Alcoholism
Alcohol is the most significant, most commonly used, and most commonly abused drug. Intoxication is measured with blood alcohol concentration (BAC). It is a depressant (contrary to popular belief that it is a stimulant, as it can ultimately cause respiratory depression). The WHO recommends no more than 14 units of alcohol per week.
Alcohol use disorder (WHO, 1952) is defined as a chronic disease characterized by a fundamental disturbance of the nervous system manifested on a behavioural level by a state of physical dependence. AUD is common in occupations with flexible work schedules and those that facilitate access to alcohol
- How alcoholism manifests (WHO, 1952)
- Inability to stop drinking before drunkenness is achieved
- Inability to abstain from drinking because of the appearance of withdrawal
- Major predisposing factor for alcohol use disorder
- Excessive alcohol use in first-degree relatives: there is a 30-60% concordance in monozygotic twins – confirmed by adoption studies done in Scandinavian countries
- Screening tests for alcohol use disorder
- CAGE Questionnaire: specific to alcohol. Answering 2 or more of these as “yes” means the patient is dependent on alcohol. Most sensitive screening test, with a sensitivity of 60-100%
- Michigan alcoholism screening test (MAST): 13-item test, self-administered. Sensitivity 30-78%
- AUDIT test: 10-question audit. Sensitivity 38-40%.
- TWEAK test: tolerance, worried, eye-opener, amnesia, cut down. Sensitivity 79%
- Pathophysiology
- Chronic alcohol consumption enhances GABA mediated inhibition in the CNS and inhibits NMDA-type glutamate receptors
- Signs and symptoms of low levels of intoxication
- Euphoria
- Talkativity
- Signs and symptoms of high-levels of intoxication
- Clumsiness
- Emotional lability
- Sedation
- Nausea and vomiting
- Anterograde amnesia (blackouts)
- Confusion
- Coma
- Death
- Treatment of alcohol intoxication
- ABCs
- Intravenous fluids with thiamine
- Benzodiazepine e.g. chlordiazepoxide and diazepam ****on a scheduled basis to prevent Delirium Tremens
- Treatment of dependence (long-term)
- Alcoholics Anonymous (Group Psychotherapy)
- Acamprosate: interferes with glutaminergic signalling to reduce craving
- Naltrexone: antagonises endogenous endorphins to reduce craving
- Disulfiram (antabuse): blocks metabolism of alcohol via aldehyde dehydrogenase, causing acetaldehyde to accumulate. Hence when the patient takes alcohol they get flushing, palpitations and vomiting as a side effect.
- Why is chlorpromazine (and antipsychotics in general) avoided in patients presenting with alcohol intoxication?
- May worsen respiratory depression
- May induce seizures
CAGE Questionnaire
| CAGE | Question |
|---|---|
| Cutting down | Do you ever feel like you should Cut down on your drinking? |
| Anger | Do you feel Anger when people confront you about your drinking? |
| Guilt | Do you ever feel Guilty about your drinking? |
| Eye-opener | Have you used alcohol as an Eye-opener after waking up? |
Complications of Chronic Alcohol Use
Psychiatric complications of alcohol use
| Complication | Description |
|---|---|
| Alcohol Withdrawal | Withdrawal symptoms occurs within 6-12 hours after the last drink and can lead to Delirium Tremens |
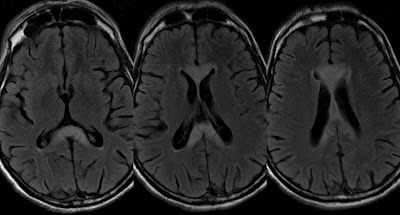
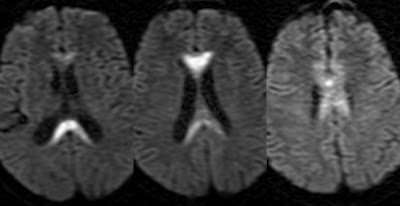
| Wernicke’s encephalopathy | Gliosis and haemorrhages in the limbc system, and structures around the 3rd ventricle and aqueduct due to thiamine deficiency |
| Korsakoff’s Syndrome | Permanent damage to structures in the limbic system leading to anterograde and retrograde amnesia |
| Alcoholic Dementia | Associated with white and grey matter loss |
| Cerebellar degeneration | A very common complication that occurs as a result of the loss of Purkinje cells in cerebellar cortex. Presents with dysarthria and limb ataxia |
| Alcoholic Hallucinosis | A rare complication with, but very characteristic if present. Can be permanent if it is not treated and persists for months. Presents with derogatory auditory hallucinations in the presence of a clear sensorium. The patient may be distressed (they are unpleasant and cause much anxiety to the patient). Treated with antipsychotics |
| Alcohol-induced depressive symptoms | Occurs in 80% of alcohol dependence. 1/3 male and 1/2 female dependent patients experience it. 15% of alcoholics die by suicide. |
| Alcohol-induce anxiety disorder | Occurs in 70% of heavy drinkers |
| Alcohol-induced Psychotic disorder (including Othello’s Syndrome) | Common in alcoholics. Othello’s syndrome is delusions of infidelity (of jealousy) of a significant other. Very difficult to treat and if attempts do not work divorce is advised. Can lead to homicide. |
