Anatomy
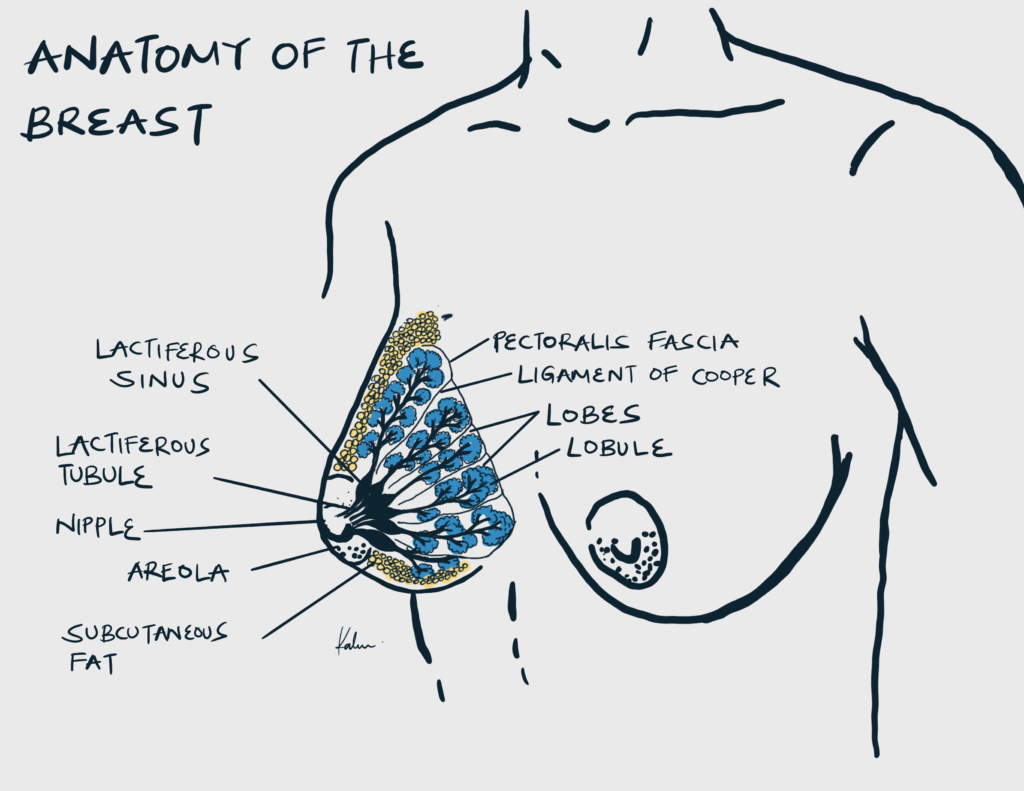
Boundaries of the breast
| Boundary | Structure |
|---|---|
| Superior | Second or third rib |
| Inferior | Inframammary fold at the sixth or seventh rib |
| Medial | Lateral border of the sternum |
| Lateral | Anterior axillary line, axillary tail of spence extends laterally across the anterior axillary fold |
| Deep | Fascia of pectoralis major, serratus anterior and external oblique |
| Superficial | Subdermal fat then dermis overlying the skin |
Important anatomical structures of the breast
| Structure | Relevance |
|---|---|
| Inframammary fold | Predilection to Candidiasis in women with large breasts |
| Tail of spence | Important to understand that it is an extension of breast tissue to the shoulder. 50% of breast cancers occur here |
| Region of axillary lymph nodes | Common region for metastasis |
| Suspensory ligaments of cooper | Causes the skin to take on a dimpling appearance in inflammatory carcinoma, since the skin remains tethered to the ligaments in the presence of swelling |
