Overview
Acute Coronary Syndromes (ACS) are synonymous with unstable angina (Chest pain lasting >10-20 minutes not relieved by rest) and may represent myocardial infarction (MI). They are caused by complete or partial occlusion of a coronary artery. ACS requires prompt admission and extensive care. The best initial step in managing a patient who presents with ACS is to get an EKG, adjunctive cardiac enzymes, and prescribe medications. NSTEMI and STEMI have elevated cardiac enzymes and are differentiated by an EKG. Unstable angina will not have elevated cardiac enzymes. Treatment is based on EKG and enzyme results. If the patient has positive enzymes but equivocal EKG results they are treated as NSTEMI.
Ischemic Heart Disease is the single largest cause of mortality worldwide. It affects Men > Women and incidence peaks after 60 years in men and 70 years in women (after losing the protective effects of estrogen). 50% of deaths occur within 2 hours of symptoms. 7% die before discharge.
Ischemic Heart Disease: An imbalance between myocardial perfusion and demand for oxygen
Myocardial Ischemia: Reduced blood supply +/- death of myocardial cells
Acute Myocardial Infarction: Death of myocardial cells with the release of cardiac enzymes (Troponins).
Silent Myocardial infarction: Asymptomatic infarction that occurs in 20% of cases. Common in the elderly and patients with Diabetes Mellitus
Types of ACS
| Type of ACS | Description | Findings |
|---|---|---|
