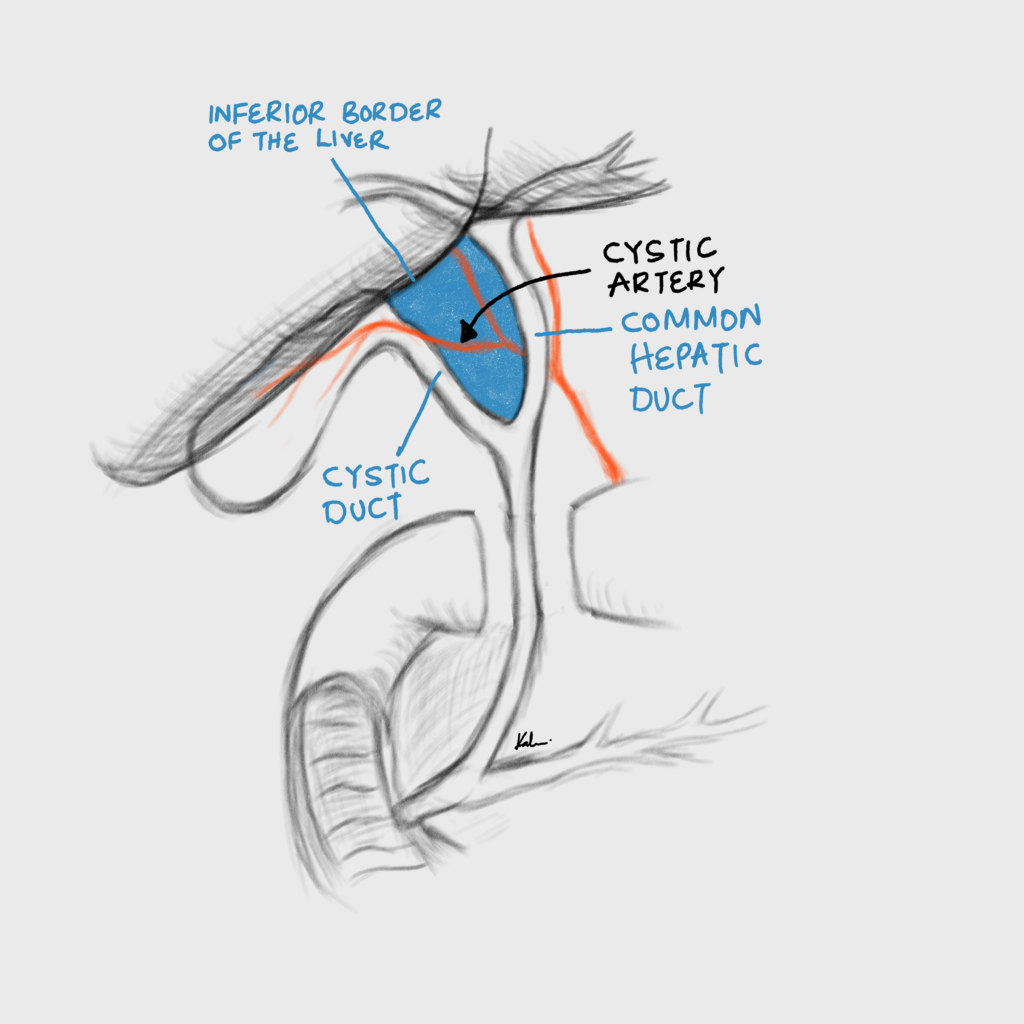
Anatomy
Cholelithiasis
Cholelithiasis is the presence of gallstones in the gallbladder. Asymptomatic cholelithias is discovered incidentally on imaging performed for other reasons. Prophylactic cholecystectomy is NOT recommended. The exception is in a calcified “porcelain” gallbladder, which in itself is an indication of cholecystectomy. There are three different types of stones.