| Adipose tissue | Gives breasts its size |
| Batson’s plexus | A venous system surrounding the vertebral column that connects other body areas including the breast. Represents a route for distant metastasis to the spine |
Alveoli vs Lobules vs Lobes
| Alveoli | 10 – 100 per lobule |
|---|---|
| Lobules | 10 – 20 per lobe |
| Lobes | 15 – 20 per brest |
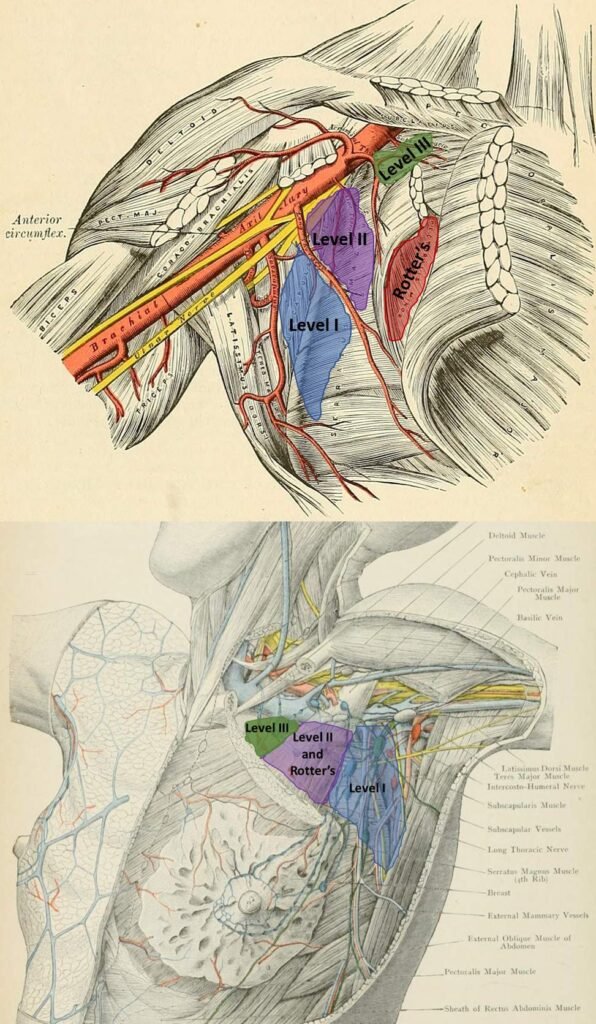
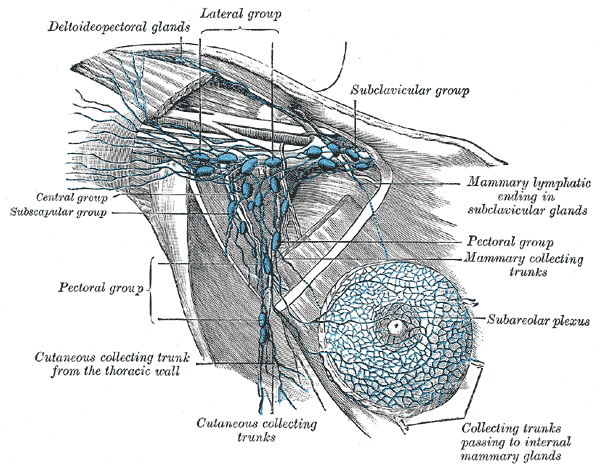
Lymph node levels of the axilla (relative to pectoralis minor)
| Level | Location relative to pectoralis minor |
|---|---|
| Level I | Lateral to pectoralis minor |
| Level II | Deep to pectoralis minor |
| Level III | Medial to pectoralis minor |
| Rotter’s nodes | Superficial to pectoralis minor (interpectoral – between pectoralis minor and pectoralis major) |
Evaluation of the Breast
Triple assessment of a breast mass involves a clinical breast exam, radiography (imaging), and histopathology (core-needle biopsy or fine needle aspiration for cystic masses).
