Overview
Pulmonary edema where the heart is to blame. Increases in pulmonary pressure (PCWP) are secondary to ineffective filling/pumping of the heart. This is the most common presentation of Congestive Heart Failure (CHF).
The patient can go into respiratory fatigue.
- Etiology of cardiogenic pulmonary edema
- Congestive Heart Failure
- Valvular Disease (Aortic and Mitral)
- Arrhythmia
- Myocarditis
- Etiology of non-cardiogenic pulmonary edema
- Lymphatic obstruction (decreased drainage from the interstitium
- Excess volume administration
- Decreased oncotic pressure (low albumin state)
- Damage to the lung itself (inflammatory process etc.)
- Cause of early pulmonary edema
- Respiratory alkalosis (due to High respiratory rate)
- Cause of late pulmonary edema
- Respiratory acidosis (due to respiratory fatigue)
- Signs and symptoms
- Dyspnea
- Cough
- Pink frothy sputum
- Anxiety
- Chest Pain
- Tachypnea
- Tachycardia
- Visible distress
- Crackles
- Wheezing
- S3, S4 murmur
- Cool extremities
- Skin mottling
- Investigations
- Labs
- CBC
- U/E/Cs
- Liver Function Tests
- BNP
- Chest X-ray: acute or chronic (best initial step in a patient who does not need to be intubated)
- Echocardiogram
- EKG
- Labs
- Emergency treatment
- IV ACEi (Captopril)
- IV loop diuretic (Furosemide)
- IV nitroprusside or nitroglycerin
- 100% O2 (face mask, CPAP, BiPAP, intubation if necessary)
- Morphine
- Identify and address the underlying cause ASAP
- If systolic heart failure use Dobutamine
- Sit patient upright
- Reassurance
Typical presentations of Cardiogenic Pulmonary Edema
- The patient presents with worsening dyspnea on exertion, a history of high cholesterol, diabetes mellitus, smoking, CAD
- Systolic CHF (HFrEF)
- The patient presents with worsening fatigue, dyspnea, and has a history of untreated Strep infection, and had a longstanding murmur
- Mitral Valve Stenosis
- The patient presents with severe dyspnea and SOB and has a longstanding history of uncontrolled hypertension
- Diastolic CHF (HFpEF)
- The patient is being hospitalized and is a few days post MI, develops sudden dyspnea, pink frothy sputum, and new systolic murmur
- Papillary muscle rupture
- The patient is very tachycardic, presents with anxiety, chest pain, and SOB, and has an EKG that shows wide QRS complexes with no discernable P or T waves
- Ventricular Tachycardia
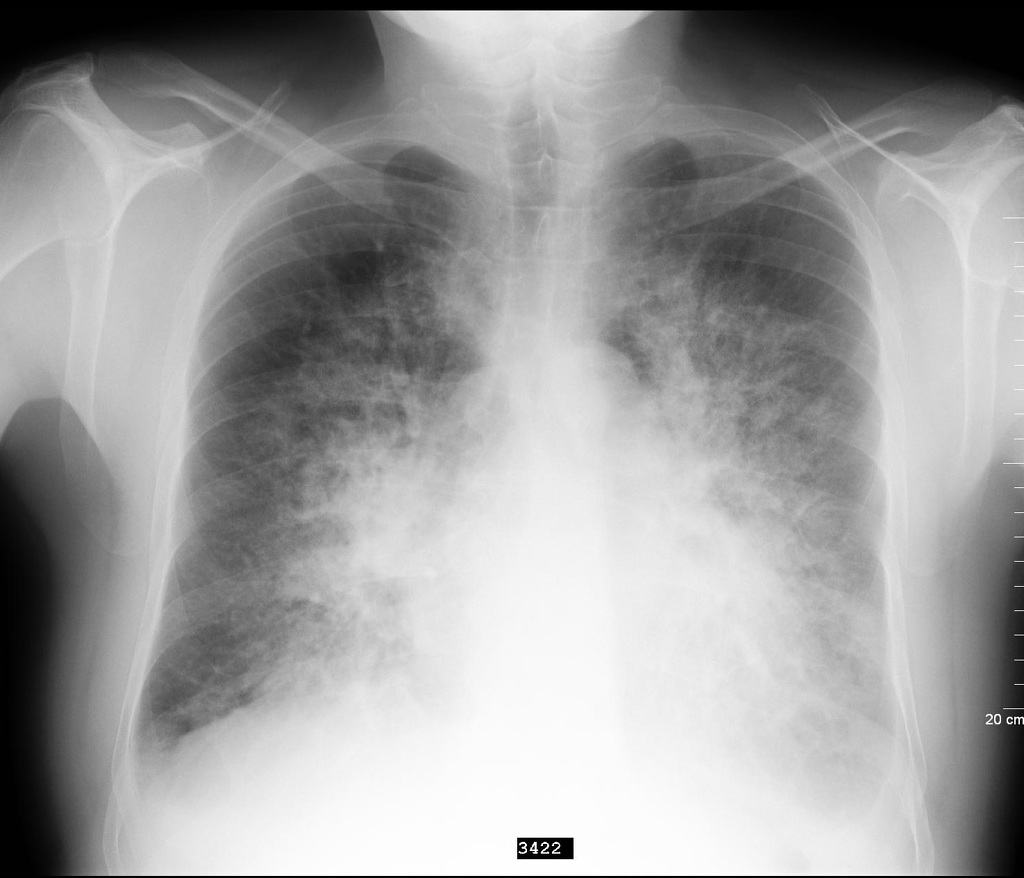
Chest X-ray in pulmonary Edema
Chest X-ray will clue you in on whether the edema is cardiogenic or non-cardiogenic. History, presentation, labs, and often echo and EKG are needed for definitive diagnosis
- Chest X-ray findings in acute pulmonary oedema
- Alveolar infiltrates: a must with every pulmonary edema (wheezing, hypoxia, etc.) – “Bat’s wings”
- Kerley B lines: fluid infiltration onto pulmonary interstitium (needs a keen eye)
- Edema prominent in lower lung fields: Dependent
- Hilar obscurity: frequent
- Blunted costophrenic angle:
- Enlarged cardiac silhouette: chronic condition (systolic CHF; Chronic Valvular Heart disease)
- Normal cardiac silhouette: diastolic CHF or acute condition (Valve rupture secondary to MI, Myocarditis, Arrhythmia, Volume overload)