Add a header to begin generating the table of contents
Endometrial hyperplasia is endometrial thickening with a proliferation of irregularly sized and shaped glands. Tends to be symptomatic in post-menopausal women. Endometrial hyperplasia in a post-menopausal woman (around 10mm) would be a normal endometrial thickness for a pre-menopausal woman in the secretory phase of her cycle. The class of hyperplasia is determined by histology. Endometrial tissue is extremely responsive to estrogen. Hyperplasia may be a precancerous lesion, although a majority do not develop into adenocarcinoma. Treatment depends on the age of the woman and whether or not there is atypia. MDPA or Megestrol is the medical treatment of choice.
1 in 38 women will develop endometrial cancer in their lifetime.
- Risk factors
- Hyperestrogenism (unopposed estrogen)
- High-dose menopausal estrogens
- Obesity (more aromatase more estrogen)
- Nulliparity
- Early menarche (≤ 11 years)
- Late menopause
- Use of Tamoxifen (SERM given for ER+ Breast cancer. Estrogen agonist in the uterus)
- PCOS (anovulation → unopposed estrogen)
- Type 2 diabetes, Hypertension, and Gallbladder Disease (may be independent, but occur more commonly in obese women)
- White race
- High socio-economic sttus
- Older age
- Living in North America or Northern Europe
- Hyperestrogenism (unopposed estrogen)
- Patient History
- Use of post-menopausal estrogen supplements
- Use of Tamoxifen
- Nulliparity
- Early onset of menarche and Late menopause
- Family History of malignancies (Lynch syndrome etc.)
- Ensure that pap smear is up to date
- Signs and Symptoms
- Abnormal uterine bleeding
- Post-menopausal women: Post-menopausal bleeding
- Pre-menopausal women: Menorrhagia, Intermenstrual spotting
- Abnormal uterine bleeding
- Physical Exam
- Pelvic exam (bimanual and speculum): feel for masses (fibroid, polyps, ovarian tumours), exclude lacerations, foreign bodies, cervical cancer
- Investigations
