Overview
An autopsy is the scientific examination of a dead person through dissection of the body for medical, legal, and/or scientific purposes. It is derived from the Greek word ‘autopsia’ meaning to see for oneself. The root Auto stands for ‘self’ while Psy stands for ‘view’
Definition of terms
| Term | Definition |
|---|---|
| Postmortem examination | Post-after, mortem- death. Any form of examination after death. A postmortem examination can be performed through an autopsy, or an external view and grant. |
| Autopsy | Dissection of the body in full or in a limited scope |
| View and grant | The body is examined thoroughly externally for any unusual signs to exclude foul play |
Types of autopsies
| Type | Description |
|---|---|
| Clinical (pathological) Autopsy | Performed to learn the extent of the disease that the deceased was being treated for. Permission of the family is required. |
| Medico-legal (Forensic) Autopsy | Done in the case of unexpected deaths to determine the cause, time and manner of death, and to identify the decedent. Permission of the family is not required and is performed under strict instructions of the legal authority. |
| Anatomical or academic autopsy | Performed by students of anatomy for study purposes only |
Purpose of an autopsy
- Purpose of an autopsy
- To make an identification of the body and to assess the size, physique and nourishment.
- To determine the cause of death or, in the newborn, whether live birth occurred.
- To determine the mode of dying and time of death, where necessary and possible.
- To demonstrate all external and internal abnormalities, malformations, and diseases.
- To detect, describe, and measure any external and internal injuries.
- To obtain samples for chemical, toxicological, or genetical analysis, microbiological and histological examination, and any other necessary investigations.
- To retain relevant organs and tissues as evidence.
- To obtain photographs and video for evidential and teaching use.
- To provide a full written report of the autopsy findings.
- To offer an expert interpretation of those findings.
- To restore the body to the best possible cosmetic condition before release to the relatives.
Role of autopsy in modern medicine
- Benefits to clinicians and healthcare organizations
- Clinicians can relate their physical and lab findings with the pathologic changes of the disease
- Autopsies are the gold standard for evaluating the accuracy of diagnosis and the outcome of therapy
- Hospital infection control committees can be alerted of a possible contagion
- Provides critical data for medical quality assurance and quality improvement
- May reduce hospital and physician malpractice risks- more careful due to the risk of litigation
- Autopsies are necessary to ensure the accuracy of death certificates
- Benefits to the family of the deceased
- Identification of hereditary or contagious disease
- Provide information for genetic counselling
- Help families with the grieving process and remove guilt
- Provides accurate data for the determination of insurance benefits or workers’ compensation
- Benefits to public health
- Surveillance through the detection of contagious diseases
- Identification of environmental hazards (bioterrorism)
- Provides accurate vital statistics (contributes to population health planning and disease prevention)
- Benefits to medical education
- Provides teaching material for anatomy, histology and pathology
- Benefits to medical discovery and applied clinical research
- Discover changing patterns of disease and new diseases
- Evaluate the toxic effects of drugs, the accuracy of imaging techniques, and the efficacy of new therapies
- Benefits to basic biomedical research
- Provides normal and diseased tissues for research
- Benefits to law enforcement and jurisprudence
- Medico-legal investigation of death is key in crime investigation
Objectives of a clinical autopsy
- Objectives of a clinical autopsy
- To establish the nature of the disease that has caused death
- To study the pathology of the disease that has caused death, even when the diagnosis had been established before death
- To ensure the standard of medical care- can give insight as to how to prevent similar deaths in the future
Clinical autopsies
Clinical autopsies should ideally be performed on all patients who die while in hospital to confirm diagnoses, check the effects of any of the treatments, identify inconsistencies, and audit the quality of the patient’s care. A preliminary report on the autopsy findings should be issued not less than 2 hours after the autopsy and a final comprehensive report should be done within 4 days. A supplementary report on the investigations, genetics, and toxicology should be timely dispatched. Clinical autopsies can be carried out only with the voluntary consent of a close relative or a senior next of kin of the decedent as opposed to a medico-legal autopsy to which the family cannot object. There may be significant religious and cultural limitations
Medico-legal autopsy
Medico-legal autopsies are mandatory, and a criminal procedure act requirement. They are carried out by a pathologist or medical officer as per the act. Done under the laws of the state
Definition of terms
| Term | Definition |
|---|---|
| Inquest | Inquiry or investigation into the cause of death where death is not apparently due to natural causes (i.e., disease) |
- When are inquests done?
