- Overview
- Pathophysiology of burns
- Types of burns according to mechanism
- Classification of burns according to depth
- Classification of burn according to extent
- Classification of burns according to severity
- Pre-Hospital Treatment and First Aid
- Outpatient management
- Hospital Management of Burns
- Special management for non-thermal burns
- Complications of burns
Overview
A burn is defined as the response of the skin, mucous membrane, and subcutaneous tissues to thermal and other few non-thermal injuries. Treatment of burns is complex (hence the need for specialized burn centres), and depends on the site of burn, the severity, mechanism, and comorbid conditions
- Relevant History
- The exact mechanism of burn
- Temperature of flame or water
- Duration of contact
- Concentration of the chemical
- Voltage of the electricity in electrical burns
- Factors that suggest inhalation injury
- Burn in a confined space
- Flash burns
- Document first aid given so far
- Document timing of injury, first aid, and resuscitation
- The exact mechanism of burn
- Signs and Symptoms that indicate respiratory compromise
- History of being trapped in a room with superheated air, smoke
- Burns to the palate or nasal mucosa
- Burns to the lower face, neck
- Soot present around the mouth or nares
- Greyish or blackish sputum (Sooty sputum)
- Singed nasal hairs
- Stridor, hoarseness, dyspnea, persistent hypoxia
- Drowsiness or confusion (d/t carbon monoxide poisoning)
- Full-thickness, circumferential burns to the chest wall
- Findings that are consistent with non-accidental injury (including burns)
- The explanation of injury does not fit the physical exam findings
- Inconsistency or change with repeated explanations of the injury
- Caregiver seems angry or avoids discussion when the medical professional seeks further details regarding the injury
- Description of events of injury is not consistent with the developmental age of the child e.g. an explanation that involves crawling or walking if a child is not able to do so
- History of abuse of other children or the child being treated
- Specific patterns of burn injury that are suspiscious for non-accidental injury
- Burns to the face, head, buttock, perineum, and genitalia
- Obvious patterns from objects e.g. cigarettes, iron, light bulb, hot plate, knife, grid, fork
- Symmetrical burns of uniform depth
- Other signs of physical abuse e.g. bruises of varied ages and in areas not typical for bruising, old fractures
Pathophysiology of burns
Physiological response to burns
| Stage I | Emergent |
|---|---|
| Stage II | Fluid-shift |
| Stage III | Hypermetabolism |
| Stage IV | Resolution |
Local effects of burns
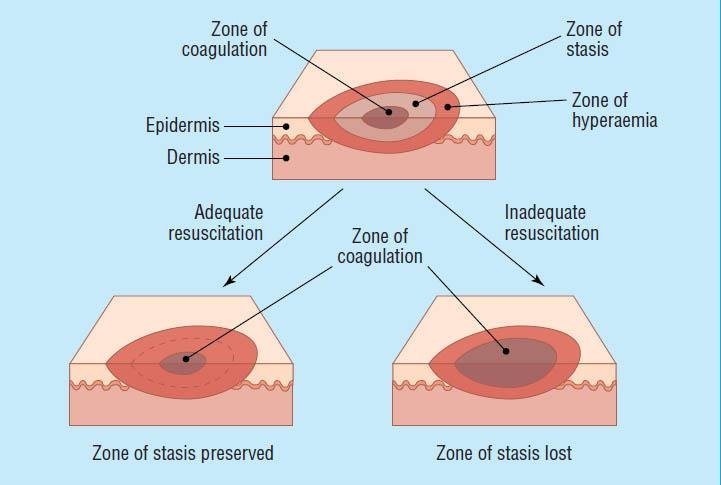
Burns cause local damage by coagulation necrosis from the direct transfer of energy. Other types of burns e.g. chemical and electrical burns directly damage the cell membrane. Adequate resuscitation and good wound care can prevent the progression of a superficial to a deeper burn. Inappropriate resuscitation and infection can worsen the depth of a burn wound, causing a burn that would heal without needing a skin graft to ultimately require grafting.