SBE vs CBE
| Self-breast Examination | Performed at home by the patient as a means of detecting massess. Conflicting evidence on its efficacy in improving survival. |
|---|---|
| Clinical breast examination | Performed in hospital by a medical doctor as the primary means for diagnosing breast massess. |
- Patient History
- Presenting complaint
- Duration and onset
- Changes to the breast or nipple e.g. discharge, skin retraction, new nipple inversion, whether unilateral or bilateral
- Cyclical associations
- Any aggravating or relieving factors
- Past Medical, Surgical and Family History
- Previous breast disease
- Biopsies
- Cancer
- Recent breast trauma
- Prior chest radiation
- Other medical conditions and previous surgeries
- History in first-degree relatives of breast disease, colon, ovarian, prostate, or pancreatic cancer
- Estrogen exposure and Gynaecologic history
- Estrogen exposure
- Age at menopause (if applicable)
- Parity
- Oral contraception or hormone replacement therapy use
- Presenting complaint
- Physical examination
- General appearance for weight loss and cachexia
- Examination of the breast
- Inspection
- Hands against hips and arms up position
- If abnormalities, ask how long the abnormalities has been there for
- Size
- Skin:
- Colour should be consistent
- Surface should be smooth.
- Areolar surface should be similar on both sides.
- Nipples normally everted (occasional inversion…look for symmetry)
- Symmetry: should be roughly symmetrical (look both planes)
- Palpation
- Supine position. Get chaperone. Might want to keep only one breast exposed.
- Gently palpate starting on the periphery moving inwards in a circular pattern (clock pattern) Use both hands; index finger and thumb. Don’t “pinch” unless you’re discerning a mass or trying to express from the nipple.
- Remember to palpate the tail of spence (region from breast to tissue)
- Palpate axillary LNs and supraclavicular
- Manipulate the nipple for expression (if patient obliges)
- Inspection
- Abdominal exam for distension (ascites), masses, hepatomegaly, discomfort on palpation
- Bony exam for pain or tenderness to palpation of the spine
- Cardiopulmonary exam in patients whom surgery may be considered
- 5 D’s for breast evaluation abnormalities
- Discoloration: may be normal during pregnancy
- Dermatologic sign: orange skin changes (Peau d’ orange, orange peeling)
- Depressed nipple: Inverted nipple
- Deviation: of one breast relative to another
- Discharge: from nipple
- When should a routine mammogram be performed?
- A routine mammogram is recommended for all women starting at age 45 and then every year thereafter such that the patient is in good health (no mass that requires diagnostic mammography)
- Women of average risk may transition to every other year after age 54
- If a woman has a relative who developed cancer, the woman should begin getting the mammogram at the age that is 5 years younger than the relative who had cancer
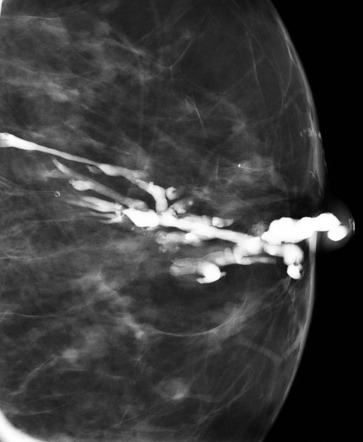
- Imaging
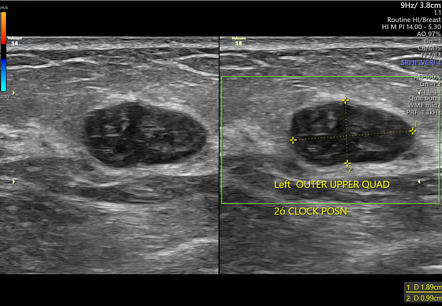
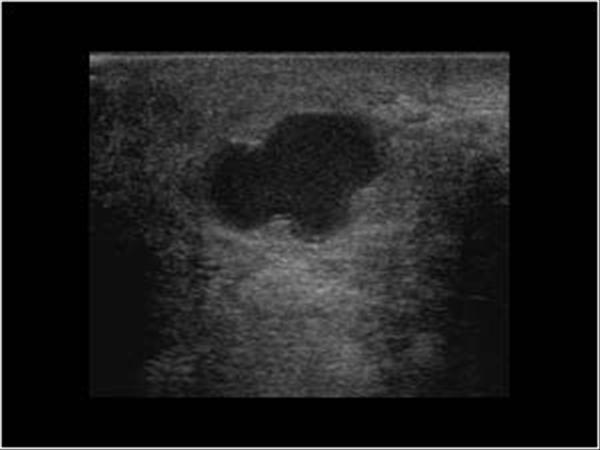
- Ultrasound: for screening women under 40 or of any age with dense breast
- Mammography: for screening women over 40. Reported in BI-RADS.