- Sudden death e.g., ruptured aneurysms, myocardial infarctions
- Suicide, homicide, infanticide
- Death from accident, burns, or fall from height
- Death under anaesthesia or operation table or from postoperative shock
- Death due to medical negligence or within 24 hours of admission to a hospital
- Death of a convict in jail or police custody
Autopsy
- Autopsy procedure
- The autopsy must be standard to avoid missing out on details. The absence of information may be used to discredit one’s evidence.
- A23 form
- Identification- physical, dental records, X-rays, DNA
- Understand the circumstances surrounding the death- history (maybe clinical), scene, photographs
- Examine the clothing-in-situ, especially for gunshot and stab wounds. Examine for tears and loss of buttons. They should be stored in brown bags (envelopes). In plastic bags, changes may occur due to moisture.
- Photography- according to the Evidence Act, the attorney general appoints the scenes of crime photographers. As an expert, photographic evidence is admissible in court.
- Guide the collection of trace evidence concurrently during the procedure
- Perform a detailed external examination with documentation. Indicate the site, describe and measure any wounds in relation to the fixed anatomical landmarks
- Sampling: blood, stomach contents, liver urine, vitreous humour, kidney, e.t.c
- The autopsy must be standard to avoid missing out on details. The absence of information may be used to discredit one’s evidence.
- Requirements for performing an autopsy
- Natural lighting
- Dissection kit
- Running tap water and dissection tables
- Containers for collecting samples for toxicology, microbiology, virology
- Who may be present at an autopsy?
- Pathologists, medical officers
- Investigating officer for medico-legal autopsies
- For examination of the scene of death, it is important for the pathologist to assess the environment, the local circumstances, and the position and condition of the body. Locard’s principle holds that the perpetrator of a crime will bring something into the crime scene and leave with something from it, and that both can be used as forensic evidence
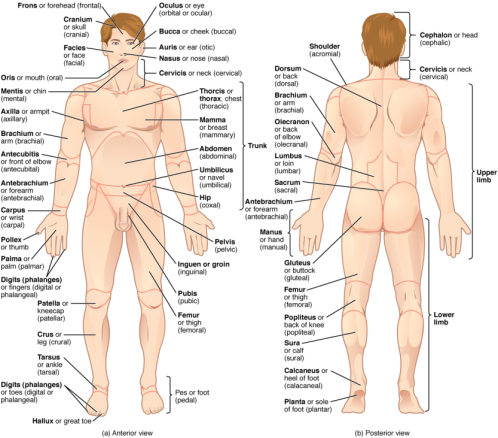
External Examination
Anatomical landmarks are used to describe locations of any important findings observed on the body during the external examination
- Clothing
- Describe in great detail. Look for tears, holes, loss of buttons
- External appearance (Head-to-toe examination)
- Gender
- Race
- Build
- Age (pediatric, adult or geriatric)
- General skin color (hypostasis, congestion, cyanosis, cherry-pink- carboxyhemoglobin), scars
- General nutritional status (malnourished, lean, obese, dehydrated, oedematous)
- State of cleanliness and hygiene (finger and toenail states, urinary or faecal soiling)
