Overview
Generally, antipsychotics are dopamine antagonists (D2 receptors). Remember the primary theory behind psychotic disorders is dopamine overproduction/hyperactivity. Antagonizing dopamine is a useful way to block psychotic symptoms.
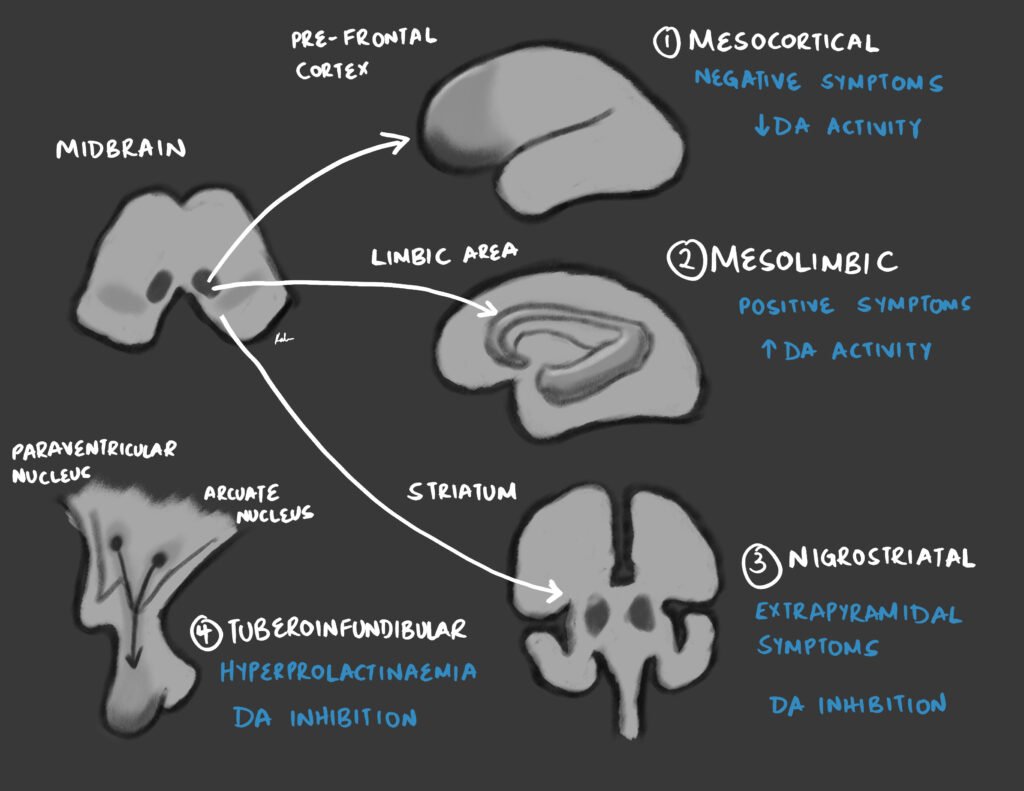
| Dopaminergic pathway | Function |
|---|---|
| Nigrostriatal | Motor Control (Responsible for extrapyramidal side effects) |
| Mesolimbic | Emotional expression (Dopamine excess responsible for positive symptoms) |
| Mesocortical | Cognitive processes (Dopamine hypo activity responsible for negative symptoms, Role of 5-HT) |
| Tuberoinfundibular | Dopamine is prolactin inhibiting factor (Blockage causes Hyperprolactinemia – Galactorrhea, Amenorrhea, Decreased libido) |
- Effects of dopamine excess
- Psychosis
- Aggression
- Hypervigilance
- Effects of dopamine deficiency
- Depression (Anhedonia)
- Hypersomnia
- Parkinsonism
- Prone to addiction (Caffeine and stimulants)
- Prone to gaining weight
First Generation (Typical) Antipsychotics
Typical antipsychotics are antagonists of D2 only (Haloperidol, Chlorpromazine). They are mostly used for acute management of psychotic symptoms. They do not relieve negative symptoms. They also have more extrapyramidal side effects (EPSEs). High-potency typical antipsychotics have a greater potential for extrapyramidal side effects.
High potency FGAs are more likely to cause EPS symptoms. Low potency FGAs are more likely to cause anticholinergic side effects. Low potency FGAs are also more likely to lower the seizure threshold.