- BI-RADS 2 nothing to do
- BI-RADS 3 wait and see (repeat imaging)
- BI-RADS 4 needs a core (biopsy)
- MRI: most sensitive but high false positive rates. Assess response to neoadjuvant tchemotherapy, detect primary tumors and screening in young women with high genetic risk.
- CT/bone scintigraphy/PET(CT): for patients with signs and symptoms of metastasis
- Biopsy techinques
- Core needle biopsy: preferred method. Sample can be taken for immunohistochemistry
- Fine needle aspiration (FNA): diagnose breast cancer but cannot evaluate invasion
- Excisional biopsy (reserved for discordant results – core biopsy does not match imaging findings)
BI-RADS scoring system
| BI-RADS score | Description |
|---|---|
| 0 | Needs additional imaging |
| 1 | Normal |
| 2 | Benign |
| 3 | Probably benign, but close follow-up and re-imaging in 3-6 months needed, < 2% risk of malignancy |
| 4 | suspicious abnormality, biopsy warranted |
| 5 | highly suggestive of malignancy (>95% likelihood) |
| 6 | imaging in known malignancy (biopsy proven) |
Benign & Semi-Benign breast disease
Aberrations of normal breast development and involution (ANDI)
| Developmental stage | Normal effects | Abnormal effects |
|---|---|---|
| Development and maturation | Lobular growth and hypertrophy, stromal growth and hypertrophy, nipple enlargement and eversion | Fibroadenoma, giant fibroadenoma, adolescent hypertrophy, gigantomastia, nipple inversion that may lead to subareolar abscesses and fistulae |
| Cyclical and Lactational | Cyclical menstrual changes, lobular and ductal hyperplasia of pregnancy | Cyclical mastalgia, breast nodularity or cysts and macrocysts, bloody nipple discharge |
| Postmenopausal involution | Lobular and ductal involution, epithelial turnover | Sclerosing lesions, ductal ectasia, epithelial hyperplasia with or without atypia |
- List five benign breast conditions that present with a palpable breast lump
- Non-proliferative breast disease
- Simple cysts of the breast
- Proliferative lesions without atypia
- Fibroadenoma and phyllodes tumor
- Ductal hyperplasia without atypia
- Intraductal papilloma
- Sclerosing adenosis
- Radial scar
- Atypical hyperplasia
- Atypical ductal hyperplasia
- Atypical lobular hyperplasia
- Infectious and inflammatory conditions
- Mastitis and abscesses
- Mammary tuberculosis
- Idiopathic granulomatous mastitis
- Mondor’s disease
- Fat necrosis
- Gynaecomastia
- Non-proliferative breast disease
Fibroadenoma
Well-defined benign stromal tumor of the breast occurring most often in younger women (<35 yo)
- Signs and symptoms
- Painless mass in breast
- Physical exam
- Well-defined, MOBILE, firm, rubbery mass
- Rarely bigger than a golf ball (< 4cm)
- Bilateral (25% of the case – check the other breast)
- Investigation
- Sonography: Best initial (for women < 35y; have denser breast and isn’t good for mammography. Range of cutoff is usually 30-40y)
- FNAC: for cytological analysis (when you suspect the mass is benign)
- Stereotactic core biopsy or Excisional biopsy: accepatbale if the pt is on the older end (usually done when you suspect the mass is malignant)
- Treatment
- Elective resection
Giant juvenile fibroadenoma
A variant of fibroadenoma found in pre-pubertal or young teenage girls. Grows faster than a fibroadenoma. Gets bigger than a fibroadenoma. May distort the development of the breast.
