Overview
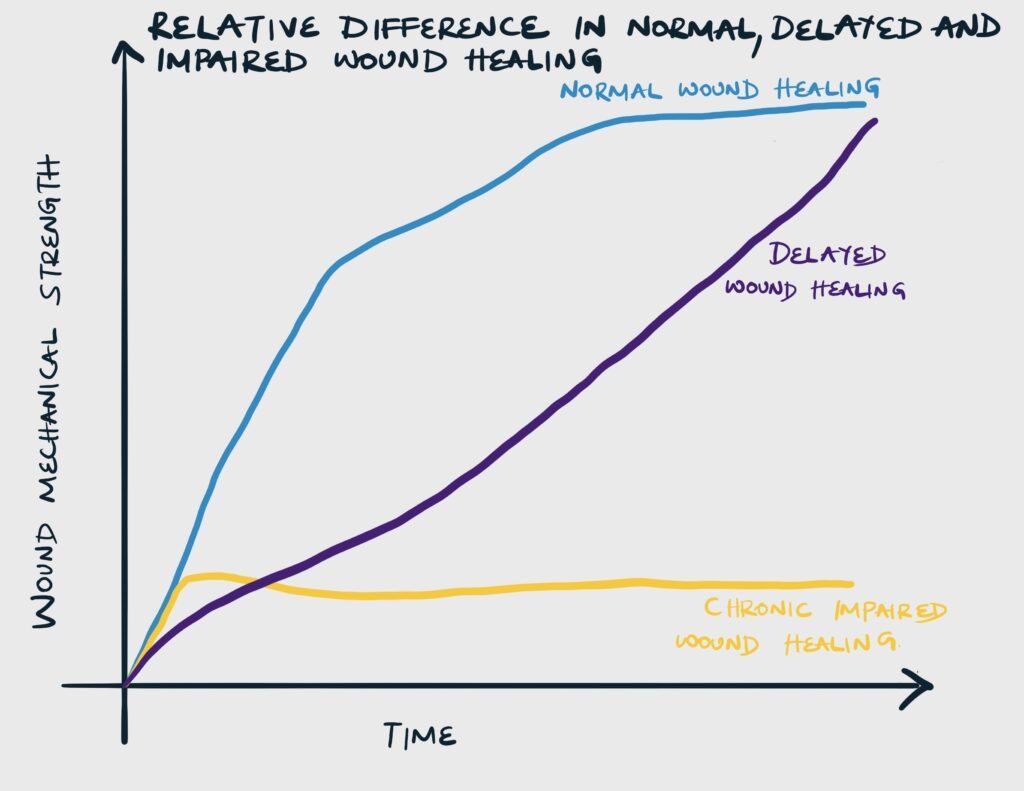
There are 2 major types of abnormal wound healing: impaired wound healing and delayed wound healing
Impaired vs Delayed wound healing
| Abnormal healing | Description | Cause |
|---|---|---|
| Delayed healing | Though at a slower rate of healing, the wound ultimately achieves mechanical strength as a wound that heals at a normal rate | Reversible underlying pathology, which when corrected allows the wound to heal |
| Impaired healing | The wound never reaches the strength of a wound that has healed normally | Related to immune compromised |
Acute vs Chronic Wound
| Type of wound | Description | Duration | Example |
|---|---|---|---|
| Acute wound | A wound that follows the orderly (continuum) steps of repair to achieve structure and function | Heals within 4-6 weeks | Surgical incision, Laceration e.t.c. |
| Chronic wound | A wound whereby the process of repair has been arrested (at the inflammatory phase) due to multiple reasons, thus failing to achieve the expected structure and function | Takes more than 4-6 weeks to heal | Diabetic ulcer, Decubitus ulcer |
Factors affecting wound healing
Local factors affect wound healing at the level of the wound. Systemic factors are conditions that involve the entire body that affect the ability of the wound to heal.