| Non-MI Unstable angina | Angina of increasing frequency or intensity, or occurring at rest | No elevated enzymes |
| NSTEMI | ACS without ST-segment elevation | ST depression (Ischemia) + elevated enzymes |
| STEMI | ACS with ST-segment elevation or new-onset LBBB | ST elevation (Infarction) + elevated enzymes |
| Stable Angina | Unstable Angina | NSTEMI | STEMI | |
|---|---|---|---|---|
| Pain | Exertion | Rest | Rest | Rest |
| Relief | Rest + Nitrate | No | No | No |
| Biomarkers | No | No | Yes | Yes |
| ST changes | No | No | No | Yes |
| Stenosis | 70% | 90% | 90% | 100% |
- Emergency Treatment With presumptive EKG diagnosis while awaiting enzymes
- Give cardio-pulmonary resuscitation (CPR)
- Morphine 10-15mg IM or 1mg/min IV to alleviate pain and anxiety
- 100% Oxygen to improve saturation in patients with hypoxia or respiratory distress
- Glyceryl trinitrate 0.5mg sublingual q5-10min for a maximum of five tablets – to induce vasodilation and reverse vasospasm
- Aspirin 150 mg PO to reduce clot propagation thus preventing further damage to the heart
- Beta-blocker or Calcium Channel Blocker to reduce myocardial oxygen demand
Pathogenesis
- Risk factors for ACS
- Modifiable
- Cholesterol level (Target LDL < 100; <70 if diabetic)
- Smoking
- Hypertension
- Diabetes Mellitus
- Obesity
- Sedentary lifestyle
- Non-modifiable
- Age >60 years
- Male gender (and post-menopausal women)
- Family History of Myocardial infarction
- Modifiable
- Non-coronary artery (atherosclerotic) causes of Myocardial infarction