Jackson’s zones of tissue damage following a burn injury
| Zone | Description | Nota bene |
|---|---|---|
| Zone of coagulation | Most severely burned tissue, usually in the center of the wound. Represents an area of irreversible tissue loss due to protein denaturation and coagulation necrosis | Damage is irreversible |
| Zone of stasis | Immediately surrounds the zone of coagulation and represents the zone of reduced tissue perfusion due increased vascular permeability and vascular damage worsened by Thromboxane A2 which causes vasoconstriction and is present in high amounts in burn wounds | Damage is reversible. Susceptible to further injury and can progress to coagulation necrosis |
| Zone of hperemia | Represents an area of increased tissue perfusion, vasodilation, and microvascular permeability and edema | Changes are reversible and the area is prone to recovery unless there is prolonged hypotension or infection |
Image of Jackson Zones
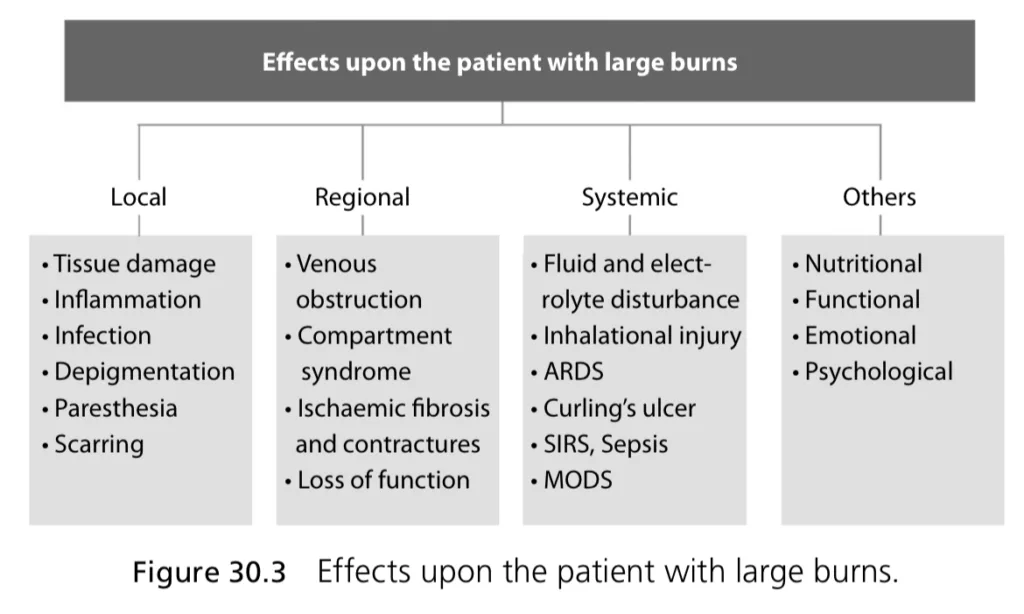
Systemic effects of burns
- Metabolic changes
- Cardiac output initially decreases. However, in the first 5 days cardiac output increases to nearly 1.5 times normal resulting in myocardial oxygen consumption that can exceed that of marathon runners
- Hyperglycemia due to increased gluconeogenesis, glycogenolysis, and reduced insulin sensitivity.
- Protein breakdown resulting in loss of muscle mass and reduced strength
- 10% loss leads to immune dysfunction
- 20% loss leads to decreased wound healing
- 30% loss leads to an increased risk of pneumonia and pressure ulcers
- 40% loss leads to death
- Anorexia
- Pyrexia
- Stimulation of hepatic lipid synthesis
- Promotion of acute-phase protein synthesis
- Reduced albumin synthesis (a negative acute-phase protein
- Inflammation and oedema
- Third spacing due to increased capillary permeability (capillary leak). This leads to hypoperfusion
- Effects on cardiovascular system
- Cardiac output initially decreases but then increases over time
- Depressed cardiac output is due to decreased blood volume, increased blood viscosity due to fluid losses, and ventricular dysfunction
- Increased cardiac output is due to tachycardia (can be 160-170% higher than normal in paediatric patients)
- Cardiac output initially decreases but then increases over time
- Effects on the respiratory system
- Bronchoconstriction
- ARDS due to cytokine-mediated vascular and tissue damage
- Inhalational injury can directly damage the oro-tracheal-bronchial tissues, and increase the likelihood of ARDS
- Lung damage also predisposes to pneumonia
- Effects on the cardiovascular system
- Curling’s ulcer due to splanchnic hypoperfusion
- Splanchnic hypoperfusion leads to stress-induced gastric hypersecretion and mucosal damage)
- Mucosal atrophy (12-18 hours post-burn)
- Decreased absorption of glucose, amino acids, and fatty acids
- Increased intestinal permeability which promotes translocation of bacteria and fungi (can be reversed by early enteral feeding)
- Curling’s ulcer due to splanchnic hypoperfusion
- Effects on the renal system
- Acute renal failure due to thirds spacing, decreased blood volume, and reduced cardiac output
- Effects on the immune system
- Immunosuppression in burns > 20% TBSA (reduced production, function, and activation of neutrophils, macrophages, and B- and T-lymphocytes)
- Increased risk for pneumonia and wound infections
- Immunosuppression in burns > 20% TBSA (reduced production, function, and activation of neutrophils, macrophages, and B- and T-lymphocytes)
Types of burns according to mechanism
55% of burns are caused by flame and 40% are caused by scalds. Chemical and electrical burns comprise about 5%. Scalds are common in children. Electric and chemical burns are common in adults. Flame burns > scalds in adults.