- Local factors affecting wound healing
- Infection
- Foreign material
- Necrotic or Devitalized tissue
- Hypoxia
- Ischamia
- Ionizing radiation
- Previous trauma
- Repeated trauma
- Venous insufficincy/edema
- Pressure
- Dessication
- Maceration
- Tension on wound edges
- Degree of approximation of wound edges
- Systemic factors affecting wound healing
- Advanced age
- Protein and Energy Malnutrition
- Vitamins and Mineral deficiency
- Metabolic disease e.g. Diabetes, Uremia, Cancer, Obesity
- Immunosuppression e.g. AIDS
- Immunosuppressive medications e.g. Steroids, chemotherapy
- Smoking
- Alcohol
- Cold temperature
- Connective tissue disorders e.g. Ehlers-Danlos, Osteogenesis Imperfecta, Acrodermatitis enteropathica
Infection
Bacteria interfere with wound healing by forming biofilm, producing endotoxin, releasing free radicals and consuming local oxygen. Clincally, an infected wound can be defined as a wound that is draining pus independent of culture results. A more narrow definition is a wound with a bacterial count of 10^5 microorganisms per gram of tissue. The best definition of wound infection, however, is a wound with multiplication of bacteria that overwhelms host defenses and results in wound damage and disruption of the healing process.
To identify wound infection, ask:
- Is the organism cultured normal flora?
- Does the organism typically cause infection of a wound
- Is there inflammation, tissue damage, or signs and symptoms?
- Erythema, pain, swelling, heat fever, and leukocytosis (any make infection more likely)
- Abscess, purulent or abnormal discharge, tissue discoloration or friabiliry, abnormal smell, unexpected wound breakdwon, rolled wound edges, or undermining (3+ make infection likely)
Colonization vs Contamination Vs Infection
| Term | Definition |
|---|---|
| Infection | Bacterial multiplication in a wound with an associated host reaction |
| Colonization | Bacterial multiplication without clinical evidence of infection or impaired healing. May progress to infection. |
| Contamination | Bacteria are present in a wound but are not multiplying and there is no host reaction. They have been introduced from an external source (direct contact, airborne or self-contamination from skin or GI tract) |
Examples of colonization
| Site or prosthesis | Organisms |
|---|---|
| Pressure ulcer | Skin flora (Staphylococcus spp.), Enteric flora (E. coli, Pseudomonas) |
| Skin wound or break | Skin flora (Staphylococcus spp.), Enteric flora (E. coli, Pseudomonas) |
| Upper Respiratory Tract | Mixed enteric flora in patients on antibiotics or those in a healthcare setting for more than 4 days, E. coli, Pseudomonas |
| Endotracheal or Tracheostomy tube | Mixed enteric flora in patients on antibiotics or those in a healthcare setting for more than 4 days, E. coli, Pseudomonas |
| Urinary catheter | Enteric flora (E. coli, Pseudomonas) |
Mechanical barriers, foreign material, and devitalized tissue
Foreign material prolong the inflammatory stage and prevent progression to the proliferative stage of wound healing. These material include necrotic debris (eschar or slough), suture material, retained dressing fibre, prosthesis, dirt, debris, and hematomas. They have to removed for wounds to heal.
Hypoxia
Oxygen is required in the hydroxylation of proline and lysine during collagen synthesis, and cellular respiration which are essential to wound healing. Hypoxia occurs in severe blood loss, hypotension, shock, ischemia, and increased tension on the wound.
Local oxygen can be improved by increasing FiO2 during and after elective surgery and by hyperbaric oxygen therapy, especially for patients with diabetes and radiation injury.
Ionizing radiation
Ionizing radiation causes atrophy, fibrosis, and impaired wound healing by causing DNA damage. DNA damage results in cell death and inhibition of mitosis.
Previous trauma
In previous trauma, there is scarring and fibrosis with reduced vascularization of the wound bed. This leads to decreased inflammation and impaired wound healing.