- Acquired external marks (tattoos, piercings, amputations, surgical scars, burns)
- Eyes (petechial haemorrhages)
- Mouth/ nostrils (vomitus, froth, blood, foreign body, damaged teeth, drugs, injured gums and lips, bitten tongue of epilepsy, jaw fractures)
- An inspection of body orifices
- Blood/ CSF leakage
- Vaginal or rectal discharge
- Injuries (shape, margins, length and breadth of the injuries, and their orientation on the body axis)
- Hands (defence wounds, bruised knuckles)
- Postmortem changes e.g. the presence of rigor mortis
- Breast palpation findings in female
- Congenital anomalies (spina bifida, ectopic cordis)
- Measurements:
- Height
- Weight
Internal examination
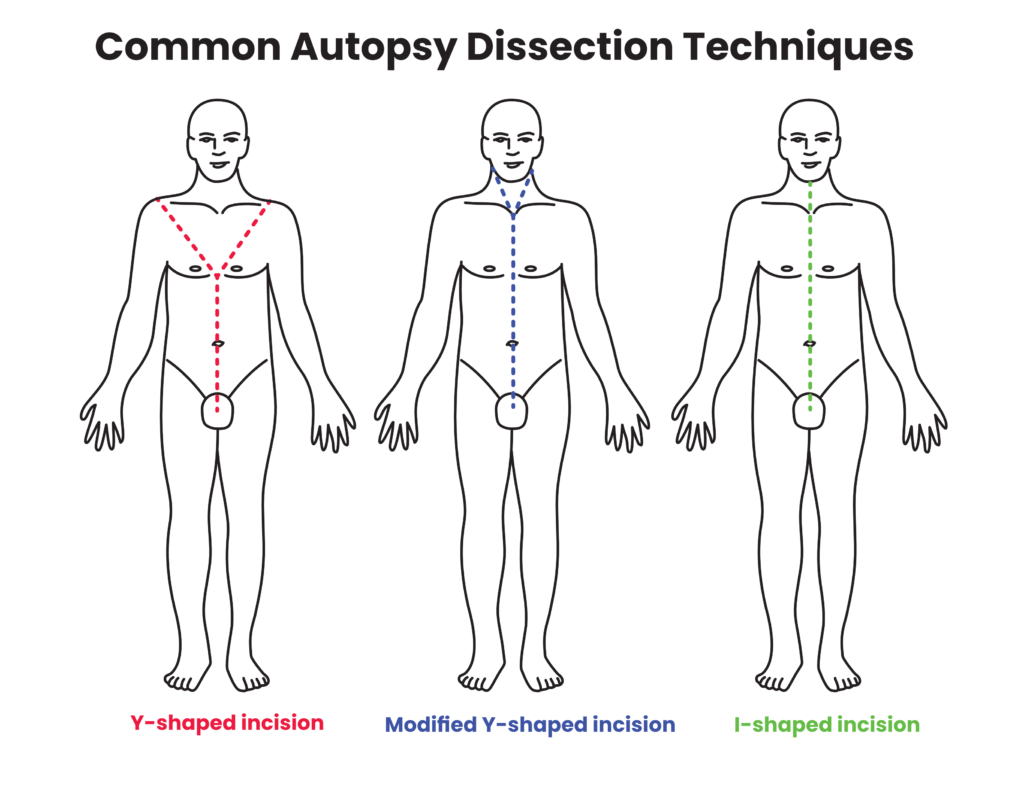
Primary incisions
Primary incisions are made on the skin. Secondary incisions are made on bones, tertiary incisions on serous membranes, and quartenary incisions on viscera.
| Incision | Description |
|---|---|
| I-shaped incision (vertical, midline) | From the chin to pubic symphysis. Commonly done for clinical autopsies, where neck dissection is not necessary |
| Y-shaped incision | From shoulder tips obliquely to xiphisternum, down to pubic symphysis avoiding umbilicus |
| Modified Y incision | From mastoid, down the lateral side of the neck, to suprasternal notch down to pubic symphysis; good for neck dissection and in asphyxial deaths |
| T-shaped or transverse | From one acromion process to the other with a vertical incision from the suprasternal notch to the pubic symphysis |
| X-shaped | On the back of the body, skin is reflected in an X shape to look for deep contusion; seen in custodial deaths |
| Coronal incision/mastoid-mastoid incision | The scalp is incised in the coronal plane, beginning at the mastoid process, behind the ear, running across the vertex, to reach the opposite mastoid |
| Minimally Invasive Tissue Sample (MITS) | Done for suspected high-risk infectious disease cases |
Methods of dissection of internal organs (evisceration)
| Technique | Description |
|---|---|
| Virchow (Individual organs) | Individual organ removal followed by dissection. Preferred if pathology is limited to one organ (rare) |
| Rokitansky (In Situ) | Organ dissection in-situ. Method of choice in post-mortem of highly transmissible disease |
| Letulle (en mass) | En-masse dissection and organ separation. Allows assessment of the relationship between organs |
| Ghon (en block) | Separate block dissection and organ separation. May lead to distortion of findings in cases of unexpected pathology |
Removal of the brain
- Removal of the brain
- Scalp incision: behind the mastoid across to the opposite mastoid (coronally)
- Examine the galea for haemorrhages, haematomas
- Retract the scalp to reveal the calvarium. Remove the dura and examine extensively for fractures. Use an oscillator saw to cut the cap of the skull
- Deliver the brain.