| Burn | Description | Nota bene |
|---|---|---|
| Thermal burn | Flame burn | Responsible for 50% of burns in adults and the most common cause of admission and mortality due to associated inhalational injury, trauma, and carbon monoxide poisoning. Tends to be deep partial thickness and full thickness. |
| Scald | Burn caused by spilling or exposure to hot liquids. Common in children (70% in children under 5) and the elderly. More superficial than flame burns | |
| Contact burn | Burn caused by prolonged direct contact with very hot or very cold objects. Common in patients with epilepsy, the elderly, or with alcohol abuse. Can arouse suspicion for non-accidental burns. Typically partial-thickness or full-thickness | |
| Flash burn | Burn caused by hot gases or combustible liquid | |
| Frostbite | Occurs when skin is exposed to extreme cold | |
| Chemical burn | Exposure to extreme acids (Battery, HCL) or alkali (Drain cleaner, fertilizer) | Evolves over time. Alkaline burns are worse due to liquefaction. Acid burns produce coagulation necrosis. Formic acid can cause hemolysis and hemoglobinuria, hydrofluoric acid can cause hypocalcemia |
| Electrical burn | Electrical shock or lightning strike | Can cause deep tissue injury between the entry and exit points (muscles, heart, and nerves) and lead to serious complications. Voltage determines the extent of damage. |
| Respiratory (Inhalation) burn | Thermal (superheated air) or Chemical (smoke) inhalation | A major concern is respiratory compromise and CO exposure. Burning plastics can produce hydrogen cyanide |
| Circumferential burn | Burns on the chest wall that go around the entire circumference | Tourniqet effect – remove patient accessories ASAP as oedema can interrupt the vascular supply to the distal extremity. Can also interfere with breathing if on the chest wall. Indication for Escharotomy. |
| Radiation burn | Sunburn from UV radiation, X-rays and other imaging, Therapeutic radiation | |
| Friction burn | Heat causes mechanical disruption of tissue from contact with an abrasive or rough surface |
Classification of burns according to depth
Factors that determine the depth of burn include the mechanism, temperature, duration of contact, and thickness of skin.
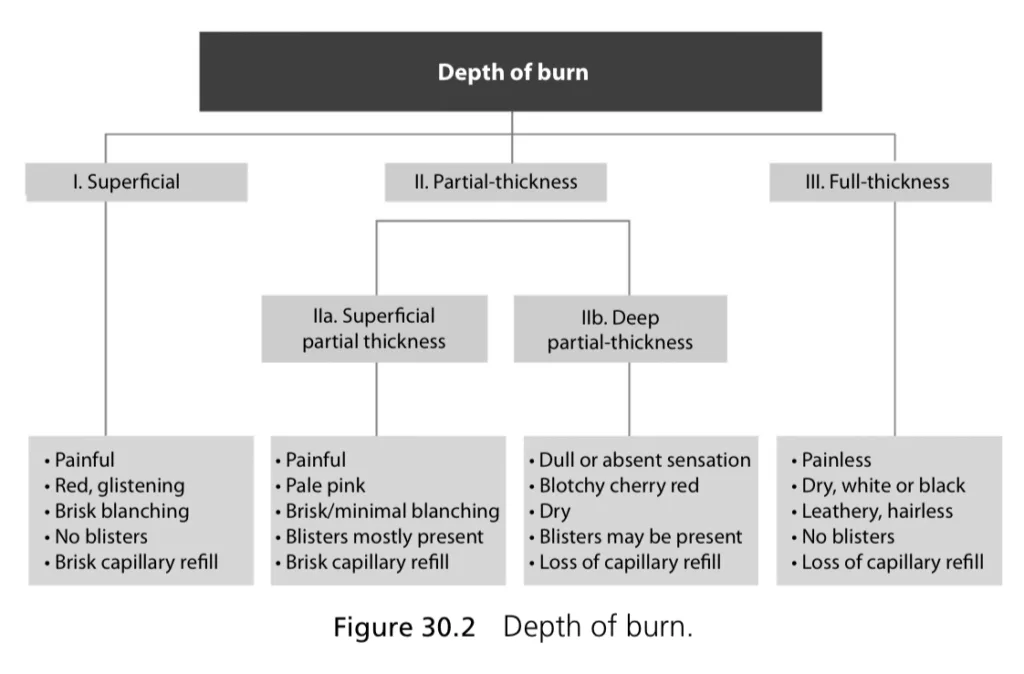
| Severity | Depth | Extent | Appearance | Skin texture | Pain | Sensation | Capilary refill | Healing |
|---|---|---|---|---|---|---|---|---|