- Patient history
- Young girl w/breast mass that’s getting bigger
- Physical exam
- Similar to fibroadenoma (well-defined, firm, MOBILE, rubbery mass)
- More obvious
- Investigations
- Sonography
- FNAC
- Treatment
- Always surgically excised (preferably with help of a plastic surgeon)
Cystosarcoma phylloides (Phylloides Tumor)
A large variant of fibroadenoma seen in women in their 30s-40s (May occur in any age). Can get really big. Semi-benign tumor (Benign 85-90% of the cases, Few develop into highly deadly sarcoma). May metastasize through the bloodstream. Not cystic. Dx is clinical.
- Signs and symptoms
- Large breast mass that continues to grow relentlessly
- Physical exam
- Obvious breast mass (much bigger than fibroadenoma)
- The overlying skin is warm, shiny and erythematous
- Treatment
- Wide local excision and biopsy for cellular atypia (r/o Sarcoma)

Fibrocystic change (mammary dysplasia)
Very common in most women of child-bearing age – consider it a norm. Small nodular masses (painless, feel like grains of rice). May be tender in week 3 – 4 of her ovulatory cycle (pt says it happens “when I’m about to have my period” → progesterone peak). Thought to be an exaggerated response of the breast stroma to hormones.
- Signs and symptoms
- Lumps in the breast that have been there for some time
- Occasionally Painful
- Physical exam
- Several nodules appreciated in breast tissue
- Bilateral
- May or may not be tender
- < 1cm in diameter
- Investigations to r/o other causes
- Ultrasound
- Mammography
- Consider FNAC is mass grows to >1cm
- Treatment
- Observation
- Patient education
- Supportive:
- Avoid trauma
- Support bras
- OCPs (disrupt menstrual cycle)
Intraductal papilloma
The most common cause of bloody nipple discharge (serosanguinous discharge) – almost identical to papillary carcinoma which is much rare. Benign tumor involving the linings of the lactiferous ducts. Affects pre-menopausal women. Little malignant potential
- Patient history
- Premenopausal women presenting with bleeding from her nipple
- Physical exam
- Serosanguinous fluid expressed from the nipple (sent to cytology)
- Investigations
- Mammography: r/o breast ca. Papilloma is small and won’t be seen
- Treatment
- Surgical excision of involved ducts (Galactogram for guidance)
Breast abscess
Abscess of breast tissue. Common in women post-partum and/or breastfeeding. Breast cancer until proven otherwise if pt is not a new mom and presents with breast tenderness.
- Patient History
- Previously diagnosed with mastitis
- Signs and symptoms
- breast tenderness
- Physical exam
- Warm, tender, fluctuant mass
- Commonly beneath the areola or peri-areola
- LAN or nipple inversion
- Systemic symptoms of infection
- Investigation
- Ultrasound: multilobulated, hypoechoic (hyperechoic is pus)
- Treatment
- Incision and drainage
- Biopsy of the wall
- Culture of the pus
- Anti-staph antibiotics (nafcillin, oxacillin)

Breast cysts
Most common breast masses. Various causes. Usually painless.
Macrocysts: palpable
Microcysts: non-palpable and are part of cyclic nodularity
- Investigation
- Ultrasound:
- cyst wall
- hypoechoic
- FNAC/ Needle drainage
- Clear or greenish: simple cyst, benign, no further steps necessary
- Milky: galactocele, benign, no further steps necessary
- Bloody: May be malignant, refer for local excision
- Ultrasound:
- Treatment
- Local excision (if bloody aspirate or recurrent or painful or growing )

Mammary duct ectasia
Blockage of the mammary duct → Dilated duct
Plasma cell inflammation → pain and nipple discharge
- Patient History
- An older lady (peri/post-menopausal) who presents with breast pain and sticky nipple discharge
- Signs and symptoms
- Breast pain
- Nipple retraction
- Subalveolar mass
- Sticky discharge expressed from the nipple (color may vary)
- Investigation
- Mammography: The age of these women puts them at risk of duct ectasia
- Treatment
- Excisional biopsy
Malignant breast disease
Breast cancer is the most common cancer in women and the second leading cancer killer in women (after lung cancer). 1 in 8 women will be diagnosed with breast cancer in her life. 99% of cases are in women. Men can also get breast cancer.