Have a latency of 4-6 weeks until full response. 70-80% of patients respond. 30-40% show partial relapse. 0% relapse within 2 years. Non-compliance is common
Typical Antipsychotics
| Potency | Examples |
|---|---|
| High-potency | Haloperidol (Haldol), fluphenazine (Prolixin), trifluoperazine, pimozide, droperidol (Inapsine) |
| Medium-high potency | Flupenthixol, zuclopenthixol, loxapine (Loxitane), thiothixene (Navane), molindone (Moban), perphenazine (Trilafon) |
| Low potency | Chlorpromazine (Thorazine, Largactil, 1950), thioridazine (Mellaril) |
Selected first generation antipsychotics
| First generation antipsychotic | Nota bene |
|---|---|
| Chlorpromazine | Invented in 1950. Onset of action via oral route is 30-60 minutes while deep intramuscular is 2-3 minutes. It accumulates in fatty tissues and has a half-life of 24 hours or more. Watch out for postural hypotension (do not give IV). A leathal side effect is QT prolongation (an potential for heart block and tachycardia). Other side effects include blue-grey discoloration and photosensitivity. Can also be used to treat intractable hiccups and vomiting. Preferred for rapid tranquilization* |
| Haloperidol | Commonly used. A decanoate (long-acting injectible – LAI) form exists |
| Fluphenazine | Commonly used. A decanoate (LAI) form exists |
Second Generation (Atypical) Antipsychotics
Atypical antipsychotics are antagonists of D2, D4, and 5-HT2. They are commonly used for maintenance therapy. More effective against resistant schizophrenia and negative symptoms. Have less Extrapyramidal Side Effects. Major side effects include hyperprolactinemia, weight gain and diabetes.
Aripiprazole (Abilify), clozapine (Clozaril; rarely causes EPSE), olanzapine (Zyprexa), quetiapine (Seroquel), ziprasidone (Geodon), lurasidone, risperidone (Risperdal)
Selected second generation antipsychotics
| Second generation antipsychotic | Nota bene |
|---|---|
| Risperidone | Highly effective against positive and negative symptoms. Higher rates of EPSE (dose-related). LAI form exists (Consta). Side effects in include hyperprolactinemia, weight gain, sedation, orthostatic hypotension and reflex tachycardia. |
| Paliperidone | A modified risperidone. LAI exists. 59% excreted unchanged in urine. Has no relevant clinical interacitons |
| Clozapine | The first atypical antipsychotic. Indicated for treatment resistant schizophrenia. Less likely to cause Tardive dyskinesia. The only antipsychotic shown to decrease the risk of suicide. Has a 4% risk of seizures. A serious side effects is agranulocystosis (stop if ANC < 1500/ul). |
| Olanzapine | A severe side effect is ventricular arrhythmia. Associated with weight gain and sedation. |
| Quetiapine | Causes little weight gain. Less likely to cause extrapyramidal side effects and hyperprolactinemia. Has sedative effects and orthostatic hypotension. |
| Aripiprazole | Theoretically useful against negative symptoms (due to partial D2 agonism). Can be more activating (akathisia) ****and less sedating. Less potential for weight gain. LAI form exists. |
| Ziprasidone | Less likely to cause weight gain |
- What are the side effects of clozapine?
- Agranulocytosis/Leukopenia (require weekly CBCs): stopped if absolute neutrophil count drops below 1500/ microliter – Before prescribing, every week for 6 months, Bi weekly for another 6 months then monthly (every 6 weeks)
- Lowers seizure threshold (especially with olanzapine and chlorpromazine)
- Small risk of myocarditis
- Hyperglycemia
- Hyperlipidemia
- Seizures
- Neuroleptic malignant syndrome
- Hypersalivation
- QT prolongation and Ventricular arrhythmia
- What are the adverse effects of clozapine?
- Anticholinergic (Contraindicated in the elderly) eg dry mouth
- Weight gain and metabolic syndrome
- Increased salivation
- Sweating
- Dizziness
- Headache
- Tachycardia
- Nausea
- What are the indications for using clozapine?
- Resistant schizophrenia
- Mania
- Severe Psychotic depression
- PDD/Autistic
- Suicidal Psychotic
- OCD (adjunct)
- Why is clozapine not used as first-line in treating psychotic disorders?
- Causes agranulocytosis
- Which atypical antipsychotic is good for patients with depressive symptoms?
- Aripiprazole
- Why is risperidone preferred for use in elderly patients?
- Less sedation (only blocks D2 and 5-HT, does not block D4; Sedated elderly patients are more likely to fall down and most of them are osteoporotic)
- Mnemonic: “Rise and shine (wake up), with Risperidone
- A person presents to you after having an acute psychotic episode. He is obese and has poorly controlled diabetes. What antipsychotics are good options for starting treatment?The
- SGAs aripiprazole (Abilify), ziprasidone (Geodon), and Lurasidone (Latuda) have minimal weight gain and metabolic side effects. Though other side effects must be weighed accordingly.