| First-degree | Superficial | Epidermis | Red, glistening | Normal; blanches w/pressure | Yes | Present | Present | 5-10 days; no scar |
| Second-degree Superficial | Superficial partial-thickness | Superficial dermis | Pale pink (+/- blister) | Edematous; feels moist; minimal blanching | Yes | Present | Present | 10-21 days; no or minimal scar |
| Second-degree deep | Deep partial thickness | Deep Reticular dermis | Pale pink | Dry | Possible | Possible | Possible | 25-60 days; dense scar |
| Third-degree | Full-thickness | Epidermis and dermis | Pale, white or black (+/- Eschar) | Dry and Leathery; Does not blanch with pressure | No | Absent | Absent | No spontaneous healing |
| Fourth-degree | Subdermal | Damage to muscles, tendons, bones | Pale | Variable | No | Absent | Absent | No spontaneous healing |
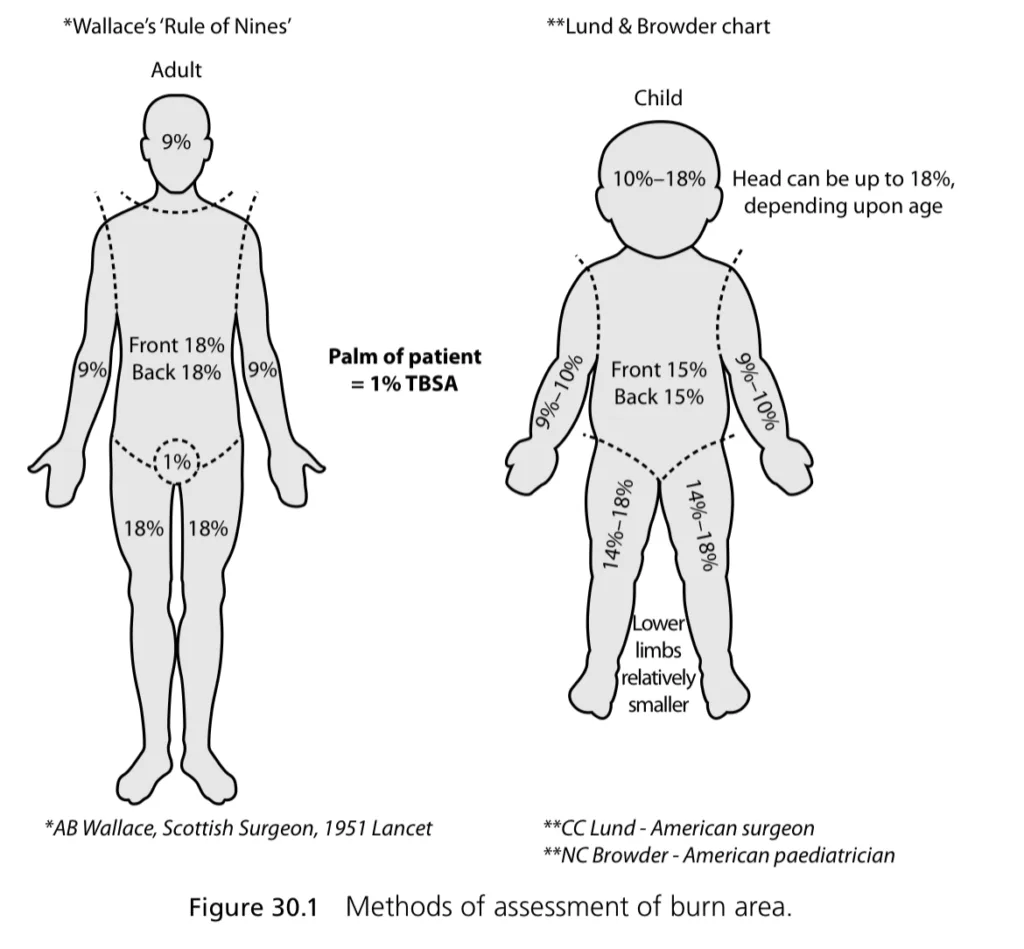
Classification of burn according to extent
Superficial burns are not included in this calculation
- Rule of 9s adults
- Entire head: 9%
- Entire left arm: 9%
- Entire right arm: 9%
- Chest front and back: 18%
- Abdomen front and back: 18%
- Entire left leg: 18%
- Entire right leg: 18%
- Perineum: 1%
- Palm: 1%
- Modified Rule of 9s children
- Entire head: 18%
- Entire left arm: 9%
- Entire right arm: 9%
- Chest + back: 9%
- Abdomen + buttocks: 9% + 9% = 18%
- Left leg (ant, post): 13.5%
- Right leg (ant, post): 13.5%
- Perineum: 1%
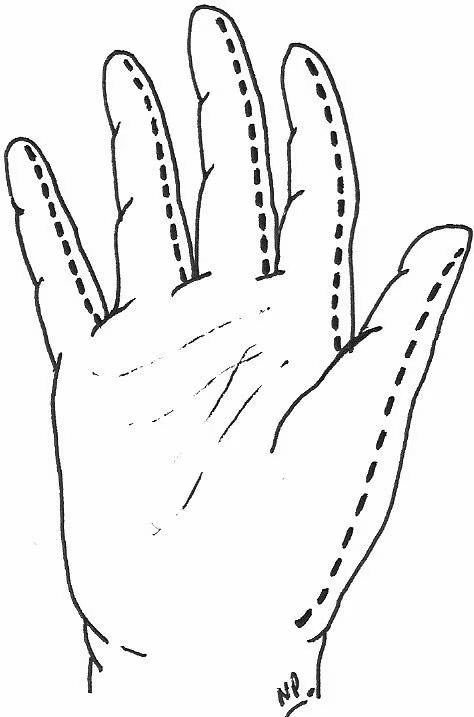
- Rule of palms
- 1% BSA is represented by the patient palms (including the fingers)
- Airway burn
- Represent 10% TBSA
Classification of burns according to severity
- Minor burn injury
- Second degree burn of <15% TBSA in adults or <10% in children
- Third degree burn <2% TBSA not involving special areas (eyes, ears, face, hands, feet, perineum)
- Excludes electrical burns, inhalation injury, concurrent trauma, all poor risk patients (extremes of age, concurrent illness)
- Moderate, uncomplicated burn injury
- Second degree burn of 15-25% TBSA in adults or 10-20% in children
- Third degree burn <10% TBSA not involving special areas (eyes, ears, face, hands, feet, perineum)
- Excludes electrical burns, inhalation injury, concurrent trauma, all poor risk patients (extremes of age, concurrent illness)
- Major burn injury
- Second degree burn of >25% TBSA in adults or >20% in children
- Third degree burn >10% TBSA
- Burns involving special care areas (eyes, ears, face, hands, feet, perineum)
