Overview
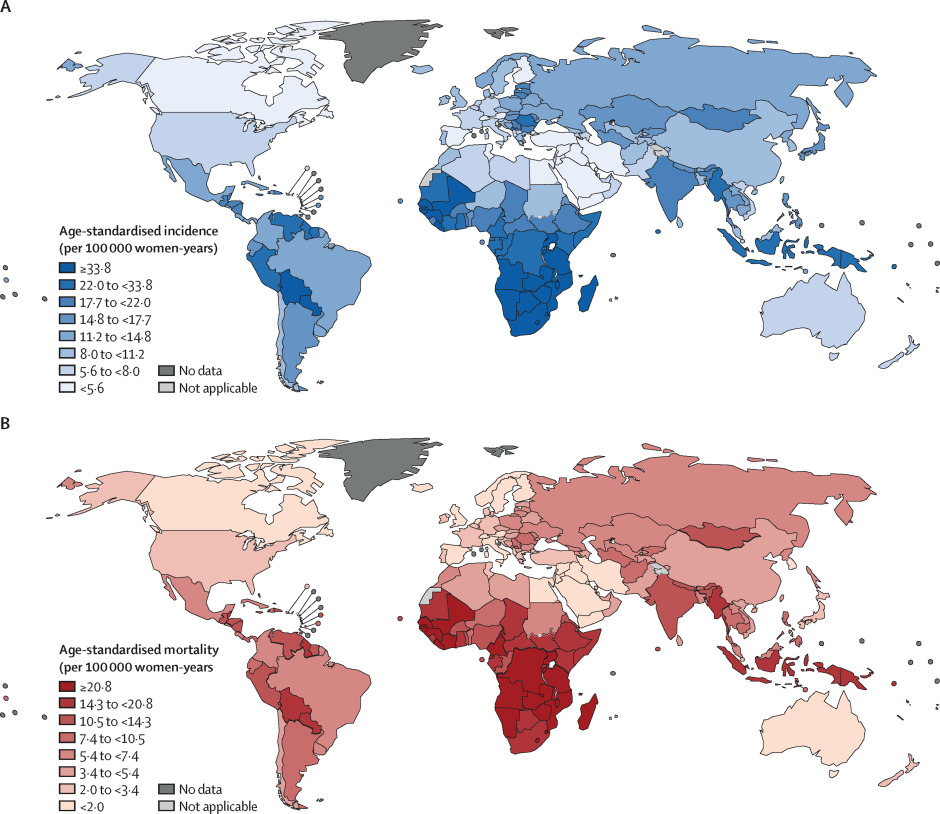
Cervical cancer rates are highest in Sub-saharan Africa. Cervical cancer is the 3rd most common cancer in women worldwide and the 2nd most common cause of cancer-related deaths in women. It contributes to about 13% of new cancer cases annually and 11% of cancer deaths annually in Kenya. It is the leading cause of cancer-related deaths in Kenya and the 2nd most common cancer among women in Kenya. Late-stage cervical cancer presents commonly at 50-79 years of age. The prevalence among women < 40 years is increasing (probably due to sexual promiscuity – increased exposure to high-risk HPV strains).
80% of cervical cancers are SCC. 20% are adenocarcinoma
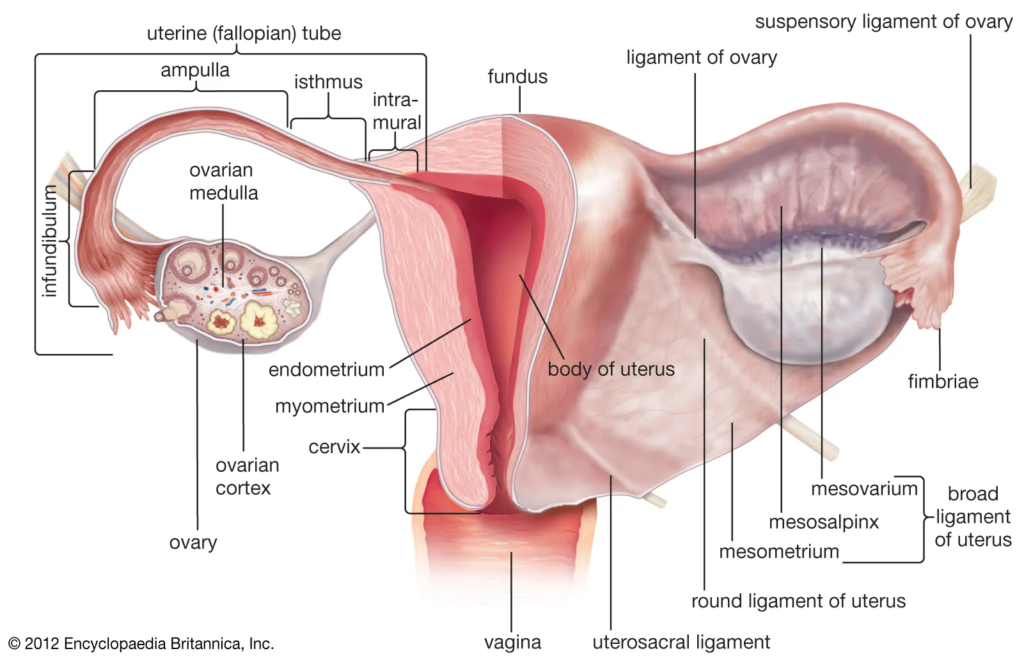
The parametrium is important – parametrial involvement necessitates chemoradiation. The average diameter of the cervix is about 1 cm and the average length is roughly 4 cm.