- Vasculitis (Polyarteritis Nodosa, Kawasaki disease)
- Cocaine use
- Thrombophilia (Antithrombin III deficiency, Polycythemia vera)
- Aortic dissection
- Iatrogenic (after revascularization procedure)
- Pathophysiology
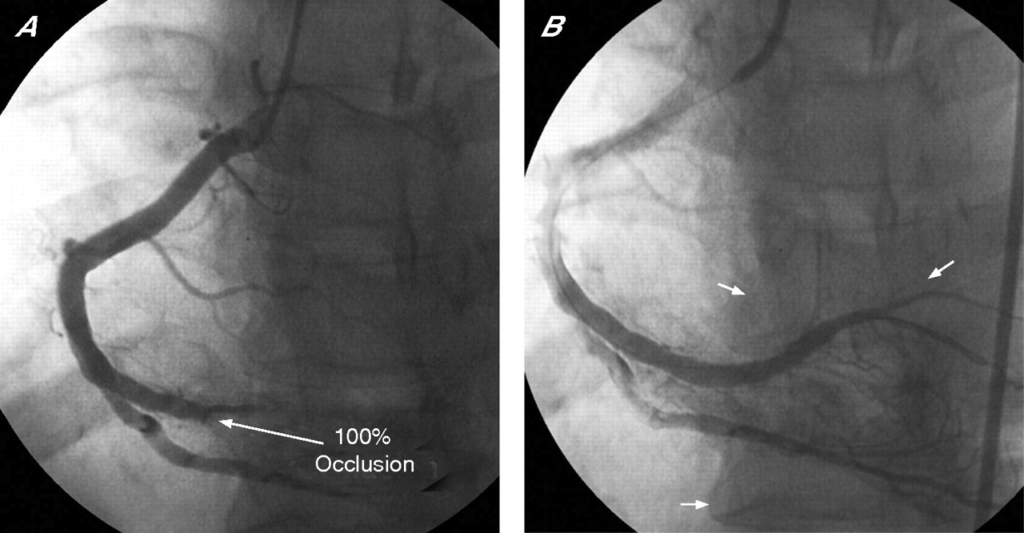
- Disruption of an atheromatous plaque in a coronary artery → subendothelial collagen and thrombogenic material (Tissue thromboplastin) are exposed → Platelets adhere to exposed material → occlusion of the artery by thrombus → Ischemia
- Irreversible myocardial injury
- Mitochondrial dysfunction: ischemia alters the permeability of the mitochondrial membrane, causing swelling, rupture of the outer membrane, and release of pro-apoptotic proteins
- Formation of superoxide free radicals: damage myocytes by altering membrane proteins and phospholipids
- Acute inflammation with neutrophil infiltration**:** reduces blood flow to ischemic tissue by occluding the capillary lumen (non-reflow phenomenon). Also releases proteolytic enzymes and reactive oxygen species.
- Activation of complement which further damages the endothelium
- Ischemia-reperfusion injury
- Spontaneous reperfusion or reperfusion following PCI/tPA → newly returning blood carries reactive oxygen species and ions → damage to the cell membrane → influx of Ca2+ → contraction of myofibrils → cytoskeletal damage and contraction band necrosis
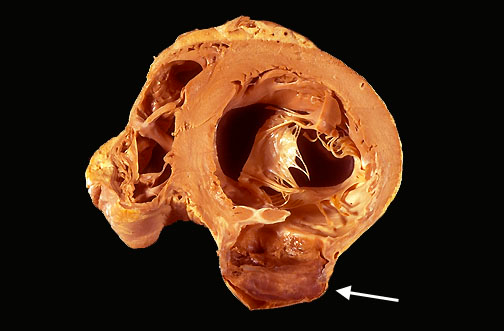
Gross morphology of myocardial infarction
| Time | Gross findings |
|---|---|
| 0 – 4 hours | None |
