Overview
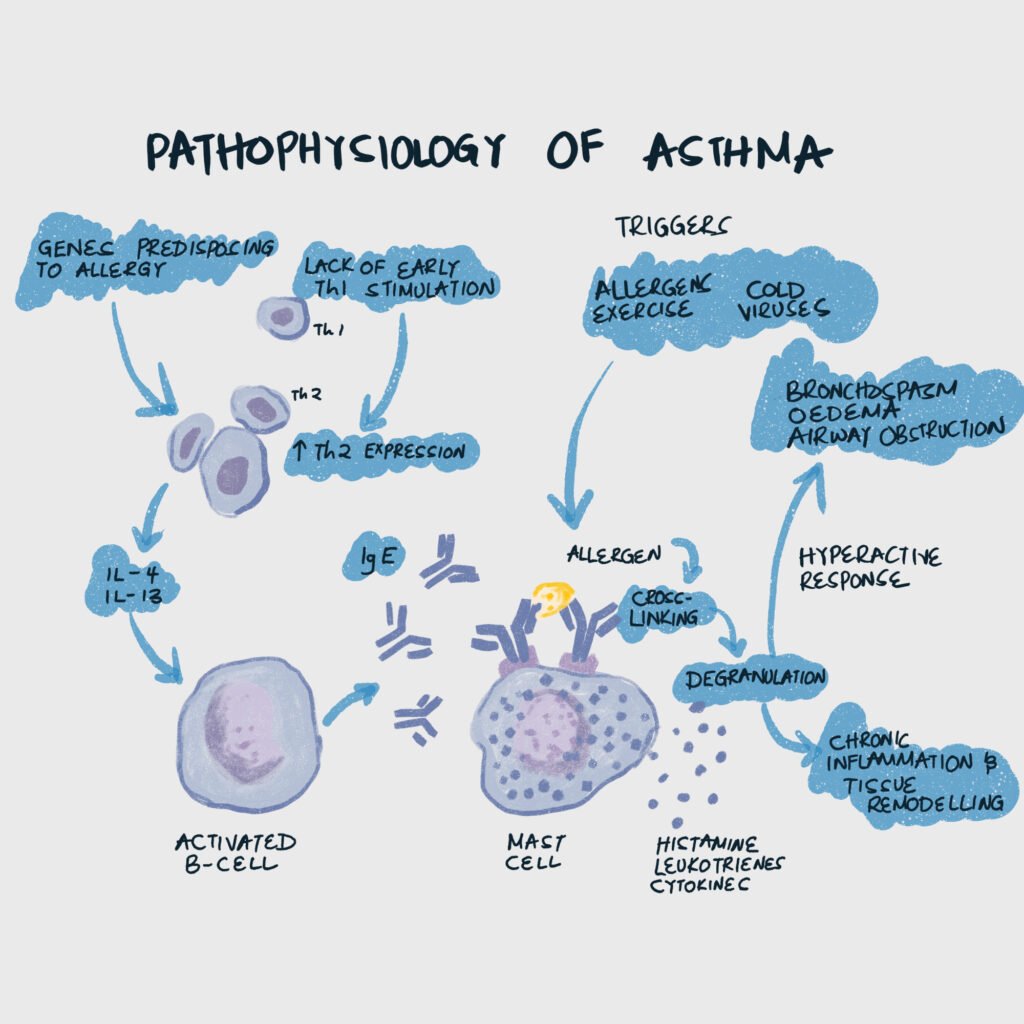
Asthma is an acute or sub-acute inflammation of the airways, precipitated by a variety of factors that result in bronchial hyperactivity and airway obstruction. The cause is idiopathic. Varies in degrees of severity and chronicity. Mild attacks may linger for weeks with only slight impairment. Severe attacks are a medical emergency. Treatment focuses on reducing overall airway inflammation and aborting acute attacks (with a rescue inhaler). Asthma is more problematic in children than in adults (narrower airway)
Preponderance in children. Boys are affected more frequently than girls. Women are affected more frequently than men. Blacks are affected more than whites. Asthma is more prevalent in urban regions.
