Overview
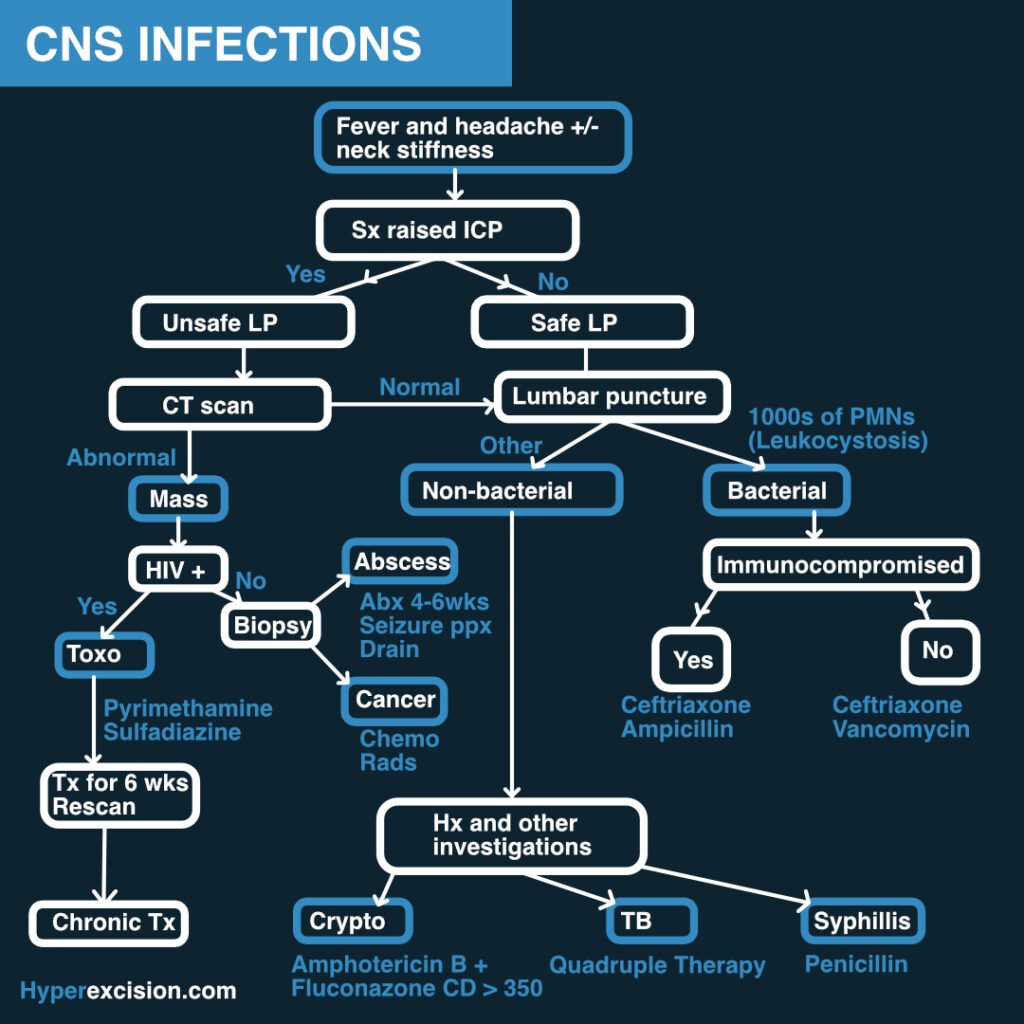
CNS infections carry a high mortality if untreated or improperly treated. It is important to recognize and treat differently neonates, young people, adults, old people, and immunocompromised since different organisms affect these different populations.
Infections of the CNS include:
| Infection | Description |
|---|---|
| Meningitis | Infection of the meninges |
| Encephalitis | Generalized infection of the brain parenchyma |
| Brain abscess | Focal infection and suppuration of the brain parenchyma |
- Symptom triad of CNS infections
- Fever
- Headache
- Altered mental status