| 4 – 12 hours | Dark mottling; infarcted tissue |
| 12 – 24 hours | Dark mottling; infarcted tissue |
| 1 – 3 days | Hyperemia |
| 3 – 14 days | Hyperemic border with central yellow-brow pallor and softening |
| 2 weeks to months | Grey-white scar, recanalized artery |
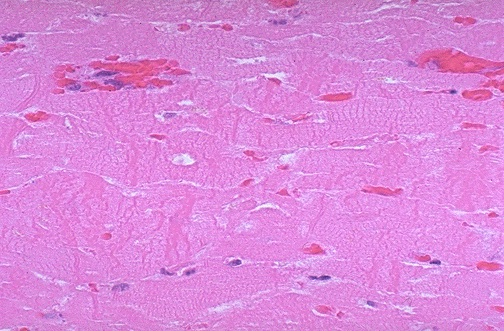
Histology of Acute Myocardial Infarction
| Time | Histological findings |
|---|---|
| 0-4 hours | None |
| 4 – 12 hours | Early coagulative necrosis |
| 12 – 24 hours | Coagulative necrosis, neutrophil migration |
| 1-3 days | Coagulative necrosis, neutrophil migration |
| 3-14 days | Macrophages, granulation tissue |
| 2 weeks to months | Fibrosis |


Clinical Features
- Signs and symptoms
- Chest pain
- Severe
- Retrosternal/epigastric
- Crushing or burning or discomfort
- Radiates to the neck and down the inner part of the left arm
- Last 20 minutes – 7 hours
- Occurs at rest
- Associated with pallor, diaphoresis, arrhythmia, hypotension
- Chest pain
- Differentials
- Stable angina
- Pericarditis
- Myocarditis
- Aortic dissection
- Takotsuba cardiomyopathy
- Pneumothorax
- Gastroesophageal reflux
- Pancreatitis
- Musculoskeletal pain
Investigations
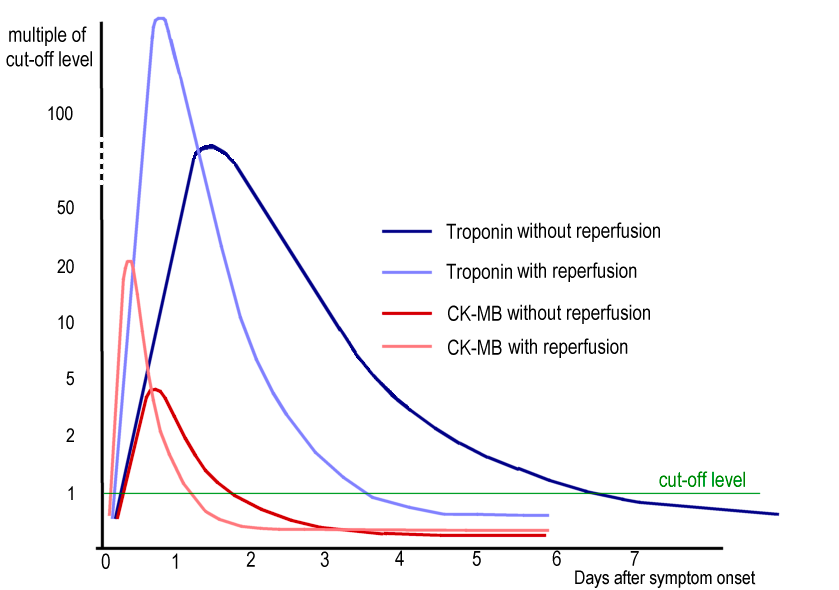
- Investigations Serial testing is required to rule out infarction since neither CK-MB nor Troponins consistently appear in blood within 6 hours of ischemia
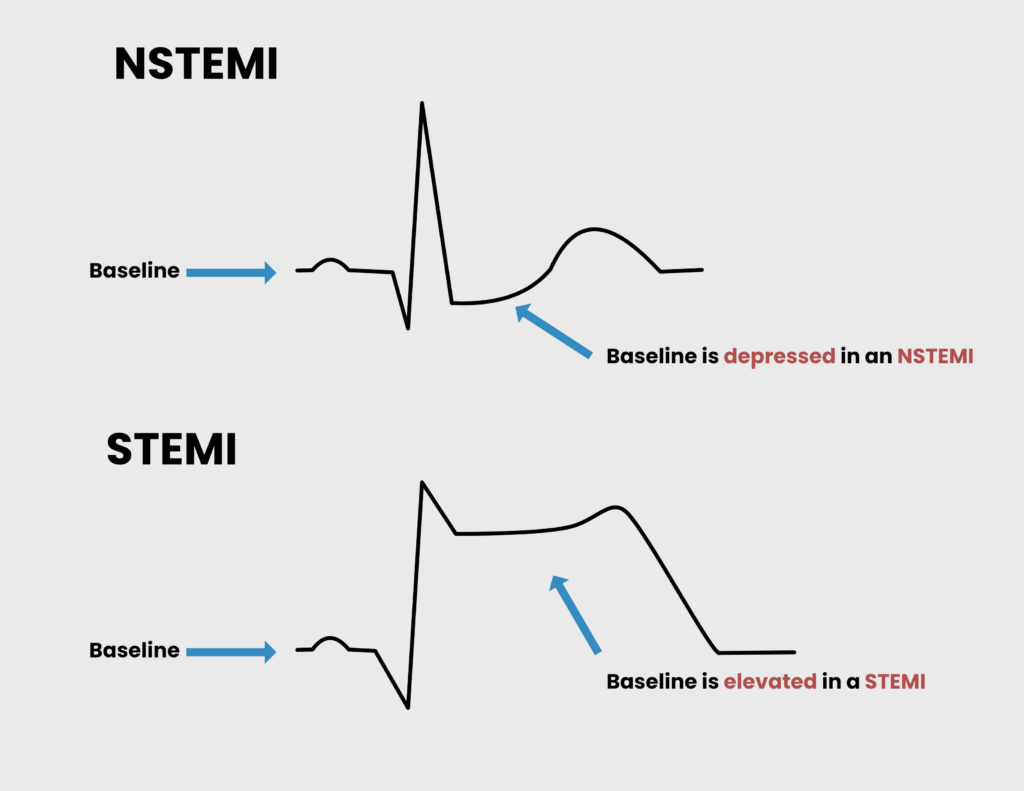
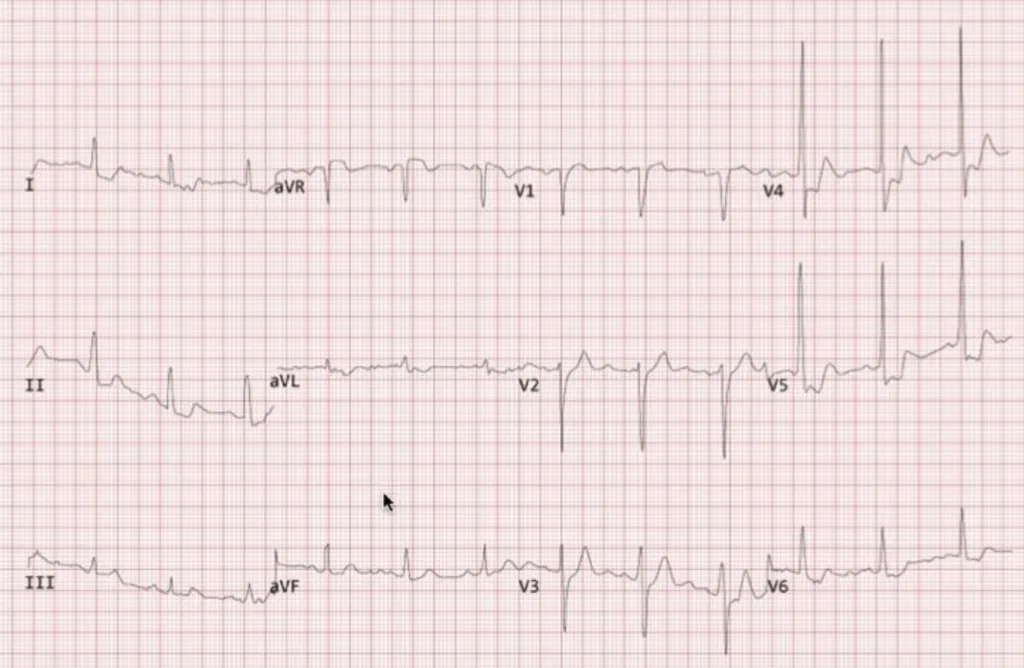
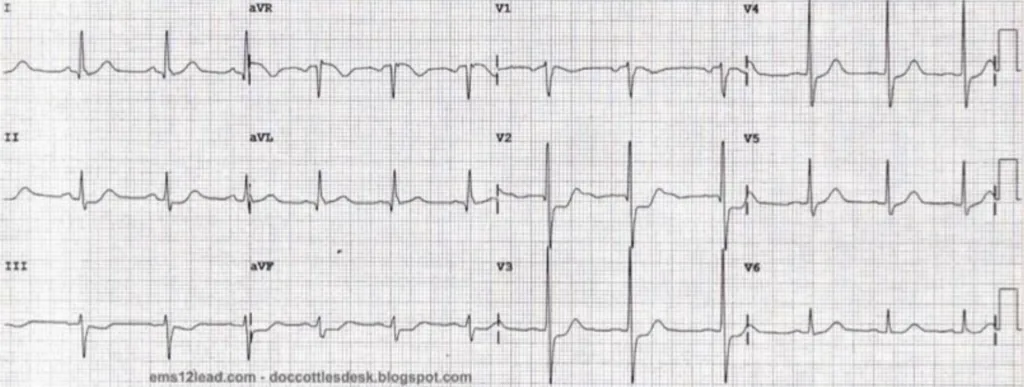