- Transvaginal ultrasound: measure the endometrial stripe. Imaging modality of choice.
- For post-menopausal women:
- Endometrial stripe < 5mm: Likely endometrial atrophy
- Endometrial stripe ≥ 5 mm: Likely endometrial hyperplasia
- For pre-menopausal women
- Normal endometrium varies from 4 – 16 mm
- For post-menopausal women:
- Endometrial biopsy
- Labs:
- Qualitative hCG
- CBC (haemoglobin)
- TFTs
- Transvaginal ultrasound: measure the endometrial stripe. Imaging modality of choice.
- Indications for endometrial biopsy
- Age > 40 years
- Risk factors for endometrial carcinoma
- Significant intermenstrual bleeding
- Failure of medical treatment for abnormal bleeding
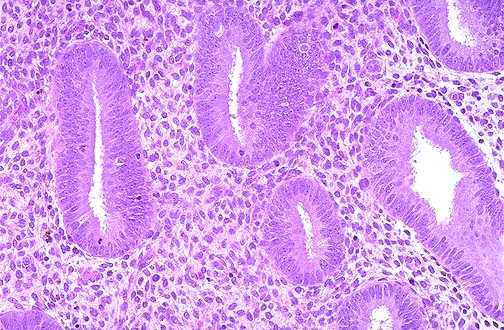
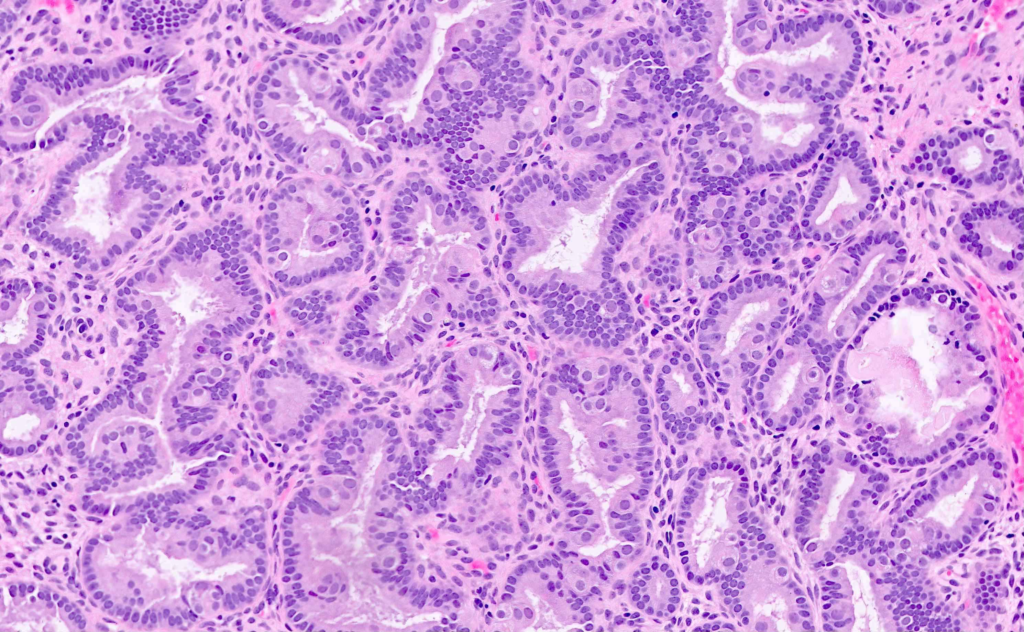
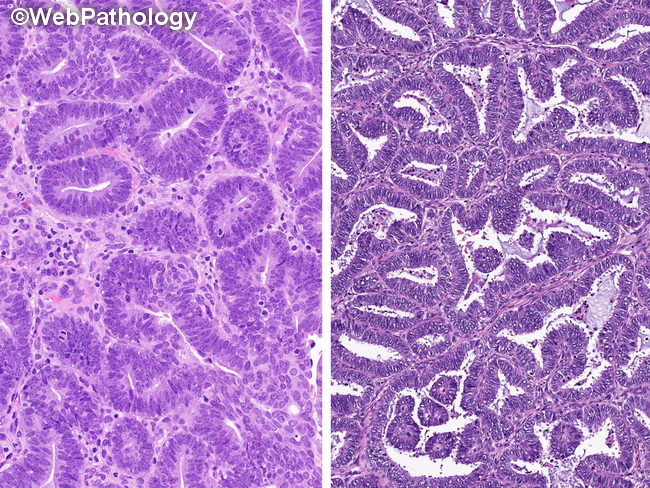
Terms used to describe the histology of endometrial hyperplasia
| Term | Description |
|---|---|
| Simple | Normal endometrial architecture but increased glands and stroma (ratio may be slighly increased > 1:1) |
| Complex | Changes in endometrial architecture (crowding, invaginations) and/or increased gland to stroma ratio (> 3:1) |
| Atypia | Changes in the nuclear structure of the cells (prominent nucleoli, salt-pepper chromatin, mitotic figaures etc…) |
Risk of progression to cancer
| Histology | Risk |
|---|---|
| Simple without atypia | 1% |
| Complex without atypia | 3% |
| Simple with atypia | 8% |
| Complex with atypia | 29% |
- Treatment for hyperplasia with NO atypia
- Premenopausal: MDPA 10-20 mg qd for 12-14 days q1mos for 3-6 months
- Postmenopausal: MDPA 2.5 mg qd continuously for 3-6 months
- Stop progestins then Repeat biopsy after 2-6 weeks (when tissue returns to normal)
- If no response, MDP 40-100 mg qd or Megestrol 160 mg qd
- Treatment for hyperplasia with atypiaThe risk of cancer is so high
- Hysterectomy (most patients will be postmenopausal)
- High dose MDPA if preservation of fertility* (ability to bear children) is desired in premenopausal women