Gallstones
| Stone | Appearance | Association |
|---|---|---|
| Cholesterol stones | Yellow-brown and crystalline | Hypercholesterolemia |
| Bilirubin stones | Black and hard | Hemolysis |
| Calcium bilirubinate stones | Brown, soft or greasy | Inflammation of the biliary tree |
- Risk factors for developing cholesterol gallstones
- Female gender
- Parity
- Age > 40 years
- Obesity
- Parity
- High-fat diet
- Heredity (hispanics, pima indians)
- Crohn’s disease
- Terminal ileal resection
- Rapid weight loss after bariatric surgery
Symptomatic Cholelithiasis
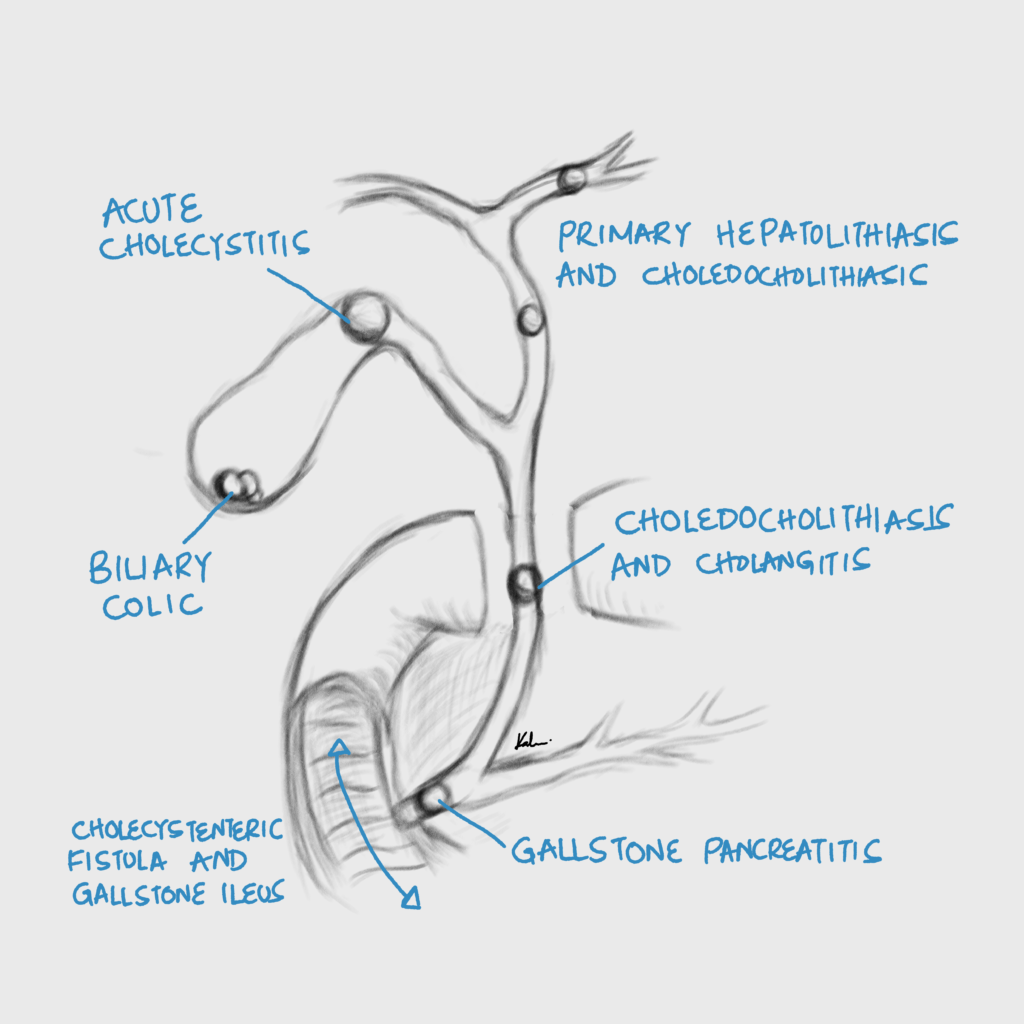
Symptomatic cholelithiasis AKA biliary colic is constant, dull RUQ pain caused by transient blockage of the cystic duct by stones.