Human Papillomavirus (HPV)
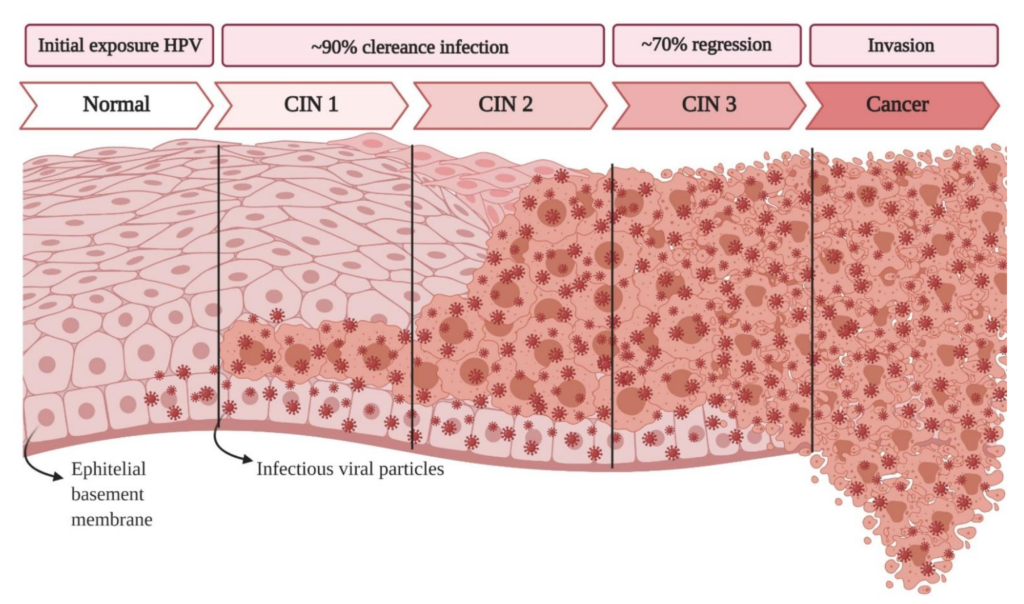
HPV is a DNA virus that has been causally linked to the development of CIN and invasive cancer (as well as other SCCs – anal cancer, vulvar cancer, HNSCCs e.t.c). It inserts its genome into the host genome leading to cancer.
Most HPV infections are cleared within a couple of years of infection. Immunocompromised women are more likely to develop cervical cancer than immunocompetent women because they cannot clear the infection. 80% of sexually active women will have acquired genital HPV infection by age 50.