Medical complications of alcohol use
| System | Complications |
|---|---|
| Central nervous system | Alcoholic Cerebellar Degeneration, Marchiafava Bignami Disease (demyelination/necrosis of the corpus callosum and related subcortical white matter in chronic ill-fed alcoholics due to B-vitamin deficiency), Central Pontine Myelinolysis, Traumatic brain injury |
| Gastrointestinal system | Erosive gastritis, Peptic ulcer, Pancreatitis, Liver disease (Alcoholic steatosis, Alcoholic hepatitis, Alcoholic cirrhosis) |
| Cardiovascular system | Hypertension, Cardiomyopathy, Arrhythmia, Congestive Heart Failure, Cerebrovascular accident |
| Genitourinary system | Testicular atrophy, Infertility, Miscarriage |
| Haemato-oncology | Macrocytic anemia, Cancer of the mouth and oral cavity, cancer of the oropharynx, cancer of the oesophagus |
| Fetal Alcohol Spectrum Disorder | Facial Dysmorphisms (Microcephaly, thin upper lip, Down-slanting eyes, Hypertelorism, epicanthal folds, receding chin), Systemic features (VSD, Heart-lung fistulas, Skeletal anomalies, Renal-aplastic or dysplastic, Growth retardation), and Intellectual disability |


Alcohol Withdrawal
Alcohol withdrawal occurs within 6-12 hours after the last drink. Withdrawal syptoms is what drives people to continue drinking. It may not be a severe illness. Withdrawal can lead to Delirium Tremens (DTs) which has a mortality rate of 5-15%. Withdrawal should be managed acutely to prevent progression to Wernicke-Korsakoff (permanent brain damage and amnesia)
Alcohol withdrawal
| Peak incidence (timeframe) | Features |
|---|---|
| 6 – 12 hours | Withdrawal symptoms |
| 36 hours | Seizures |
| 72 hours | Delirium tremes |
- Pathophysiology
- In alcohol withdrawal there is marked excitatory action mediated by the glutamatergic system (increased NMDA glutamate transmission) and decreased inhibitor GABA
- Signs and symptoms of alcohol withdrawal
- Tremor
- Anxiety
- Seizure or Hallucinations (characteristic of DTs)
- Insomnia
- Irritability
- Anxiety
- Tremors
- Loss of appetite
- Tinnitus
- Sweating (perspiration)
- Signs and symptoms of Delirium Tremens (DTs)
- Disorientation in time and place (as a result of reduced level of consciousness)
- Tremors (Marked)
- Visual, tactile and auditory hallucinations or illusions (symptoms tend to be worse in the evening and better in the morning; “Creepy Crawlies”/ formication)
- Sweating
- Tachycardia
- Hypertension
- Dilated pupils
- Ataxia
- Anxious (very very very anxious)
- Seizures (rum fits, less common – occurs in 5% of patients in withdrawal)
- Treatment of Delirium Tremens
- Admit (can be in the ICU)
- Supportive care
- Sedate the patient with a Benzodiazepine e.g. diazepam, lorazepam: no dose limit, give as much as is needed for sedation. Then taper.
- Dextrose bolus with Thiamine containing vitamin complex: this is continued for 3 months
- AVOID using antipsychotics (especially Chlorpormazine): may induce more fits
- Complications of alcohol withdrawal
- Post-withdrawal Wernicke’s encephalopathy
- Korsakoff syndrome (an anamnestic state)
Wernicke’s encephalopathy
Wernicke’s encephalopathy is caused by thiamine deficiency which causes gliosis and haemorrhages in structures around the 3rd ventricle and aqueduct. These structures include: mamillary bodies, hypothalamus, mediodorsal thalamic nuclei, colliculi, and mibdrain tegmentum. If not managed aggressively 80% of patients progress to the amnestic stage (Korsakoff’s syndrome).
- Functions of papez circuit
- Important in memory and forgetting
- Emotional control
- Signs and symptoms
- Global confusion (with extreme anxiety)
- Memory deficits
- Ataxia
- Ocular signs (horizontal nystagmus, weakness of lateral rectus, and conjugate gaze paralysis)
Korsakoff’s Syndrome
Korsakoff’s syndrome may appear without antecedent Wernicke’s encephalopathy. It is caused by permanent damage to structures in the limbic system. Lesions are in the dorsomedial thalamus (on histology). Anterograde and retrograde memory loss
- Signs and symptoms
- Clear sensorium (MMSE)
- Intact intellectual abilities (hence develops confabulation since they are aware they have memory deficits)
- Global amnesia
- Confabulation: subconsciously fills gaps in memory (intellect is conserved)
Wernicke-Korsakoff
| Strutures affected | Symptoms | |
|---|---|---|
| Wernicke’s (Acute) | Cerebellum, Brainstem, Mamillary bodies, Thalamus, Hypothalamus | Confusion, Ophthalmoplegia, Ataxia, Loss of appetite, Autonomic dysfunction, Peripheral neuropathy |
| Korsakoff’s (Chronic) | Papez circuit, Cerebellum | Amnesia, Confabulation, Behavioral symptoms |