- All electrical burns, inhalation injury, concurrent trauma, all poor risk patients (extremes of age, concurrent illness)
Pre-Hospital Treatment and First Aid
- Pre-hospital treatment
- Assume inhalation injury or CO poisoning and give 100% oxygen
- Assess need for intubation
- IV access and give IV fluids if possible
- Assume as trauma patient and assess for other injuries
- First aid for flame burns
- Remove from flame source and stop the burning process
- Remove involved clothing (synthetic fibers e.g. nylon, polyester, raynon burn rapidly and melt into skin, continuing to burn)
- Douse with running water for 20 minutes (beware of hypothermia in infants, young children, and adults >25% TBSA)
- Cover burns with cling wrap to prevent moisture loss
- Cover with clean, dry towel to prevent hypothermia
- Remove from flame source and stop the burning process
- First aid for chemical burns
- If powder, dust off
- Douse with running water
- Do not neutralize (can generate heat)
- First aid for electrical burns
- Survey the scene to ensure no further danger to the rescuer
- Turn off source of power or remove the victim from the source
- Assess whether CPR is required
Outpatient management
Outpatient management is reserved for burns that cover <10% BSA (<5% in children and elderly) and no third-degree burns. Tx involves disinfection, dressing, and pain management. Inpatient observation overnight is recommended for patients with comorbidities that make healing difficult e.g. Diabetes
- Treatment of first-degree burns
- Non-adherent dressing
- NSAIDS
- Treatment of second-degree burns
- Cleaning
- Do not deroof
- Topical agents: Silver-sulfadiazine or Triple cream ointment (for facial burns)
- Dressing (should be changed daily)
- NSAIDS
- Treatment if fever or worsening of erythema/pain (cellulitis)
- PO antistaphylococcal penicillin (dicloxacillin) or 1st gen cephalosporin (cephalexin)
Hospital Management of Burns
Management of burns takes place in 3 stages
- Primary survey and Resuscitation- Onset of injury to completion of fluid resuscitation
- Acute phase– Beginning of diuresis to near completion of wound closure
- Long-term management (Rehabilitation/Reconstruction)- from major wound closure to return of individual’s optimal level of physical and psychosocial adjustment
- Resuscitation
- Prevention of shock
- Prevention of respiratory distress
- Detection and prevention of concomitant injury