Low-risk HPV: HPV 6 and 11. More likely to cause genital warts
High-risk HPV: HPV 16, 18, 31, and 45
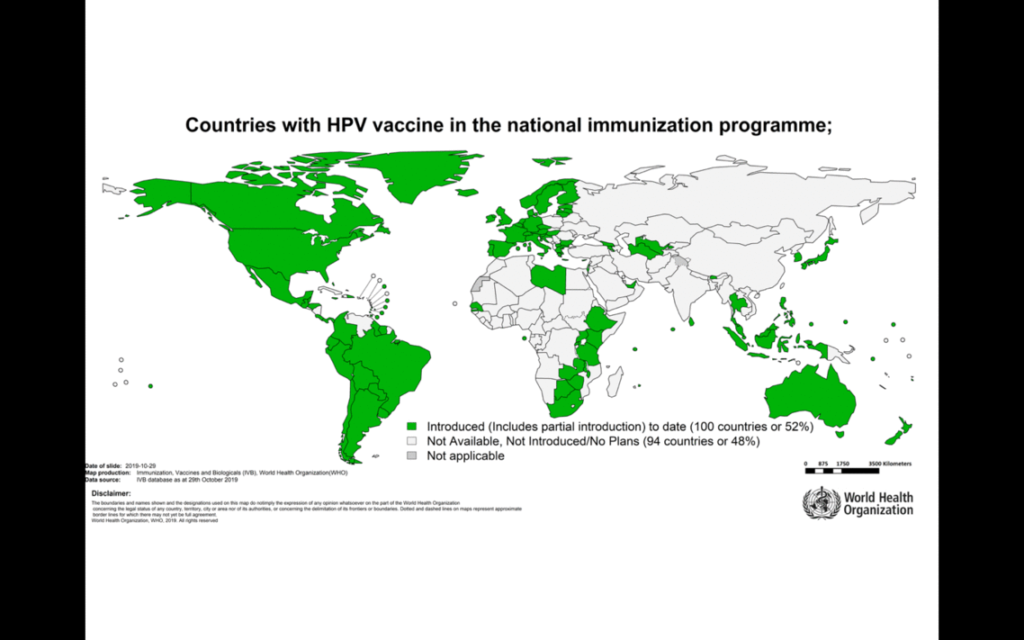
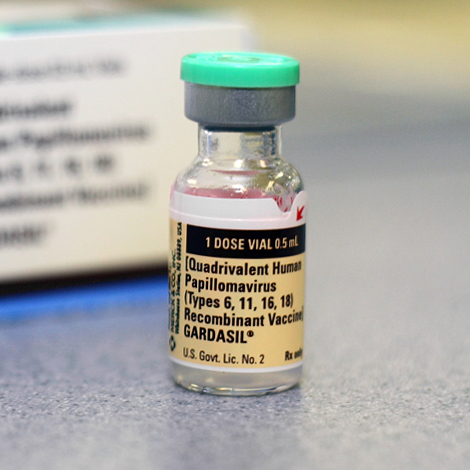
Vaccination (Gardasil)
“Guard against squamous intraepithelial lesions”
Gardasil is a vaccine containing recombinant Virus-like particles (VLP)s. It contains no HPV DNA and is therefore safe for immunocompromised and lactating patients. Exposing the patients to the particles causes an antibody response that quickly eliminates the virus when exposed to it.
Gardasil 4: HPV 6, 11, 16, and 18
Gardasil 9: HPV 6, 11, 16, 18, 31, 33, 45, 52, and 58
- Schedule
- Routine vaccination for girls and boys
- First dose: At 10- years (higher efficacy when given at younger years)
- Second (and third) dose: q6mos subsequently
- Routine vaccination for girls and boys
- Why is it important to immunise against HPV?