Prescribing antipsychotics
- When to prescribe antipsychotics?
- **Psychotic disorders (**atypical antipsychotics for long-term management)
- Acute agitation (haloperidol, ziprasidone)
- Major Depressive Disorder with psychotic features
- Bipolar II Disorder- in treatment of mania, hypomania and depression
- Movement disorders involving the basal ganglia dopaminergic syndrome (Huntington’s Disease, Tourette’s syndrome)
- Psychosis associated with delirium, dementia, or other organic disorders
- Psychosis caused by other drugs and psychoactive substance abuse
- Delusional disorders
- How to prescribe antipsychotics
- Select the drug based on side-effect profile, patient preference, medical history, previous history, cost, and availability
- Start at the lowest dose possible first (”start low, go slow). Especially for antipsychotic naive patients. Long-acting injectables are not recommended during the acute phase of the first episode of an antipsychotic naive patient.
- Review the mental state regularly. Can use the PANSS or BPRS to monitor for improvement.
- Monitor for side-effects.
- Avoid antipsychotic ‘poly-pharmacy) using more than one
- Prescribe an adequate fose for at least 4 to 6 weeks
- Effect manifests within 2 – 3 weeks and a further 2 -3 weeks for it to maximise )(a total period of 4 – 6 weeks). If the patient recovers continue the medication for several months after recovery. If there is no improvement change to another antipsychotic.
- Contine treatment for at least 1 year following remissio
- If there is repreated relapses whenever medication is discontinued, consider long-term (possibly life-long) maintenance
- If non-complaince is a major factor in relapse, consider a long-acting injectable
General monitoring (especially with second-generation antipsychotics) – note that this is an oversimplification
| Investigation | Frequency |
|---|---|
| Complete blood count | At the start of therapy, annually (clozapine requires more frequent monitoring) |
| Urea and electrolytes | At the start of therapy, annually |
| Liver function tests | At the start of therapy, annually |
| Lipids and weight | At the start of therapy, at 3 months, annually |
| Fasting blood glucose | At the start of therapy, at 6 months, annually |
| Prolactin | At the start of therapy, at 6 months, annuallu |
| Blood pressure | Baseline, frequently during dose titration |
| Electrocardiogram | Baseline |
| Cardiovascular risk assessment | Annually |
Long-term Maintenance treatment
This is given to control symptoms, reduce the risk of relapse and improve the quality of life
| Episode | Duration of maintenance after remission |
|---|---|
| 1st episode | 1 year |
| 2nd episode | 2 years |
| 3rd episode | 5 years |
| Others | Life-long maintenance |
Tranquilization
Tranquilization is indicated for agitated/aggressive patients when verbal or other methods of de-escalation fails.
Haloperidol is the drug of choice for rapid tranquilization in agitation due to psychiatric illness and alcohol intoxication. This is due to its relative lack of autonomic side effects.
- Oral options for tranquilization
- Lorazepam 1-2 mg PO repeated after 45-60 minutes if needed
- Promethazine 25-50 mg PO repeated after 45-60 minutes if needed
- Lorazepam 1-2 mg PO and Haloperidol 5-10 mg PO repeated after 45-60 minutes if needed
- Oral risperidone 2 mg and Lorazepam 2 mg
- Oral olanzapine 10 mg and Lorazepam 2 mg
- Maximum oral doses in 24 hours:
- Lorazepam: 4 mg
- Haloperidol: 30 mg
- Promethazine: 100 mg
- Olanzapine: 20 mg
- Risperidone: 4 mg
- Intramuscular options for rapid tranquilization
- Chlorpromazine (Largactil) IM 25-100 mg
- Haloperidol (Haldol) IM 10-20 mg
- Lorazepam IM 1-2 mg
- Zuclopenthixol (Clopixol, Acuphase; 2-3 hours, lasts 48 hours) IM 50-150 mg, repeat every 2-3 days if necessary with maximum dose of 400mg
- Olanzapine (Zyprexa, 30 min lasts 6 – 7 hours) IM
- Diazepam 10 mg by slow IV bolus
- What is the contraindication for rapid tranquilization with benzodiazepines
- Possible head injury
Adverse effects of antipsychotics
- What is a common side effect of atypical antipsychotics?