- Wound assessment and initial wound care
- Acute phase
- Wound care and closure
- Blood Transfusion
- Pain control
- Antimicrobial therapy
- Nutritional support
- Prevention or treatment of complications including infections
- Rehabilitation/Reconstruction
- Prevention of scarring and contractures
- Physical, occupational and vocational rehabilitation
- Functional and cosmetic reconstruction
- Psychological reconstruction
Indications for Admission
- Indications for admission (to burn center)
- Partial thickness burns > 10-15% in teens and adults
- Partial thickness burns > 5-10% in children and elderly
- Full-thickness burns > 2%
- Partial thickness and Full-thickness burns involving the face, hands, perineum, or feet; cross a major joint; or circumferential
- Significant electrical burns
- Significant chemical burns
- Inhalation injury
- Other criteria
- Patient with significant comorbidities e.g. Diabetes, Renal Failure
- Patients with concomitant trauma e.g. Fracture
- Very young (< 5 years) or very old (>55 years)
- Psychiatric patients where wound care may be a challege
- Non-compliant patients
- Patients with suspected or known history of drug abuse
- Patients who may not be safe at home (suspected abuse)
Primary Survey and Resuscitation
- Airway and Breathing
- Upper airway injury (above the glottis). Patients who have inhaled smoke or superheated air (leading to laryngeal edema) may have respiratory compromise and require early endotracheal or nasotracheal injury intubation. Delayed intubation→ difficult because of swelling. If delayed → emergency cricothyroidotomy
- Lower airway injury (below the glottis). Assess for expectoration of sputum with carbonaceous particles. Fiberoptic Bronchoscopy to look for damage to the respiratory tract
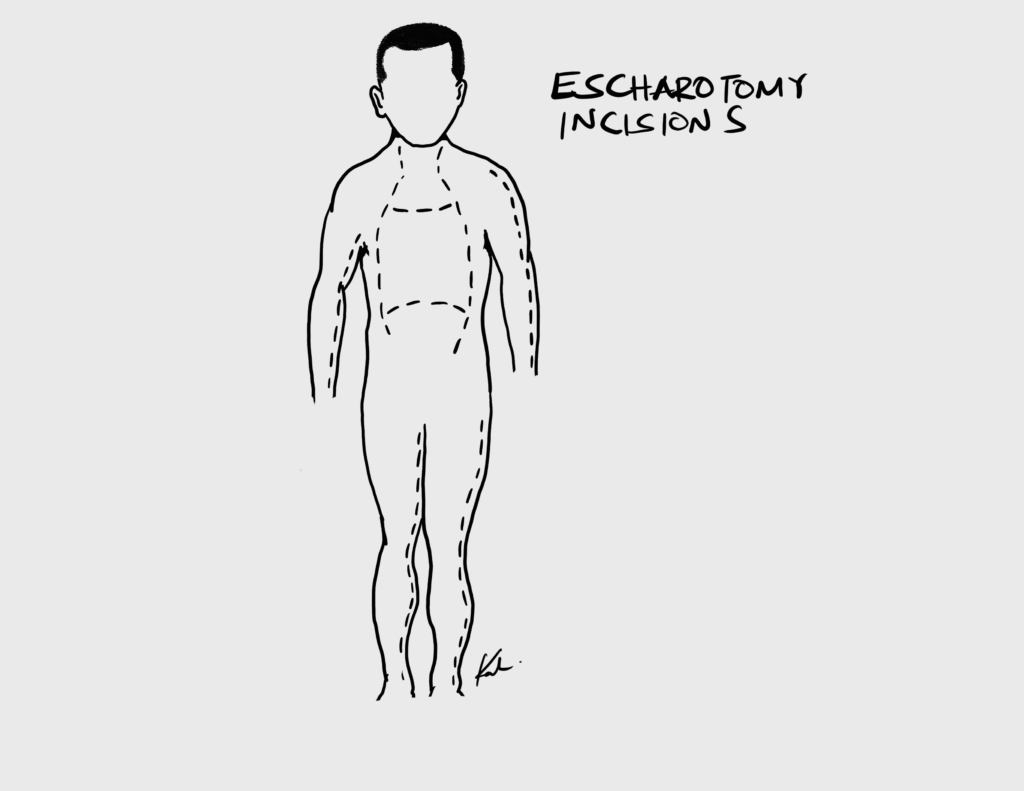
- Circumferential burns around the neck and chest: Escharotomy
- Carbon monoxide poisoning: early intubation with supplemental 100% oxygen. Nasal cannula OR NRB (Smoke exposure. To displace CO)
- Circulation
- Establish venous access points: For obtaining labs and fluid resuscitation (16 G needles to get the fluids in as quick as possible)
- **Fluid resuscitation with RL (**in adults with >10% TBSA or children with > 15 % TBSA; RL buffers acidosis). 1/2 volume of resuscitation fluid is given in the first 8 hours, and the remaining half over the next 16 hours. RL is preferred over hypertonic saline/human albumin/colloid resuscitation.