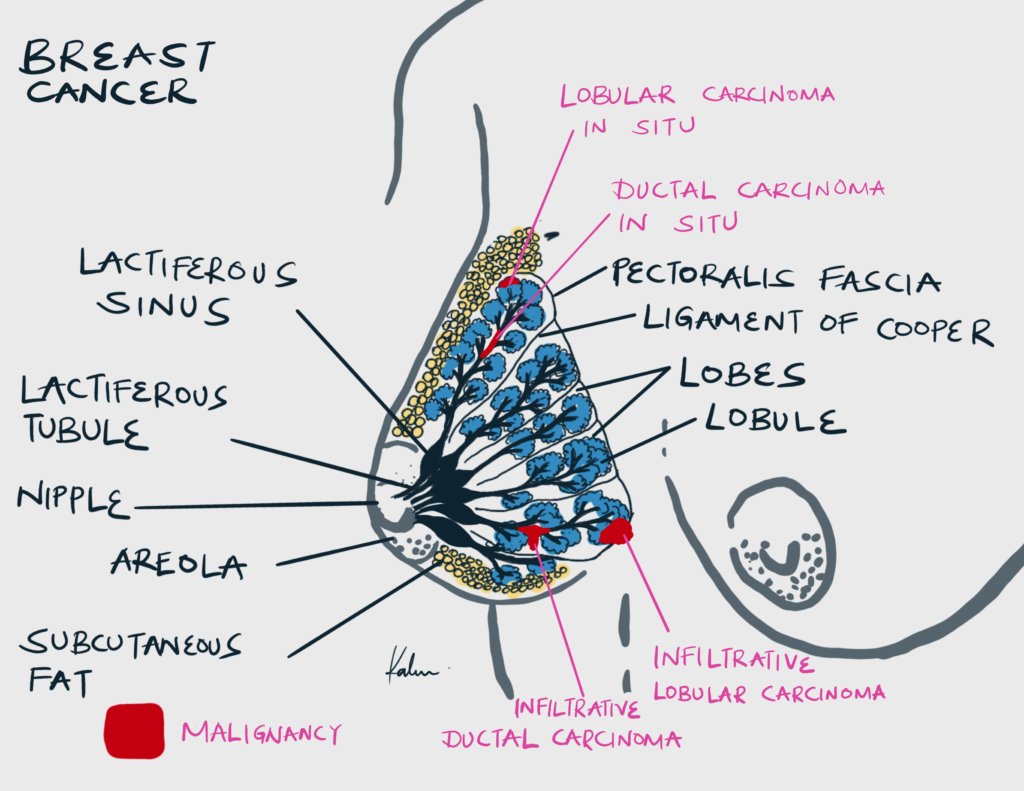
| Non-invasive breast cancer | Ductal Carcinoma In Situ, Lobular Carcinoma In Situ |
|---|---|
| Invasive breast cancer | Invasive Ductal Carcinoma, Invasive Lobular Carcinoma |
- Risk factors
- Female sex
- Older age (>40)
- Hx of breast cancer
- FHx of breast cancer
- Nulliparity
- Obesity
- Hypertension and Diabetes
- Chronic stress
- Living in a cold climate
- Race (White women more likely to get breast cancer, Black women more likely to have aggressive triple-negative breast cancer)
- Obstetric and Gynaecologic factors associated with breast cancer
- Early menarche
- Late menopause
- FHx of Gynecological malignancies
- OCPs (debatable)
- Genetic mutations associated with breast cancer
- BRCA1 and BRCA2 mutations (needs genetic testing)
- Li-Fraumeni syndrome (p53 mutation associated with breast, sarcomas, brain, and adrenal tumors)
Likelihood of developing breast cancer
| Primary relative with bilateral breast cancer, premenopausal | 8.8 x more likely |
|---|---|
| Primary relative with bilateral breast cancer, postmenopausal | 4x more likely |
| Primary relative with unilateral breast cancer, premenopausal | 1.8x more likely |
| Primary relative with unilateral breast cancer, post-menopausal | 1.2x more likely |
- Suspicious findings in clinical/self breast exam
- Ill-defined mass
- Fixed mass, esp attached to chest wall
- Overlying skin changes
- Orange peeling (seen in advanced inflammatory breast ca)
- Dimpling (d/t compromised suspensory ligaments of cooper)
- Erythema (d/t local invasion)
- Nipple retraction
- Axillary Lymphadenoapthy
- Investigations (Triple-assessment)
- Clinical breast exam
- Imaging
- Mammography = best initial step in woman >35 years (most women will be over the age of 35). Look for calcifications. Hard to see in the dense breasts of younger women.