- Triggers
- Environmental allergens
- Exercise
- Infection (Rhinovirus, Pneumonia, Sinusitis)
- GERD
- Aspirin
- Cardinal symptoms
- Shortness of breath
- Wheezing
- Tachycardia
- History of allergy
- Severe symptoms
- Accessory muscle use
- Decreased breath sounds
- Diaphoresis
Determining the severity of asthma
| Intermittent | Mild | Moderate | Severe | |
|---|---|---|---|---|
| Daytime Symptoms | ≤ 2 days/week | > 2days/week but not everyday | Daily | Throughout the day |
| Awakenings | ≤ 2x/month | 3-4x/month | >1x/week but not qPM | qPM |
| SABA use | ≤ 2days/week | >2days/week but not daily | Daily | Several times a day |
| Daily interference | None | Minor | Some | Extreme |
| Lung function (FEV1/FVC) | Normal between exacerbations | Normal between exacerbations | 0-5%, <nl between exacerbations | >5%, <nl between exacerbations |
| Exacerbations requiring systemic corticosteroids | 0-1/yr | ≥ 2/yr | ≥ 2/yr | ≥ 2/yr |
| Recommended treatment step | Step 1 | Step 2 | Step 3; consider PO steroids | Step 4 or 5; consider PO steroids |
Asthma meds
Short-acting Beta 2 agonist (SABA): Albuterol. Rescue inhaler for recurrent episodes.
Long-acting Beta 2 agonists (LABA): Formoterol, Salmeterol. For control.
Inhaled corticosteroids (ICS): Fluticasone, Budesonide Triamcinolone, Mometasone
Mast-cell stabilizers: Cromolyn
Leukotriene receptor antagonists (LTRAs): Montelukast, Zafirlukast
Theophylline
Zileuton
Omalizumab
Step-up approach for Asthma Treatment
All patients get SABA. LABA may be substituted by a LTRA (montelukast, zafrilukast), theophylline, or zileuton. Most pts w/asthma are in Step 2, or Step 3 therapy (once in a while step 4). Pts who have asthma w/known triggers are in step 1 therapy. Consider adding Omalizumab in steps 5 and 6.
| SABA | ICS | LABA | Systemic Corticosteroid | |
|---|---|---|---|---|
| Examples | Albuterol | Fluticasone, Mometasone | Salmeterol, fomoterol | Prednisone (PO), Methylprednisolone (IV) |
| Step 6 | Yes (PRN) | High dose | Yes | Yes |
| Step 5 | Yes (PRN) | High-dose | Yes | No |
| Step 4 | Yes (PRN) | Medium dose | Yes | No |
| Step 3 | Yes (PRN) | Low-dose or medium-dose | Yes | No |
| Step 2 | Yes (PRN) | Low-dose | No | No |
| Step 1 | Yes (PRN) | No | No | No |
- When to step up
- Persistent symptom (make sure to check adherence)
- Use of SABA > 2 days/week for symptom relief
- Comorbidities
- When to step down
- If possible
- Symptoms controlled for ≥ 3 months
- What to do if a patient has symptoms more than twice a week
- Add inhaled corticosteroids
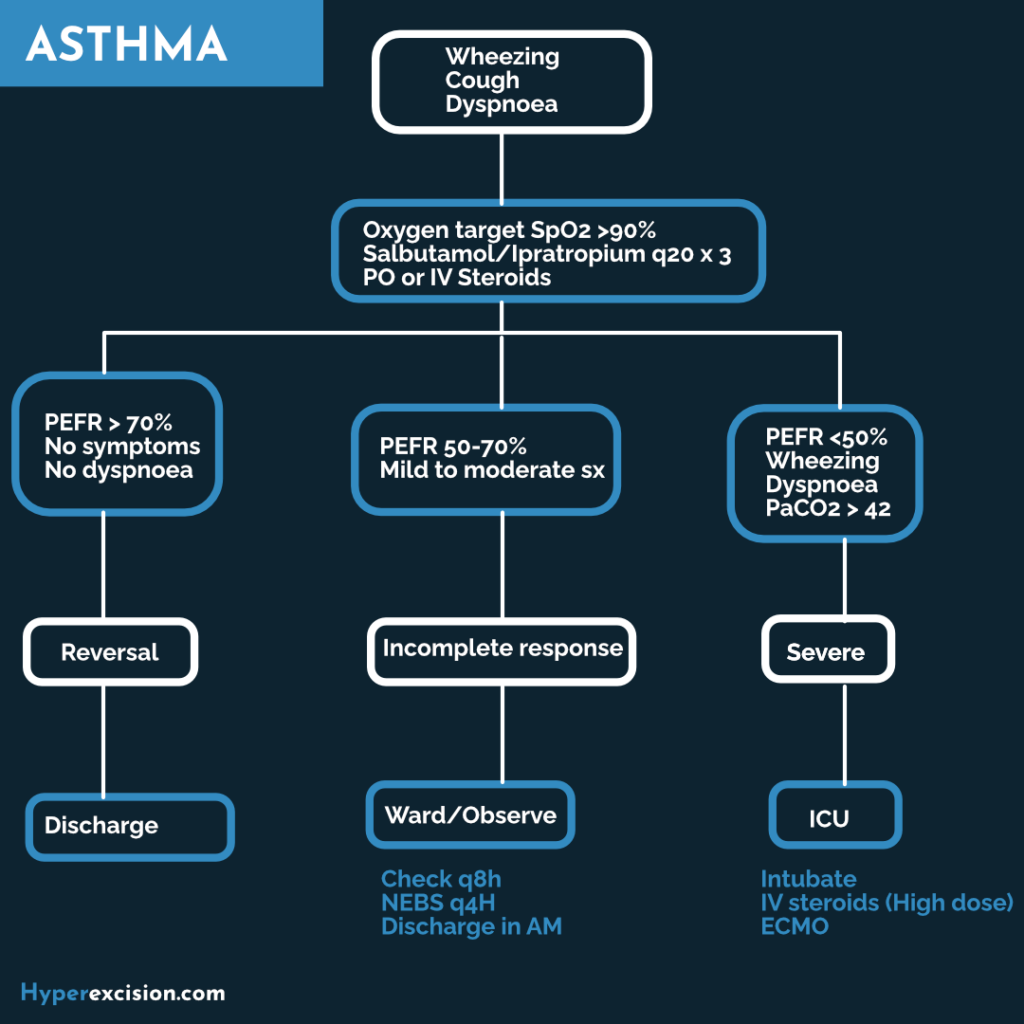
Acute Asthma Attack