- Children: 24H of RL (3mL x TBSA X weight in kg) → 24H of maintenance D5RL (4 -2 – 1 rule for maintenance requirements)
- Adults: 24H of RL calculated by ATLS/Parkland recommendations
- Disability
- Evaluate for possibility head injury and spinal cord injury
- Exposure
- Expose and assess total body surface area
- Remove jewelery, rings, amultes, and necklaces
- Use warmers and blankets to prevent heat loss, and cover all burns as soon as possible
- Adjuncts
- Labs: CBC, BMP, GXM, Carboxyhemoglobin, CXR (Respiratory burns), EKG, Cardiac Enzymes (Electrical burns)
- Foley catheter: Get Urinary sample for myoglobin, measure urine output (0.5 – 1mL/kg in adults, 1mL/kg in paeds)
- NG tube: decompressing the GI tract since >20% BSA can develop ileus
- Pulse oximetry (respiratory burns or exposure to fire CO can have falsely elevated O2 sat. Get carboxyhemoglobin level and subtract)
- CO oximetry
- Tetanus toxoid
- Remove jewelery
- Investigations
- CBC with differenital, RBS, U/E/Cs (possibility of myoglobinemia), GXM, Toxicology screen, Septic screen (blood culture, urine culture),
- Electrical burns: EKG, Cardiac enzymes, urine myoglobin, CT head if LOC
- Respiratory burns: Carboxyhemoglobin, CXR, ABGs, Cardiac enzymes, EKG
- Any other tests depending on co-existing injuries
Calculating fluid resuscitation
Formulas can be used to calculate additional fluid needed (Lactated Ringers) for burn patients and should be added to maintenance fluid (2L D5W over 2 days) if necessary. >15% TBSA will need resuscitation because of third spacing. Max % burn area used for the formula is 50%. 2nd and 3rd-degree burns have some level of edema and will also require resuscitation.
Adequate resuscitation should be matched with a urine output of 1-1.5ml/kg and an adequate MAP. Paediatric patients should also receive sugar containing fluid at their calculated maintenance rate due to a risk of hypoglycemia.
Parkland formula for adults: V = (% area burn) x (kg weight) x (4 ml/kg)
ATLS recommendation for adults V = (% area burn) x (kg weight). x (2ml/kg)
ATLS recommendation for paediatrics: V = (% area burn) x (kg weight) x (3ml/kg)
ATLS recommendations for electrical burns: V = (% area burn) x (kg weight) x (4ml/kg)
- Administration
- 1/2V over the first 8 hours
- 1/2 V over the remaining 16 hours
Wound management
Wounds should be cleaned and small blisters kept (acts as biological dressing). Early excision and grafting (within 1 week) is beneficial for deep partial thickness and full thickness burns. Burns that do not heal within three weeks should be treated surgically. Topical agents including Silver sulfadiazine and Mafenide acetate, and dressing can be used. Escharotomy can be performed during debridement for burns in the chest, and upper and lower exremities to prevent compartment syndrome. Fasciotomy is performed if compartment syndrome develops.
- Goals for topical burn care
- Protect damaged skin
- Prevent heat loss
- Maintain appropriate functional positioning by splinting
- Provide comfort and reduce pain
- Treatment for 2nd and 3rd degree burns with no eschar present
- 1% Silver sulphadiazine
- 0.5% silver nitrate cream
- Early excision and grafting
- Treatment for burns with eschar
- Mafenide acetate
- Escharectomy during debridement
- Treatment for Burns to the face
- Triple antibiotic ointment – Neosporin (bacitracin, neomycin, polymixin B)
- Wound coverage
- Autografts (split-thickness and full-thickness)
- Acellular dermal matrix (Alloderm, Xenoderm)
- Engineered synthetic dermal substitutes (integra)
Escharotomy incisions
| Location | Incision |
|---|---|
| Upper limb | MAL. Anterior to elbow medially to avoid the ulnar nerve |
| Hand | Midline in the digits. Release muscle compartment if tight |
| Lower limb | MAL. Posterior to the ankle medially to avoid the saphenous vein |
| Chest | Down the chest lateral to the nipples. Across the chest below the clavicle. Across the chest at the level of the xiphisternum |
| General rules | Extend the wound beyond the deep burn. Diathermy any significant bleeding vessels. Apply haemostatic dressing and elevate the limb post-op |
Pain Control, Nutrition, and Blood Transfusion
- Pain control A combination of pharmacological and non-pharmacological techniques
- First and second degree burns that are treated as outpatient: discharge with NSAIDs
- Severe burns: IV opiates (morphine, fentanyl, oxycodone). Transition to oral opiates then NSAIDs
- Multimodal analgesia (use of several drugs in combination)
- Non pharmacological strategies:
- Relaxation tapes
- Visualisation, guided imagery
- Meditation
- Music
- Nutrition
- Burn patients are catabolic.