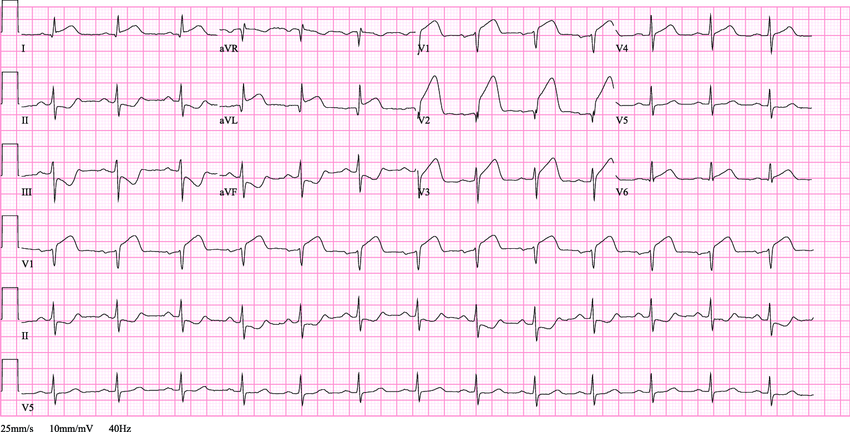
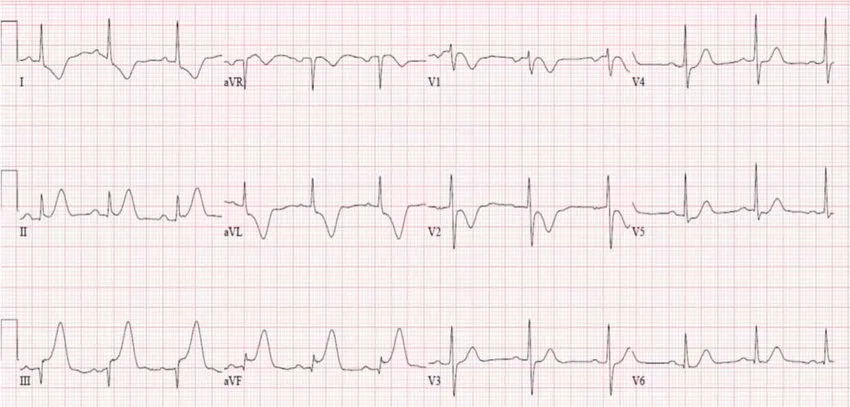
- Electrocardiography ****to determine whether it is NSTEMI or STEMI
- Inverted T-waves: areas of ischemia at the periphery of the infarct
- Elevated ST segment: injured myocardial cells surrounding the area of necrosis
- New Q waves: areas of coagulation necrosis
- Cardiac enzymes ****to determine whether there is infarction or not
- CK-MB: Good for assessing reinfarcion. Appears in the first 4-12 hours. Corrects within 3 days.
- Cardiac Troponins: Highly sensitive (96%). Appears within 3-12 hours. Corrects within 7-12 days.
- Echocardiography to look for regional wall abnormalities
- Chest X-ray to look for cardiomegaly, pulmonary oedema, or a widened mediastinum
- Other Labs: Complete blood count, U/E/C, Random Blood Sugar, Lipids
- Electrocardiography ****to determine whether it is NSTEMI or STEMI
STEMI vs NSTEMI
| EKG | Pathology | Treatment |
|---|---|---|
| NSTEMI | Occlusion that causes subendocardial ischemia | Heparin can be used to prevent clot extension |
| STEMI | More severe occlusion that causes transmural ischemia | Fibrinolytics (tPA) can be used to break the clot down |
- Definition of ST elevation
- Cut-off points
- ≥ 0.2 mV in men or ≥ 0.15 mV in women in leads V2-V3
- ≥ 0.1 mV in other leads
- Similarities between STEMI and NSTEMI Both cause cardiac enzyme elevation Both are life-threatening emergencies that require treatment Both can be classified as anterior, lateral, inferior, anteroseptal, etc.