- Brain is suspended in 40% formalin to fix it (for 14 days)
- Scalp incision: behind the mastoid across to the opposite mastoid (coronally)
Ancillary investigations
- Ancillary investigations
- Microbiology: blood, tissues
- Toxicology: blood, urine, stomach with its contents, organs (liver, kidney), intestinal contents, CSF, bile, ocular fluid
- Histology
- Autopsy radiology and post-mortem imaging: suspected child abuse, gunshot wounds, identification and dentistry
- Forensic photography
The autopsy report
- Components of the autopsy report
- Full personal details of the deceased subject, unless unidentified- includes name, gender and age
- Place, date and time of the autopsy
- Name and qualifications of the pathologist
- Persons present for the examination
- The authority commissioning the autopsy
- A record of who identified the body- their names and I.D.s
- The name and address of the deceased subject’s regular (or last) medical attendant
- The date and time of death, where known
- The history and circumstances of the death
- External examination
- Internal examination
- List of specimens collected and the purpose for collection e.g., toxicology, histology
- The results of further examinations such as histology, microbiology, toxicology and clinical and/ or forensic genetics
- Discussion of the findings, if necessary, in the light of the known history
- An opinion as to the definite or most likely sequence of events leading to the death
- A formal cause of death, in the format recommended by the WHO (ICD 10 or 11) suitable for the completion of a death certificate
- The signature of the pathologist
Cause of death
Cause of death is defined as any injury or disease-producing physiological derangement briefly or over a long period, and which results in the death of the individual. It refers to the anatomical or pathological change directly leading to death. It is what you can visualise during the autopsy
- Examples of causes of death
- Hemopericardium due to sharp force trauma secondary to a stab wound to the chest
- Head injury due to blunt force trauma secondary to a road traffic accident
Mechanism of death
Mechanism of death is the physiological derangement produced by the cause of death that results in death. A particular mechanism of death can be produced by multiple causes of death and vice versa
- Examples of mechanisms of death
- Haemorrhage
- Septicaemia
- Ventricular fibrillation
- Respiratory paralysis
Manner of death
Manner of death explains how the cause of death came about. Manner of death is categorised as either natural or unnatural.
Manner of death
| Category | Description |
|---|---|
| Natural | Death due to disease |
| Unnatural | Homicide, suicide, accident, undetermined |
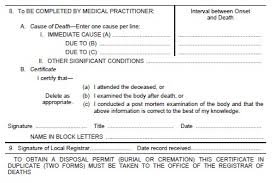
Death certification using ICD 10
ICD 10 is the international classification of diseases. WHO 20 assembly described the cause of death as all those diseases, morbid conditions, or injuries which either resulted in or contributed to death and the circumstances of the accident or violence which produced any such injuries
It ensures that all relevant information is recorded and that the certifier does not select some conditions for entry and reject others
This does not include symptoms or modes of dying e.g., heart failure or kidney failure or headache
- Important aspects of the death certificate:
- Should be clear
- No abbreviations
- Cause of death well indicated under part 1
- Underlying disease process or processes that lead to the death is under part 2
- This is the disease or injury which initiated the train of morbid events leading directly to death
- The circumstances of the accident or violence that produced the fatal injury
- More examples of causes of death:
- Death due to massive haemorrhage due to sharp force trauma due to a stab wound of the heart, with the manner being a homicide
- Death due to head injury due to blunt force trauma secondary to road traffic accident
- Death due to pulmonary thromboembolism, due to deep venous thrombosis due to immobilisation as a consequence of fracture of the right femur
- Upper GI haemorrhage due to oesophageal varices as a consequence of macronodular cirrhosis of the liver due to a Hepatitis B infection
Negative autopsy
A negative autopsy is when gross and microscopy examination fail to reveal the cause of death. 5- 10 % of deaths remained unascertained after autopsy
Legal considerations for an autopsy
- Consent
- Clinical Autopsy requires consent from the next of kin.
- Consent is generally not needed for a medico-legal autopsy.
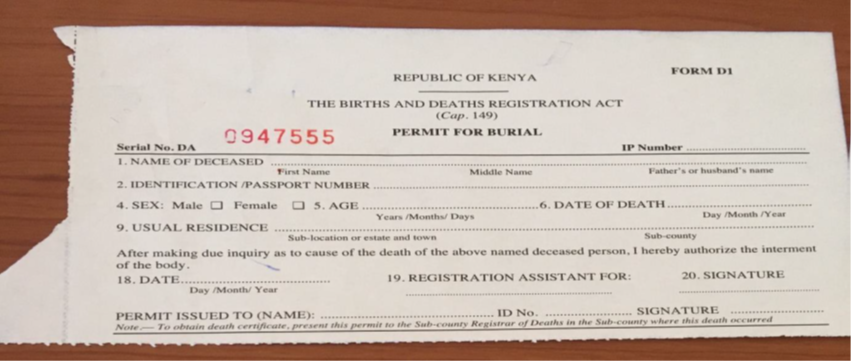
- Request is made by police, authorised by the law in Inquests Act (by a magistrate). The report is documented in a police document e.g. Form A 23.