- Very early enteral feeding is recommended. An NG tube is indicated for all patients with burns > 15% TBSA
- TPN can be given using a central line if enteral feeding is not tolerated
- Calculating nutritional requirment
- Indirect Calorimerty (IC) is the gold standard for assessing nutritional requirment
- Other formulas: Harris-Benedict, Curreri, Ireton-jones, and Toronto can be used to calculate nutritional requirments. Their disadvantage is that the underfeed in the early periods of highest energy use and overfeed in the later periods
- Nutrition Sutherland formula
- Children: 60 kcal/ kg + 35 kcal %TBSA
- Adults: 20 kcal/ kg + 70 kcal %TBSA
- 1.5- 2g/ kg of protein per day
- Protein 20% of energy requirements
- Burn patients are catabolic.
- Blood Transfusion
- Blood transfusion
- Transfusion is restricted to Hb concentrations of 7-8 g/dL in patients without other indications for blood transfusion e.g. ongoing bleeding
- Techniques that reduce transfusion rates:
- Tourniquets during excision and/or grafting of an extremity to reduce blood loss
- Epinephrine Tumescence: Intradermal cysis or tumescence with a vasoconstricting agent (epinephrine and phenylephrine).
- Combination of above techniques
- Blood transfusion
Long-term management (Rehabilitation/Reconstruction)
Plastic or cosmetic surgery is performed for burns that are disfiguring and debilitating.
- Risk factors for contracture formation
- Burn across a joint
- Burn depth (≥ third degree)
- Risk factors for hypertrophic scars
- Scars that result from healing by secondary intention
- Scars which are subject to tension in two dimensions after primary closure
- N.B: affect the young, rather than the elderly, and females more than males. The anterior chest, shoulders and deltoid regions are particularly predisposed
- Reporting a contracture
- Location and joint involved
- Joint position (extension, flexion, adduction etc.)
- Degree of contracture
- Fixed or flexible contracture (caused by bony or Soft tissue changes respectively)
- Active wounds over the contracture
- Prevention of contractures
- Early excision and grafting
- Early splinting in extension
- Infection control to prevent full-thickness skin loss
- Physiotherapy
- Pressure garments
- Scar massage
Special management for non-thermal burns
Chemical burns
Acid Vs. Alkaline burns
| Acidic burns | Alkaline burns | |
|---|---|---|
| Mechanism | Protein injury by hydrolysis, thermal burn on skin contact | Saponification of fat→ hygroscopic effect (dehydrates cells), dissolves proteins by creation of alkaline proteinates |
| Type of necrosis | Coagulative necrosis | Liquefactive necrosis |
| Depth | Shallower burns than alkaline burns | Deeper burns than acidic burns |
- What is an important concern in patients with phosphorus burns (”white phosphorus munition”)?
- Phosphorus can be absorbed leading to hypocalcemia and arrhythmias
- Treatment of Chemical burns
- Copious irrigation with tap water ASAP (DO NOT play chemist and try to neutralize the burn)
- Phenol burn – can use PEG (polyethylglutamate)
- HCl burn – can use calcium gluconate in petroleum jelly
Electrical burns
The severity of electrical burns is determined by the voltage and ambient conditions (wet vs. dry conditions). Muscles and nerves are most at risk as they offer most resistance.
- Investigations
- EKG is mandatory! (arrhythmogenic complications of electrical exposure)
- Treatment
- Diuresis
- Anti-arrhythmics
- Fasciotomy (compartment syndrome can rapidly develop)
Complications of burns
Common causes of death in burns patients include shock, sepsis and respiratory failure
- Acute (early) complications of burns (48-72h)
- Hypothermia
- Shock
- Sepsis (Common causative organisms include S.aureus (including MRSA), Enterococcus, and Pseudomonas)
- Respiratory failure (ARDS)
- Multi-organ failur (e.g. Renal failure)
- Sub-acute (intermediate) complications of burns
- DVT
- Post-burn hypermetabolism
- Malnutrition (hypoproteinemia)
- Curling ulcers
- Paralytic ileus
- Infection (wound infection, hypostatic pneumonia)
- Anemia
- Chronic complications of burns
- Hypertrophic scars
- Keloid formation
- Contractures
- Marjolin ulcer (Tx is wide excision or amputation)
- Psychological problems
- Complication of chemical burns
- Eyes: Cataracts or vision loss
- Esophagus: Strictures
- Systemic poisoning
- Complication of electrical burns
- Arrhythmia
- Myoglobinuria → Renal failure
- Rhabdomyolysis