- Weight gain
- Adverse effects secondary to dopamine blockade
- Nigrostriatal: Extrapyramidal symptoms -Acute dystonia TD, NMS, Akathisia (Movement of the basal ganglia, degenerates in Parkinson’s syndrome hence causes Parkinson-like syndromes)
- Tuberoinfundibular: Galactorrhea, Gynecomastia, Amenorrhea (disinhibition of prolactin. Dopamine is prolactin inhibiting factors)
- Adverse effects secondary to antihistaminic properties
- Sedation
- Weight gain
- Adverse effects secondary to alpha 1 adrenergic blockade
- Orthostatic Hypotension with reflex tachycardia (the patient just falls or staggers)
- Sedation
- Adverse effects secondary to anticholinergic properties
- Constipation
- Urinary retention
- Dry mouth
- Blurred vision
- Impotence
- Tachycardia
- Which typical antipsychotic causes photosensitivity?
- Chlorpromazine
- Which atypical antipsychotic causes Leukopenia/Agranulocytosis?
- Clozapine
- Which atypical antipsychotic causes prolongation of the QT interval?
- Ziprasidone
- Which antipsychotics have the highest risk of metabolic syndrome?
- Olanzapine and clozapine (Hence rule out family history of Obesity, DM, HTN, Dyslipidemia and Cardiovascular disease; measure BMI, Weight circumference, BP, FBS/HbA1C and Lipid profile)
- How do antipsychotics change the seizure threshold?
- They lower the seizure threshold
Extrapyramidal Symptoms (EPS)
Extrapyramidal symptoms are movement symptoms primarily caused by typical antipsychotics. Can be prevent by using atypical antipsychotics for long-term use. If, using a typical antipsychotic (haloperidol), keep an eye out for acute dystonia which presents within hours to days of treatment. The most serious EPS is tardive dyskinesia (it is irreversible)
Acute dystonia (hours to days)
Spasms of muscle groups of the body that are sustained and painful
- Signs and symptoms
- Torticollis (involves muscles of the neck)
- Oculogyric crisis (fixed gaze, eyes roll, cannot return)
- Opisthotonus (Widespread muscular spasm)
- Treatment
- IM anticholinergics (Benztropine, Trihexphenydyl) OR Antihistamine (Diphenhydramine) OR Benzodiazepines
- Then switch to an SGA or continue secondary prophylaxis with Procyclidine or Diphenhydramine (especially in patients receiving IM Haloperidol)
Akathisia (months)
Basically subjective restlessness and anxiety that presents objectively as fidgetiness
- Treatment
- Reduce or discontinue the neuroleptic. Change to an atypical antipsychotic if possible.
- If it continues use beta-blockers (1st line), benztropine (2nd line) or benzodiazepines (3rd line)
Tardive Dyskinesia (somewhat irreversible)
- Mechanism
- Postulated to be due to dopamine receptor ‘supersensitivity’
- Signs and symptoms
- Chorea
- Involuntary movements of the facial muscles and jaws (Lip smacking, tongue protrusion, Foot tapping)
- Rabbit syndrome: rhythmic motion of the mouth and lips
- Treatment
- Switching to atypical antipsychotics or clozapine
- Valbenazine and deutretrabenazine can reduce symptoms but are expensive options
- Prognosis
- Reversed in <50 % of patients
Parkinsonism
- Signs and symptoms
- Cogwheel rigidity
- Mask-like face
- Bradykinesia
- Pill-rolling tremor
- Treatment
- Oral anticholinergics (benztropine and benzhexol) are first line
- Anti-parkinsonism agents e.g. amantadine): added or substituted as monotherapy if anticholinergic is ineffective
- Reduce or change neuroleptic
Neuroleptic Malignant Syndrome (NMS)
This is a MEDICAL EMERGENCY! Death can occur in 24 hours. Very important to note that untreated NMS has a 20% mortality rate. Eventhough it is rare, a high index of suspicion should be kept for any patient on antipsychotics presenting with its characteristic symptoms. The mechanism is complex but think of it as a dysfunction of Ca2+ release from the sarcoplasm.
- Signs and symptoms of NMS (FALTTERED)
- Fever (most common)
- Autonomic instability (tachycardia, labile hypertension, diaphoresis)
- Leukocytosis
- Tremors
- Tachycardia
- Elevated creatinine phosphokinase
- Rigidity (lead pipe, almost universal)
- Excessive sweating (diaphoresis)
- Delirium (mental status change)
- Investigations
- CBC: Leukocytosis
- CPK: elevated
- Treatment
- Immediately discontinue antipsychotics
- IV Dantrolene (MR – stops muscular rigidity and hyperthermia)
- Dopamine agonists (Bromocriptine Amantadine, Apomorphine) OR
- Benzodiazepines (Diazepam, Lorazepam; if mild symptoms/psychomotor agitation)
- Calcium Channel Blockers (for Hypertension)
- Supportive management
- Monitor vitals
- Adequate hydration
- Cooling pads
- Benzodiazepines ready in case of seizure activity