- Signs and symptoms
- RUQ or epigastric pain
- Constant and dull
- Resolves within an hour
- Post-prandial (after a fatty meal, d/t vagal stimulation of CCK)
- May radiate to the epigastrium, right shoulder, and back
- May have nausea, vomiting, bloating, early satiety, and dyspepsia
- RUQ or epigastric pain
- Investigations
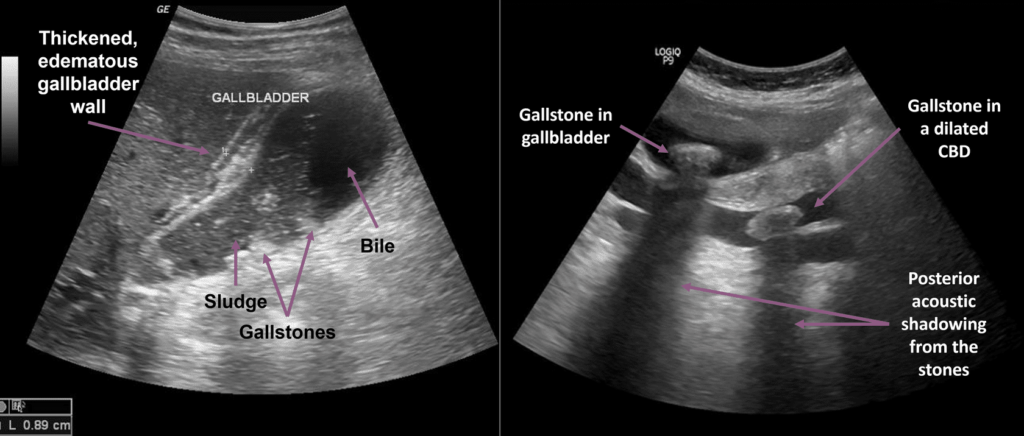
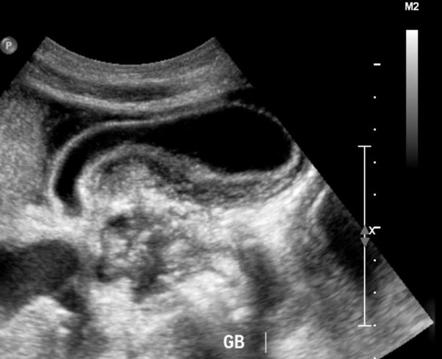
- RUQ ultrasound: best diagnostic test
- Stones in gallbladder
- Normal gallbladder
- RUQ ultrasound: best diagnostic test
- Treatment
- Elective cholecystectomy
Acute Calculous Cholecystitis
Acute cholecystitis is inflammation of the gallbladder usually with an underlying infection (75%) due to obstruction of the gallbladder neck or cystic duct.
- Signs and symptoms
- Fever
- Nausea and vomiting
- RUQ pain/tenderness
- Positive murphy sign
- Differentials
- Acute hepatitis
- Right lower lobe pneumonia
- Pancreatitis
- Pyelonephritis
- Myocardial Infarction
- Investigations
- RUQ Ultrasound: best initial diagnostic step
- Pericholycystic fluid
- Thickened gallbladder wall (>3mm)
- Sludge
- CBC: leukocytosis, left-shift
- LFTs: mildly elevated Total bilirubin, AST
- Amylase: to rule out gallstone pancreatitis
- Urinalysis: to rule out pyelonephritis especially in women.
- b-hCG: in women of childbearing age to rule out pregnancy because antibiotics are going to be administered
- CXR: to rule out right lower lobe pneumonia if indicated
- EKG: to rule out myocardial infarction. May show sinus tachycardia. Optional in younger patients
- RUQ Ultrasound: best initial diagnostic step
- Treatment
- Admit
- Nil Per Oral
- Analgesics
- IV fluids
- IV antibiotics to cover gram negative and anerobes
- Metronidazole + Ampicillin/Gentamicin
- 1st and 2nd Generation cephalosporins e.t.c.
- Cholecystectomy
- Preferably within 48 hours
Acute Acalculous Cholecystitis
Acalculous cholecystitis is an acute life-threatening necrotic-inflammatory disorder of the gallbladder, usually seen in critically ill patients, that is not associated with gallstones. It has a higher mortality rate than acute cholecystitis (10-50%). Severe illness is a major risk factor for acalculous cholecystitis. Treatment is to decompress or remove the gallbladder ASAP.
- Risk factors
- Sepsis
- Burns
- Trauma
- Dehydration
- Mechanical Ventilation
- Surgery
- Immunodeficiency
- Why is there inflammation in acalculous cholecystitis without compression of the gallbladder neck?