Any patient with an asthmatic attack resistant to a beta-agonist inhaler or nebulizer should be admitted for overnight observation. Status asthmaticus is a moderate or severe asthma attack not responding to conventional therapy or persisting for more than 12 hours.
- Symptoms of an asthma attack
- Dyspnea
- Shortness of breath
- Wheezing
- Prolonged expiration
- Use of accessory muscles
- Intercostal retractions
- Perspiration
- Reduced breath sounds
- Fatigue
- Symptoms of a mild attack
- Wheeze
- Pulse rate < 100bpm
- Respiratory rate < 20/min
- Blood pressure is normal
- Symptoms of a moderate attack
- Wheeze + cough
- Sweating
- Pulse rate 100-120bpm
- Respiratory rate 20-30/min
- Blood pressure is normal
- Symptoms of a severe attack
- Cyanosis
- Pulse rate >120bpm
- Respiratory rate >30/min
- Pulsus paradoxicus
- Respiratory distress (use of accessory muscles, intercostal retractions)
- Chest silent to auscultation
- Differentials
- Foreign body: unilateral wheezing, stridor, mucus, visible foreign body, and the history is suggestive
- Anaphylaxis: swelling/flushing of the face, rhinorrhea, stridor, hypotension, history (bug stings, recent medications, etc.)
- Investigations
- Chest X-ray PA, Erect
- Peak expiratory flow rate (PEFR): decreased
- Forced expiratory volume in the first second (FEV1): decreased
- Maximal mid-expiratory flow rate (MMEFR): decreased
- Other routine labs
- ABGs: initially respiratory alkalosis, shifting to acidosis
- General treatment
- Admit for overnight observation
- Supplemental O2 (NC or mask, mandatory)
- Maintain SpO2 > 90%
- Nebulized Albuterol (Salbutamol)
- IV beta agonist (terbutaline)
- Anticholinergic (Ipratropium, Tiotropium) if patient is having a minor attack and is relatively stable (takes longer to act)
- Treatment of a mild attack
- SC adrenaline 1:1000 0.5ml STAT, repeat after 20-30 minutes for a total of 3 doses if no response
- Nebulized Albuterol (Salbutamol)
- Discharge on Salbutamol 4mg TDS for 1 week or Theophylline 200-250mg BD or TDS
- Treatment of a moderate asthma attack
- SC adrenaline 1:1000 0.5ml STAT, repeat after 20-30 minutes for a total of 3 doses
- Nebulized salbutamol and ipratropium bromide q20mintes until response (or if a patient develops tremors)
- IV aminophylline 6mg/kg slowly over 15 min if no response, then 0.9mg/kg/hour
- Treatment of a severe asthma attack
- Oxygen 3-5 L/min; Endotracheal intubation may be indicated
- IV Aminophylline 0.9mg/kg/hour in NS drip after loading dose if not already given
- IV Hydrocortisone 200mg STAT or Methylprednisolone 1g IV STAT or Dexamethasone 2-4mg IV/IM STAT
- Oral Prednisone 10-15mg TDS on admission. Taper off in 7-10 days.
- Give ICS or LABA or LTRA or Theophylline
- Give amoxicillin or cotrimoxazole or tetracycline