Venous insufficiency
Edema from hydrostatic pressure causes fibrinogen to leak and hemoglobin to extravasate. This causes skin damage and pruritus. Furthermore, fibrinogen polymerizes causing perivascular cuffing and impedes oxygen exchange. Edema alo dilutes bactericidal fatty acids making infection more likely
Advanced age
Older patients are more susceptible to wound dehiscence with less force than young patients. There is delayed epithelialization, slower wound contraction and higher rate of surgical site infections. Older patients also have a higher rate of comorbidities that independently impair wound healing.
Physiological changes associated with aging that inhibit normal wound healing include:
- Increased rate of collagen degradation due to increasd matrix metalloproteinase
- Increase in non-collagen proteins
- Delayed macrophage infiltration and impaired phagocytosis
Nutritional deficiency
| Nutrient | Role |
|---|---|
| Proteins | Hypoproteinemia causes a lack of critical amino acids required for collagen synthesis |
| Vitamin C | Required for hydroxylation of lysine and proline, and collagen cross-linking. Deficiency leads to decreased collagen synthesis and increased collagenolysis |
| Vitamin A | Vitamin A increased collagen production and epidermal growth factor receptors. Supplementation benefits wound healing in non-deficiency individuals, reverses the inhibitory effects of corticosteroids and promotes wound healing in patients with diabetes, chemotherapy, and radiation exposure. |
| Vitamin D | Essential for bone healing |
| Zinc | Multiple enzymes including DNA and RNA polymerase require zinc. Deficiency inhibits cell proliferation and granulation tissue thus impairing early wound healing. Supplementation is only helpful in deficiency individuals. |
Diabetes
Uncontrolled diabetes impairs wound healing by:
- Reducing host immune response and are 5 times more prone to infection
- Impairing angiogenesis
- Decrease collagen synthesis and increased collagen degradation (brittle collagen due to glycosylation)
- Ischemia due to large and small vessel vascular disease
- Renal failure resulting in ischemia
- Repetitive trauma and pressure ulceration due to peripheral neuropathy
Uremia
Uremia decreases collagen deposition and reduces the strength of collagen
Obesity
Obese patients have a higher risk of wound dehiscence, surgical site infection, incisional hernia, seroma, hematoma, fat necrosis and anastomotic leak. Adipose tissue produces adipokines and cytokines which impair cells necessary for wound healing.
Cancer
Impaired wound healing in cancer is often related to malnutrition which can occur due to:
- Cachexia
- Decreased nutrient absorption
- Decreased oral intake
There is also altered metabolism of nutrients:
- Increased glucose utilization
- Increased protein catabolism
- Inability to utilize fat over other sources for energy
Steroids
Steroids impair wound healing by:
- Impairing the inflammatory phase
- Impairing fibroblast proliferation and collagen syntehsis
- Reducing the amount of granulation tissue formed
Prescribing steroids can be delayed until 3-4 days post-operatively to minimize the impact on wound healing.
Chemotherapy
| Drug | Mechanism |
|---|---|
| Antimetabolites | Inhibit DNA and protein synthesis |
| Doxorubicin | Reduces platelets, inflammatory cells, and growth factors |
| Tamoxifen | Decreases cell proliferation. Increasing the dose decreases wound tensile strength |
| Bevacizumab | Impairs angiogenesis |
Smoking
Smoking impairs wound healing by:
- Impairing chemotaxis and cell migration
- Impairing phagocytosis
- Reducing fibroblast migration and proliferation
- Causing hypoxia
Connective tissue disorders
| Disorder | Effect |
|---|---|
| Ehlers-Danlos syndrome | Tissue friability makes suturing difficult |
| Osteogenesis imperfecta | Results in dermal thinning, increased bruising, brittle bones, and ligament and joint laxity |
| Acrodermatitis enteropathica | Inability to absorb zinc reduces cell proliferation and granulation tissue formation |