- Local ischemia and impaired venous return in critically ill patients → local ulceration → seeding ground for bacteria
- Total parenteral nutrition has also been implicated to cause acute acalculous cholecystitis by promoting the formation of sludge
- Signs and symptoms
- Fever
- RUQ pain
- Severe and prolonged (> 6 hours, than biliary colic)
- Post-prandial
- Radiates to the right scapula (due to diaphragmatic irritation)
- Nausea and vomiting
- Fever, malaise, anorexia
- RUQ tenderness or mass
- Murphy sign positive
- Guarding
- Investigations
- RUQ ultrasound: best initial diagnostic step. Will show inflammation of the gallbladder
- Gallbladder wall thickening (>3-5mm)
- Pericholecystic fluid,
- No stones (though sludge may be present)
- HIDA scan (Cholescintigraphy): gallbladder not visualized within 4 hours (or within 30 minutes after the administration of morphine)
- CT abdomen with IV contrast
- Labs
- CBC: leukocytosis
- CRP: elevated
- Blood culture
- Bile culture: In patients undergoing laparoscopic cholecystectomy or gallbladder drainage
- LFTs: mild elevation in AST and ALT
- Lipase and amylase: mild elevation of amylase, >3 times normal suggests acute biliary pancreatitis
- RUQ ultrasound: best initial diagnostic step. Will show inflammation of the gallbladder
- Treatment
- IV fluids
- IV broad-spectrum antibiotics
- NPO
- Emergent laparoscopic cholecystectomy (ideal Treatment if the patient is a surgical candidate)
- Percutaneous Cholecystostomy to decompress the gallbladder (if the patient is not a surgical candidate)
Biliary dyskinesia
Biliary dyskinesia is disordered motility or contraction of the biliary tract. It can also be due to an abnormal high tone at the sphincter of Oddi, resulting in pain. Think of it as a constipated biliary tract.
- Signs and symptoms
- RUQ pain
- Nausea
- Variable fever
- Investigations
- RUQ ultrasound: unremarkable
- HIDA scan with Cholecystokinin: best diagnostic step
- Impaired gallbladder emptying
- Labs
- CBC: leukocytosis
- LFTs: disturbed
- Treatment
- Elective laparoscopic cholecystectomy
- Oddi sphincterotomy
Choledocholithiasis
Choledocholithiasis is obstruction of the biliary tract at the level of the common bile duct (CBD). It has a similar presentation to cholecystitis but is often accompanied with jaundice.
Females > Males. Peak incidence at > 40 years. Exact prevalence is unknown. But 5-20% of patients who undergo cholecystectomy have choledocholithiasis at the time of surgery
| Choledocholithiasis | Cause | Risk factors |
|---|---|---|
| Primary choledocholithiasis | Bile stasis | Prolonged parenteral nutrition, cystic fibrosis |
| Secondary choledocholithiasis | Passage of gallstones into the bile duct | H/O cholelithiasis, H/O cholecystectomy (post-cholecystectomy choledocholithiasis) |
| Post-cholecystectomy choledocholithisais | Presentation |
|---|---|
| Residual stones | Symptomatic < 3 years after surgery |
| Recurrent stones | Symptomatic > 3 years after surgery |
- Other risk factors for choledocholithiasis
- Periampullary duodenal diverticulum
- Dilated CBD
- CBD stricture
- Chronic cholangitis
- SCA
- Rapid weight loss (e.g. after bariatric surgery)
- Signs and symptoms
- RUQ pain
- Severe and prolonged (longer than cholelithiasis – >6 hours)
- Post-prandial
- May radiate to the epigastrium, right shoulder, and back (due to irritation of the diaphragm)
- RUQ tenderness
- Nausea and vomiting anorexia
- Jaundice, Pale stool, Dark urine, Pruritus
- Can have features of complications: Acute pancreatitis, acute cholecystitis, acute cholangitis (Triad and Pentad)
- RUQ pain
- Differentials of jaundice with a dilated bile duct
- Biliary stricture
- Cancer head of pancreas
- Cholangiocarcinoma
- Mirizzi syndrome (an exception to Courvoisier’s law where the extrahepatic bile duct is compressed by a stone at the neck of the gall bladder or cystic duct leading to obstructive jaundice)