- Sonography = for women in < 35 years
- Pathology
- Stereotactic Core Needle Biopsy
- FNAC (for tumors that you suspect to be benign or cystic)
- Prognostic factors for breast cancer survival
- Stage at diagnosis
- Tumor size
- Lymph node involvement
- Histological tumor grade
- Receptor status**:**
- Hormone-negative breast cancer has a poorer prognosis than hormone-positive breast cancer.
- HER2-positive tumors show aggressive growth and metastasize quickly compared to HER2-negative tumors.
- Triple-negative disease is associated with a poor prognosis.
- Advanced age
- Aneuploidy

Axillary lymph node groups
| Group | Nodes |
|---|---|
| Group I | Pectoral, Subscapular, Brachial |
| Group II | Interpectoral, Central |
| Group III | Apical, Supraclavicular |
Treatment strategies
Surgical treatment will always include sentinel node biopsy. Breast conservation therapy and Modified Radical Mastectomy (MRM) have equal survival outcomes. However, MRM has a lower recurrence likelihood. Hormonal therapy has an equal efficacy to chemotherapy in post-menopausal patients (Keep in mind that older women may not be able to tolerate chemotherapy). In women with very large breast cancer, pre-op radiation and chemotherapy are performed to shrink the cancer.
Treatment options
| Treatment option | Description | Nota bene |
|---|---|---|
| Breast conservation Therapy (BCT) | Lumpectomy with histologically clear margins, Sentinel node biopsy (+/- axillary dissection), Post-op Radiation | For single lump < 2cm in size and well-differentiated histology |
| Simple Mastectomy | Removal of skin, breast tissue and nipple areolar complex, breast reconstruction | |
| Skin-sparing mastectomy | Removal of breast tissue and nipple-areolar complex. Skin is preserved for reconstruction | |
| Nipple-sparing mastectomy | Removal of breast tissue only before reconstruction. The nipple-areolar complex is preserved. | |
| Modified Radical Mastectomy (MRM) | Removal of breast tissue and nipple/areolar complex, Axillary dissection, Breast reconstruction | For early localized growth < 5cm |
| Radical Mastectomy | Removal of breast tissue, nipple/areolar complex, pectoralis muscles, Axillary dissection | For tumor that invades the chest wall |
| Palliative simple mastectomy | Removal of the entire breast and surrounding skin after assessing resectability and skin closure | For locally advanced cancer without distant metastasis |
| Radiation therapy | Brachytherapy, External beam, Proton beam | For patients undergoing breast conservation; For patients with high risk of recurrence |
| Neoadjuvant chemotherapy | Administered before surgery to shrink the tumor and reduce the risk of metastatic spread | |
| Chemotherapy | For patients with positive lymph node status and/or metastasis, and administered after surgery to reduce the risk of metastatic spread. | 5-FU, Adriamycin/MTX, Cyclophosphamide – CAF/CMF |
| Hormonal therapy | Lestrozole, Anastrozole, Tamoxifen, Raloxifene | For ER+/PR+ patients; |
| Biological therapy | Trastuzumab | For Her2/neu+ patients; |
- Treatment of DCIS or LCIS
- Breast conservation therapy (BCT)
- Modified Radical Mastectomy (MRM)
- Treatment of Metastatic Breast Cancer
- Modified Radical Mastectomy (MRM)
- Chemotherapy
- Radiation therapy
- Hormonal Therapy
- Biological Therapy
Ductal Carcinoma in situ (DCIS)
Carcinoma confined to ductal tissue w/o invasion of the basement membrane
- Treatment
- BCT
- MRM
- Is chemotherapy necessary for in situ carcinoma?