- Differences between STEMI and NSTEMI
- STEMI infarcts have a higher early mortality rate compared to NSTEMI
- NSTEMI infarcts have an increased risk of re-infarction and Sudden Cardiac Death post-MI

Acute Management of ACS
Bottomline treatment of ACS
| Treatment | When to use it | Treatment goal |
|---|---|---|
| Statin | Any ACS | LDL < 70 and HDL > 40 |
| Beta Blocker | Any ACS | SBP < 140 and DBP < 90 |
| ACEi/ARB | Any ACS | SBP < 140 and DBP < 90 |
| Aspirin | Any ACS | No goal |
| Clopidogrel | Aspirin allergy or drug-elluting stent | |
| tPA | ST elevation or positive stress test when PCI or transport is unavailable | |
| Heparin | ST elevation or positive stress test when tPA is contraindicated | |
| Angioplasty (PCI) | ST elevation or positive stress test, 1 or 2 vessel disease | |
| CABG | ST elevation or ositive stress test, Left-mainstem or 3 vessel disease |
Acute Treatment of Unstable Angina or NSTEMI
Diagnosis of Unstable Angina/NSTEMI is no ST elevation (> 1mm in > 2 leads) ****nor new LBBB New ****Left Bundle Branch Block (LBBB) in the context of elevated enzymes is treated as NSTEMI.
- Emergency treatment
- Supportive care: Morphine, Nitrates, 100% Oxygen
- Aspirin
- Beta-Blocker or Calcium Channel Blocker (Verapamil, Dilitiazem) to reduce myocardial oxygen demand
- Heparin to prevent clot extension
- Definitive treatment
- Catheterization for Angiography and potentially Percutaneous Intervention
- Administer Clopidogrel and GpIIb/IIIa inhibitor – Eptifibatide, Tirofiban)
- Coronary Artery Bypass Graft (consult the surgeon)
- Catheterization for Angiography and potentially Percutaneous Intervention
- Indications for catheterization for Angiography and Percutaneous Intervention (PCI)
- < 12 hours onset
- The diagnosis is NSTEMI (positive cardiac enzymes)
- The patient has had prior intervention (PCI, CABG)
- The patient has CHF, CKD, Hypotension, or prolonged pain
- Indication for Coronary Artery Bypass Graft (CABG)
- >12 hour onset
- PCI has failed
Acute Treatment of STEMI
The diagnosis of STEMI is ST elevation (> 1mm in > 2 leads) OR new LBBB. Remember there is a 3-hour window to administer tPA. If recanalization with tPA is successful, the patient should be admitted and PCI done within 24 hours. If tPA is unsuccessful the patient should get a rescue PCI immediately. If PCI fails contact surgeon for Bypass surgery.
- Emergency treatment
- Supportive care: Morphine, Nitrates, 100% Oxygen
- Aspirin
- Beta-blocker or Calcium Channel Blocker to reduce myocardial oxygen demand
- Tissue plasminogen activator (Alteplase, Reteplase) within 3 hours to dissolve the clot and rescue reversibly damaged myocytes
- Definitive treatment
- Catheterization for Angiography and Percutaneous Intervention
- Administer clopidogrel + GpIIb/IIIa inhibitor – eptifibatide, tirofiban
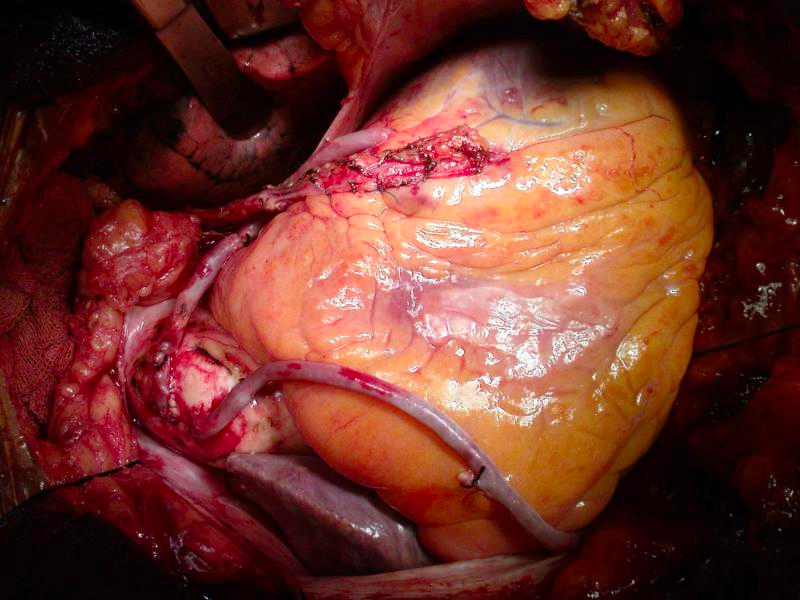
- Coronary artery bypass graft (CABG)
- Catheterization for Angiography and Percutaneous Intervention
- Why is tPA given instead of heparin in STEMI?