- Courvoisier’s ;aw: Painless jaundice + palpable gall bladder = malignant obstruction and unlikely to be stones
- Investigations
- RUQ ultrasound: best initial step, make sure you visualize the CBD
- Dilated common bile duct (CBD)
- Stone in CBD
- CT-abdomen with IV contrast
- Dilated CBD with or without dilation of the intrahepatic biliary tree
- Target sign (central hypodense stone surrounded by hyperdense bile)
- ERCP:
- Smooth-walled, well-defined, intraluminal filling defects within the CBD
- Dilated CBD
- Dilation of intrahepatic biliary tree
- Cholelithiasis
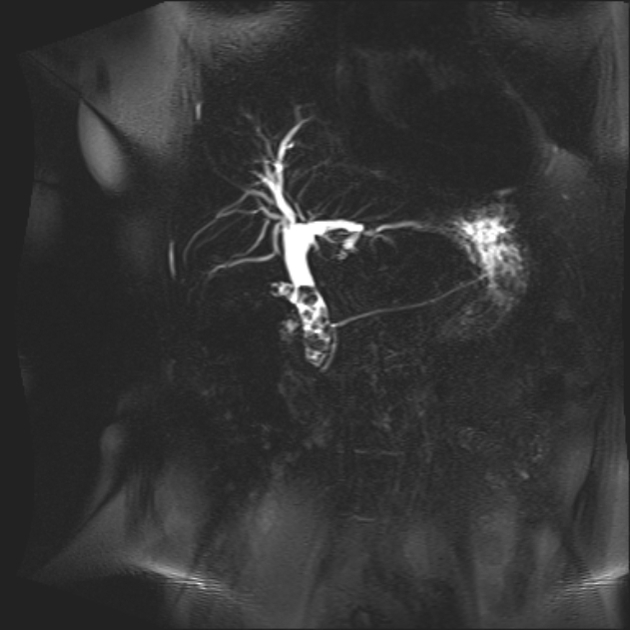
- MRCP: similar findings to ERCP
- Endoscopic Ultrasound (EUS): same findings as transabdominal ultrasound
- Labs
- LFTs: Elevated ALP, GGT, Total and Direct bilirubin
- CBC: Leukocytosis to r/o cholecystitis and cholangitis
- Amylase and Lipase: To r/o biliary pancreatitis
- RUQ ultrasound: best initial step, make sure you visualize the CBD
- Treatment
- Options for CBD stone removal
- ERCP w/ sphincterotomy and retrieval of CBD stone
- Laparoscopic bile duct exploration with intra-op stone extraction (LCBDE)
- Lithotripsy
- Elective laparoscopic cholecystectomy may follow
- Options for CBD stone removal
- Complications of choledocholithiasis
- Gallstone ileus
- Gallstone pancreatitis
- Acute cholangitis
- Acute cholecystitis
- Biliary stricture
- Pyogenic liver abscess



Acute (Ascending) Cholangitis
Cholangitis is an ascending bacterial infection of the biliary tract due to obstruction. It is a true medical/surgical emergency! ****Presents with charcot’s triad of fever, jaundice, and RUQ pain. It is a clinical diagnosi and should be treated ASAP. The best initial step is IV fluids resuscitiation and IV broad spectrum antibiotics, as well as getting blood for labs and blood culture.
Females > Males. Incidence is 9% of patients with cholelithiasis. Peak incidence at 50 – 60 years
- Risk factors
- Choledocholithiasis (MCC)
- Biliary strictures
- Congenital
- Infectious: HIV
- Inflammatory: PSC, IgG4 related sclerosing cholangitis
- Iatrogenic: ERCP, Stent placement
- Malignant obstruction
- Cholangiocarcinoma
- Cancer head of pancreas
- Extrinsic compression
- Mirizzi syndrome
- Parasitic infection
- Liver fluke
- Hydatid cyst
- Ascaris spp.
- Acute pancreatitis
- Periampullary duodenal diverticulum
- Contamination of bile with intestinal contents
- Biliary-enteric fistula (cholecystoenteric, choledochoenteric, endoscopic gallbladder drainage)
- Manipulation of the biliary tract
- Papillotomy
- Stent placement
- ERCP
- Liver transplant
- Signs and symptoms
- Charcot’s triad
- RUQ abdominal pain
- High fever
- Jaundice (least common feature)
- Reynolds Pentad (fulminant sepsis → associated with significant morbidity/mortality)
- Charcot’s triad
- Hypotension
- Altered mental status
- Features of sepsis, septic shock, and multiorgan dysfunction; depending on the disease severity
- Charcot’s triad
- Differentials of RUQ pain with fever (+/- jaundice)
- Acute calculus cholecystitis and its complications (emphysematous cholecystitis, gangrenous cholecystitis)
- Acalculous cholecystitis
- Liver abscess
- Acute hepatitis
- Bile leak (Iatrogenic post ERCP, postcholecystectomy)
- Acute necrotizing pancreatitis
- Malignancy (supported with anorexia and significant weight loss)
- HCC
- Gall bladder cancer
- Cholangiocarcinoma
- Carcinoma head of pancreas
- Mets
- Investigations
- RUQ ultrasounds; Dilated CBD, Dilated intrahepatic bile ducts, Thickened bile duct walls evidence of choledocholithiasis, biliary stricture or biliary tumor
- CT scan with IV contrast: Concentric thickening and heterogeneous enhancement of the walls of the biliary tree, Bile duct dilation, Periductal edemaa etc.