- No…BUT a lot of women get them at the call of the surgeon/oncologist
Recurrence
| Treatment | Recurrence |
|---|---|
| Lumpectomy alone | 25% (and may be invasive) |
| Lumpectomy + radiation | 8% |
| Modified Radical Mastectomy | < 1% |
Lobular carcinoma in situ (LCIS)
Carcinoma confined to lobular tissue w/o invasion of the basement membrane. More commonly an incidental finding in Self or clinical breast exam as it is likely to calcify. Increases the risk of invasive cancer in either breast (bilaterality or recurrence in another breast)
- Treatment
- BCT
- MRM
- Prophylactic bilateral mastectomy should be considered
Infiltrating Ductal Carcinoma
Carcinoma of the ductal cells w/invasion of the basement membrane. Most common “breast cancer” (70% of all diagnoses)
- Investigations to work up for metastases
- CXR: for lung Mets
- CT liver: for liver Mets
- LFTs: for liver Mets not apparent on CT
- Bone scan: for Bone Mets
- CT head: for CNS metastasis if the patient has neurological signs
- Surgical Treatment
- BCT
- MRM
- Radical mastectomy if there is invasion of Pec Major
- Medical Treatment
- Chemotherapy (if there is spread)
- CAF (Cyclophosphamide, Adriamycin, 5-FU)
- CMF (Cyclophosphamide, MTX, 5-FU)
- Hormone therapy (if ER+/PR+)
- Estrogen inhibitors (Tamoxifen, Raloxifene)
- Aromatase inhibitor (Anastrozole)
- Adjunctive therapy
- Trastuzumab/Herceptin (for Her2/Neu+ Breast Ca)
- Chemotherapy (if there is spread)
Infiltrating Lobular Carcinoma
Carcinoma of ductal cells w/invasion of the basement membrane. Workup for mets after dx via biopsy (CXR, CT liver, LFTs, Bone scan). Strong tendency towards bilaterality (20-29%)
- Surgical Treatment
- BCT
- MRM
- Radical mastectomy if there is an invasion of Pec Major
- Medical Treatment
- Chemotherapy (if there is spread)
- CAF (Cyclophosphamide, Adriamycin, 5-FU)
- CMF (Cyclophosphamide, MTX, 5-FU)
- Hormone therapy (if ER+/PR+)
- Estrogen inhibitors (Tamoxifen, Raloxifene)
- Aromatase inhibitor (Anastrozole)
- Chemotherapy (if there is spread)
Inflammatory breast cancer
Aggressive breast cancer variant (1-4%). Presents with Peau d’orange, dimpling, and mets. Poor prognosis.


- Treatment
- Urgent chemotherapy
- MRM
- Radiation to breast and axilla
Infiltrating papillary carcinoma
Very rare breast cancer variant. Include in differential of bloody (serosanguinous) nipple discharge (intraductal papilloma has a similar presentation)
Paget’s disease of the breast
Patient with breast cancer presenting with eczematous dermatitis of the nipple. Signals underlying breast cancer (94%, almost always breast cancer). Best initial dx step is mammography followed by punch biopsy.

Male breast cancer
Possible. Outnumbered 150:1 F: M. Survival by stage is similar to cancers in women.
- Risk factors
- Klinefelter’s syndrome
- High estrogen level
- BRCA2 mutation
Breast cancer in pregnancy
Workup the same way. Different management but no difference in survival.
- Differences in evaluation and treatment
- Mammograms with abdominal shielding
- Do not give radiation during the pregnancy
- Do not give chemotherapy during the first trimester
- Do not give tamoxifen, aromatase inhibitors, or trastuzumab
- SLNB can be performed with radiocolloid but NOT lymphazurin blue due to increased risk of anaphylaxis
- Best to operate in the second trimester with pre- and post-op fetal heart tones. Although operation can be performed at any trimester depending on clinical situation