- The clot is already complete. We want to break down the clot with tPA (instead of preventing it from progressing)
- However, note that t-PA is NEVER the final treatment and it should be followed up with Percutaneous Coronary Intervention (PCI) or Coronary artery bypass graft (CABG) surgery
- What to do if t-PA recanalization is successful
- Admit the patient
- Perform Percutaneous Coronary Intervention (PCI) within 24 hours
- What to do if t-PA recanalization is unsuccessful OR patient > 3hrs from onset OR t-PA is contraindicated (recent bleed or surgery)
- Rescue Percutaneous Coronary Intervention (PCI) immediately
- What to do if Percutaneous Coronary Intervention (PCI) fails
- Coronary artery bypass graft (CABG) surgery (call surgeon)
Percutaneous Coronary Intervention (PCI) or Coronary artery bypass graft (CABG) surgery?
In stable angina, angiography will tell you WHETHER to do PCI or CABG (since the problem is little occlusions in multiple arteries)
- Indications for PCI in stable angina
- Single vessel disease
- Indications for CABG in stable angina
- Multiple vessel disease
- Left main artery disease
In unstable angina, angiography will tell you WHERE to do PCI or CABG (since the problem is an occluding thrombus in one artery). If PCI fails, do CABG.
In-patient management of Myocardial Infarction
After emergency management, all MI patients should be admitted to the coronary care unit (CCU). Should be closely monitored on telemetry (to detect V-Fib, arrhythmias, and monitor vitals). Frequent monitoring every 3-4 hours for Cardiovascular and Pulmonary symptoms. Any angina post-MI hospitalization period should be sent for CABG
Left Ventricular Ejection Fraction is the most significant prognostic factor for survival following MI.
- Investigations
- Echocardiogram: check for LV function and geographical damage done to the heart
- Serial Cardiac enzymes: to detect re-infarction
- Medications
- Aspirin: decreases mortality 😃
- IV beta-blockers: decrease mortality😃
- Anticoagulation with Heparin or Fondaparinux (INR 1.5 – 2.5): decreases mortality😃
- Nitroglycerin: for comfort
- Morphine: for pain
- High-dose Statin: The majority of patients with Myocardial infarction will have hypercholesterolemia
- Supportive therapy
- Strict bed rest for 24-48hrs: prevent heart rate from rising
- 100% oxygen: to keep SpO2 at 100%
- Gradually rehabilitate to activity after 48 hours
Outpatient management of MI
After discharging the patient, we want to minimize the risk of developing MI down the road. Make sure they are on a very strict medical and lifestyle regimen. Follow-up within 2 weeks of discharge.
- Discharge medications
- Aspirin*: all patients for life; reduces clotting (reduce mortality) 😃
- Beta-Blocker:* all patients for life; reduces Oxygen demand (reduce mortality) 😃
- Clopidogrel*: all patients, for at least 9-12 months; reduces clotting (reduce mortality)😃
- Statins*: all patients; don’t want them to have more plaques (reduce mortality)😃
- Nitrates: In ****all patients, nitroglycerin > ISDN since can develop tolerance to ISDN – long-acting (reduce pain)
- ACEi or ARB*: for patients with LVEF <40% or symptoms of CHF
- Warfarin: for patients at risk of embolism due to A-fib, CHF
- Counselling and lifestyle management (secondary risk factor reduction)
- Hypertension: managed anyway with Beta-blockers (+/- ACEi or ARB particularly if the patient has Diabetes mellitus. Can also use Diuretics)
- Diabetes: strict management with diet or insulin therapy. Home BG monitoring. HgB A1C check q 3 mos.
- Cholesterol: statin is started in all post-MI pts.