- MRI abdomen without and with IV contrast with MRCP
- Labs
- CBC: Leukocytosis with left shift
- CRP: elevated
- Blood culture
- LFTs: increased bilirubin, Increased GGT, Increased ALP, increased ALT (Cholestasis)
- **Bile culture (**during biliary drainage procedure)
- Treatment
- Admit
- IV fluids
- IV broad spectrum antibiotics
- NPO
- Urgent biliary drainage via:
- Percutaneous transheptic cholangiogram (PTC)
- ERCP
- Elective cholecystectomy should follow
 Percutaneous transhepatic cholangiogram
Percutaneous transhepatic cholangiogram
Other Conditions
Emphysematous cholecystitis
Emphysematous cholecystitis is colonization of the gallbladder wall by anerobic gas-forming organisms, resulting in air in the gallbladder wall. Diagnosed by ultrasound
- Treatment
- Emergent cholecystectomy along with usual Treatment of acute cholecystitis
Gangrenous cholecystitis
Gangrenous cholecystitis is extreme inflammation of the gallbladder causing thrombosis of the cystic artery and ischemic necrosis of the gallbladder tissue. Diagnosed by ultrasound.
- Treatment
- Emergent cholecystectomy along with usual treatment of acute cholecystitis
Perforated gallblader
This is perforation of the gallbladder wall resulting in biliary and septic spilage into the peritoneum. Will have peritoneal signs (not present in typical acute cholecystitis). Diagnosed by peritoneal signs + ultrasound.
- Treatment
- Emergent cholecystectomy + Peritoneal lavage + Usual Treatment of acute cholecystitis
Post Cholecystectomy Syndrome
Post cholecystectomy syndrome is persistent RUQ pain OR any other new symptoms following GB removal.
- Differentials for post-cholecystectomy syndrome
- Biliary
- Choledocholithiasis
- Biliary stricture
- Sphincter of Oddi dysfunction
- Pancreatic
- Pancreatitis
- Pancreatic pseudocyst
- Pancreatic malignancy
- Other GI causes
- GERD
- Inflammatory bowel syndrome
- Peptic ulcer disease
- Extraintestinal cause
- Coronary artery disease
- Pain syndromes
- Wound neuroma
- Biliary
Porcelain Gallbladder
Porcelain gallbladder is calcification of the GB wall due to chronic inflammation. Cholecystectomy is indicated as this is a risk factor or gallbladder ca (10-30%). Imaging shows hyperdensity (radio-opaque) appearance of the GB.
- Treatment
- Cholecystectomy (even if asymptomatic)
Gallstone Ileus
Gallstone illeus is mechanical obstruction of the gastrointestinal tract by stones at the ileocecal valve or pylorus (Bouveret syndrome)
- Causes
- Gallbladder perforation
- Biliary-enteric fistula (due to Mirizzi syndrome)
- Signs of distal bowel obstruction
- Abdominal pain/tenderness
- Abdoinal distention
- Obstipation
- Nausea and vomiting
- Signs of gastroduodenal obstruction
- Vomiting
- Post-prandial
- Non-bilious
- Early satiety
- Weight loss
- Abdominal distension
- Succussion splash (pathological if ≥ 3 hours of fasting)
- Vomiting
- Investigations
- CXR: Rigler’s triad triad
- Features of small bowel obstruction
- Gallstone (in iliac fossa)
- Pneumobilia (gas in the biliary system)
- CXR: Rigler’s triad triad
- Treatment
- Admit
- IV fluids
- IV empiric antibiotics for intra-abdominal infections
- Analgesics
- NG tube for decompression
- Emergent enterolithotomy
- Elective cholecystectomy with closure of the biliary-enteric fistula