- HPV can be acquired at any point in life (including during monogamous relationships)
- The vaccine is not as effective if received later in life
- The vaccine may also be effective against Head and Neck Squamous Cell Carcinomas (HNSCCs)
Clinical Features
Cervical cancer is one of the more common gynaecologic cancers that present at a young age. CIN is more likely to present in younger women while invasive carcinoma is more prevalent in older women. Diagnosis is via biopsy (pap smears DO NOT diagnose cervical cancer)
- Risk factors
- Early intercourse (early exposure to HPV, more likely to have sex more in life)
- Early child-bearing (probably had intercourse earlier)
- “High-risk” partners (promiscuous partners, MSM)
- Low socio-economic status (lower quality of care and screening)
- History of STIs (can cause cervicitis)
- Cigarette smoking (independent)
- Immunosuppression (cannot clear HPV)
- Signs and symptoms
- Early disease is asymptomatic
- Post-coital bleeding
- Watery discharge
- Pelvic pain or pressure
- Rectal or urinary tract symptoms (depending on invasion or pressure effects)
- Physical exam
- Bimanual
- Cervical mass appreciated
- Invasive lesions in the upper vagina, cul-de-sac or adnexa
- Speculum exam
- Friable, bleeding cervical lesion (may invade other parts of the vagina)
- Bimanual
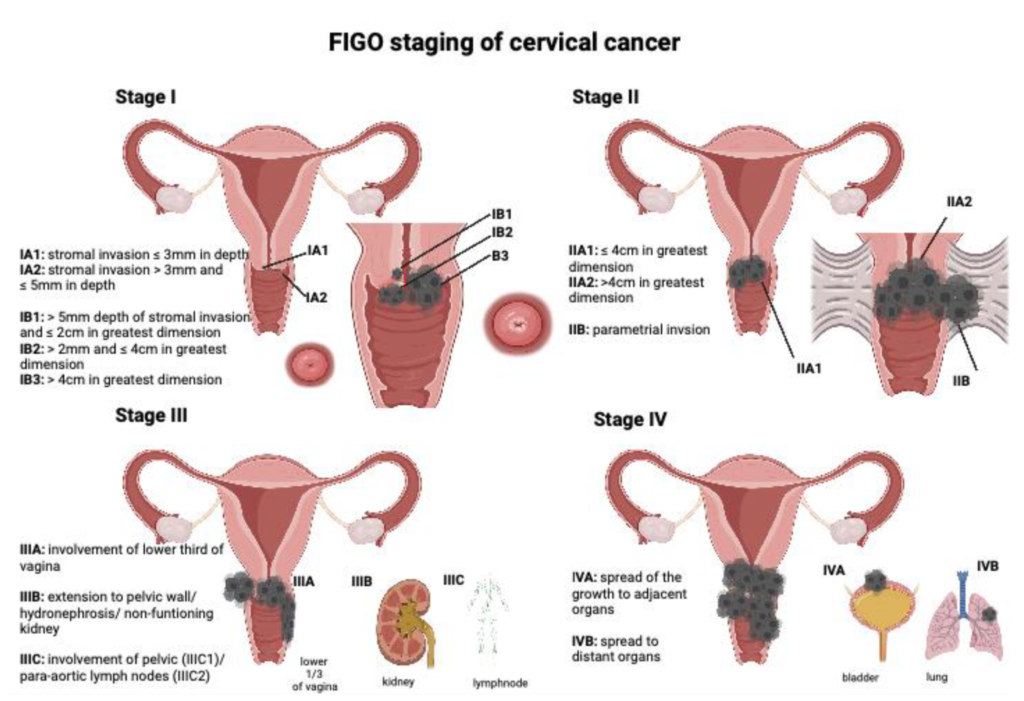
Staging cervical Cancer
Cervical cancer is the only gynecologic cancer that is stage clinically
- Investigations for screening cervical cancer MRI and CT are useful to determine the extent of disease (e.g. distant mets) but not for staging
- Examination under anaesthesia
- Cystoscopy
- Proctoscopy
- IV pyelography
- Barium enema
- CXR
| Stage | Description |
|---|---|
| 0 | Carcinoma in situ |
| I | Invasive carcinoma strictly confined to the cervix |
| IA | Microscopic lesion (IaI, Ia2 based on depth) |
| IB | Gross lesion (Ib1, Ib2 based on size etc.) |
| II | Extension beyond the cervix (upper 2/3 of the vagina) but not to the pelvic wall |
| IIA | No parametrial involvement |
| IIB | Parametrial involvement |
| III | Extension to the pelvic wall, lower 1/3 of vagina, or has caused hydronephrosis |
| IIIA | Extension to Lower 1/3 of vagina |
| IIIB | Pelvic sidewall involvement; hydronephrosis |
| IV | Extension beyond true pelvis or involving bladder or rectum |
| IVA | Extension to bladder or rectal mucosa |
| IVB | Extension outside true pelvis or distant mets |
Management of Cervical Cancer
- Treatment of stage 0 and IA1
- Cold Knife Conization
- Simple Hysterectomy
- Treatment of stage IA2 and IIA
- Radical hysterectomy
- Radiation
- Treatment of stage IIB to IV
- Chemoradiation
- Stage IIB – IVA: Cisplatin and 5-FU
- Stage IVB (metastatic) or recurrent: regimens with advanced chemotherapeutics, radiation if never received and pelvic exenteration
- Surgery added on top
- Chemoradiation
Cervical Cancer 5-year Survival
| Stage | 5-year survival |
|---|---|
| Stage I | 85-90% |
| Stage II | 65-70% |
| Stage III | 35-45% |
| Stage IV | 15-20% |