- Smoking cessation
- Appropriate physical activity: walking → cycling → swimming → jogging
- OK to have Sex (Male patients may develop psychogenic erectile dysfunction. Diagnosed clinically. Can prescribe Sildenafil, but remember to discontinue nitrates)
- Stress testing for PCI/CABG (4-7 days after discharge. Protocol as in stable angina. Usually comes back positive. Workup for PCI/CABG afterward)
- Resume driving at 1 month
- Return to work at 3 months
- ABCDE mnemonic for Post-MI long-term management
- Aspirin, Anti-anginas (nitrates), ACEis/ARBs, Anticoagulation (warfarin)
- Beta-Blockers
- Clopidogrel, Cholesterol management (statins), Cigarette
- Diet and Diabetes Management
- Exercise and Education
Complications of MI
- Complications of MI
- Arrhythmia: most common complication (90%; any kind of arrhythmia under the sun, commonly bradycardia and AV block)
- Ventricular fibrillation: most common cause of sudden death
- Contractile dysfunction: The patient slowly starts developing CHF symptoms and a new murmur ( LV or RV dysfunction, hence the need for an echo)
- Mechanical dysfunction: The patient suddenly decompensates and has a new murmur (papillary rupture, septal rupture, free wall rupture, hence need for echo)
- Re-infarction: will have rebound CK-MB
- Other complications
- Cardiogenic shock (7%): survival is greatly improved by revascularization
- Anterior wall rupture: can produce cardiac tamponade
- Posteromedial papillary muscle rupture: seen as acute onset mitral regurgitation or LHF
- Interventricular septum rupture: seen as new RHF caused by left-right shunting
- Mural thrombus (10%): risk of peripheral embolization and stroke
- Fibrinous pericarditis: During the first week of STEMI. Presents as sub-sternal chest pain relieved by leaning forward and aggravated by leaning backward. Friction rub may be present.
- Dressler syndrome: Occurs after the first week of STEMI due to autoantibodies against pericardial antigens. AKA Autoimmune pericarditis
- Ventricular aneurysm: Occurs late (4-8 weeks) due to fibrosis. Complicated by HFrEF due to lack of contractile tissue.
Sudden Cardiac Death
Sudden cardiac death is unexpected death from cardiac causes in persons without symptoms of heart disease or within one hour of the onset of symptoms. Frequently occurs in the morning hours and evening as the adrenergic system kicks in on an already weakened heart.
- Risk factors for sudden cardiac death
- History of Myocardial infarction
- History of recent NSTEMI
- Obesity
- Diabetes Mellitus
- Hypertension
- Hyperlipidemia
- Left Ventricular Hypertrophy
- Non-atherosclerotic causes of sudden cardiac death
- Cardiomyopathy
- Aortic valve stenosis
- Mitral valve prolapse
- Cocaine
- Myocarditis
- Conduction defects
- Causes of sudden cardiac death in children
- Aortic valve stenosis
- Hypertrophic cardiomyopathy
- Wolff-Parkinson White Syndrome
WHO Criteria for the diagnosis of Acute Myocardial Infarction (AMI)
- Category A:
- Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99th percentile of the upper reference limit, together with evidence of myocardial ischemia with at least one of the following:
- Ischemic symptoms: Crushing chest pain that radiates to the left jaw, axilla, arm
- ECG changes consistent with new ischemia: new ST changes, or new left bundle branch block (LBBB)
- Development of pathological Q waves in ECG
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
- Sudden unexpected cardiac death, involving cardiac arrest, often with symptoms suggestive of myocardial ischemia and accompanied by:
- presumably new ST elevation or new LBBB
- evidence of fresh thrombus by coronary angiography and/or at autopsy
- Autopsy findings of an acute myocardial infarction
- Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99th percentile of the upper reference limit, together with evidence of myocardial ischemia with at least one of the following:
- Category B: if the requirements for diagnostic tests in Category A (above) have not been met, and:
- Both of the following criteria are present:
- Symptoms of ischemia
- development of unequivocal pathological Q waves
- Death with a history of coronary heart disease and/or documented cardiac pain within 72 h before death, and no evidence of non-coronary cause of death, or autopsy evidence of chronic coronary heart disease, including coronary atherosclerosis and myocardial scarring
- Both of the following criteria are present:
- Category C: definition and diagnostic criteria of probable MI
- The term probable MI should be used when there is insufficient information to decide whether or not there was an MI based on definitions in Categories A and B above, but/ or:
- Either one of the following is present in a person with symptoms of ischemia:
- development of unequivocal pathological Q waves
- incomplete information on cardiac biomarkers
- Autopsy findings suggestive of MI but not conclusive.
- Either one of the following is present in a person with symptoms of ischemia:
- The term probable MI should be used when there is insufficient information to decide whether or not there was an MI based on definitions in Categories A and B above, but/ or:
- NOTE: In all categories, several biomarker (troponin or creatine kinase (CK)-MB) determinations, which are all normal, exclude the diagnoses of MI or probable MI.