Endometriosis is the presence of endometrial glands and stroma outside the normal location, excluding adenomyosis. It is a hormonally dependent disease, and therefore commonly presents as cyclical pelvic pain. Prevents chiefly in women of reproductive age. Should be considered as a differential in a pt presenting with ongoing pelvic pain and infertility/subfertility. Sx may overlap with adenomyosis. Tx depends on specific sx, severity, location, and desire for future fertility.
Prevalence of 2-10%. More common in East Asians > whites > blacks.
- Risk factors
- Familial clustering (Increased incidence in first-degree relatives)
- Genetic mutations/polymorphisms (some gene mutation candidates have been considered as risk factors – PTEN, EMX2)
- Anatomic defects (increased incidence w/ outflow tract obstruction)
- Nulliparity
- Early menarche
- Late menopause
- Short menstrual cycle (< 27 days)
- Menorrhagia (> 1 week)
- Other environmental factors
- TCDD/Dioxins (industrial pollutants)
- Caffeine
- Alcohol use
- Protective factors
- Regular exercise
- High parity
- Longer duration of lactation
- Theories behind the cause of endometriosis
- Retrograde menstruation: dissemination of endometrial fragments into the peritoneal cavity d/t uterine hyperperistalsis/dysperistalsis. Explains endometriosis in women with outflow obstruction.
- Lymphatic/vascular spread: theory behind spread into weird tissues e.g. implants behind the eye
- Coelomic metaplasia (Meyer’s theroy): suggests that the parietal peritoneum is pluripotent and can transform into endometrial tissue. Explains why some men can get endometriosis (chronic pelvic pain with Hx of hyperestrogenism)
- Induction theory: exposure to estrogen induces tranformation of certain tissues into endometrial-like tissue. Ovarian surface epithelium can transform into endometrial like-tissue.
- Immune dysfunction: very complex…
- Pathophysiology
- Regardless of location of endometrial tissue it responds to the normal hormonal cycle resulting in:
- Production of inflammatory and pain mediators
- Infertility
- Nerve dysfunction
- There is increased prostaglandin and oestrogen formation leading to chronic inflammation (IL 1, IL6, IL 8, TNF alpha all play a role) = PAIN
- Premenstruation – the tissue is stimulated to grow by progesterone and oestrogen. They enlarge and undergo secretory changes and bleeding.
- However, surrounding tissues prevent expansion and enlargement of the hemorrhagic fluid causing an increase in pressure = PAIN
- Severe pain is seen in cases where there are deeply infiltrating lesions.
- Regardless of location of endometrial tissue it responds to the normal hormonal cycle resulting in:
- Signs and symptoms
- Chronic Pelvic pain (severity correlated with depth of invasion)
- Localized
- Radiating to the upper back or leg
- Pain Sx (chronic or cyclical, or cyclical superimposed on chronic)
- Dysmenorrhoea (pain precedes menses by 24-48H, Less responsive to NSAIDs and COCs)
- Dyspareunia (partly caused by implants in the uterosacral ligament)
- Dysuria (associated with cyclical frequency and urgency)
- Defecatory pain
- Infertility/subfertility (d/t disruption of tubo-ovarian structure, or implants in ovaries)
- Sx of intestinal obstruction
- Sx of urethral obstruction
- Urgency
- Frequency
- Can progress to post-renal failure
- Chronic Pelvic pain (severity correlated with depth of invasion)
- Physical exam
- Visual inspection
- Normal
- Speculum exam
- Normal
- Occasional blue or powder-burn red lesions which bleed easily
- Bimanual exam (variable)
- Uterosacral nodularity and tenderness
- Fixed retroverted uterus
- Enlarged cystic adnexal mass
- Fixed, firm posterior cul-de-sac
- Visual inspection
- Gynaecologic differentials
- Pelvic inflammatory disease (TOA, Sapingitis, Endometritis): Hx HOB and other infectious sx, Hx of untreated STDs
- Hemorrhagic ovarian cyst
- Ovarian torsion
- Primary dysmenorrhea
- Degenerating leiomyoma
- Ectopic pregnancy
- Investigations
- Labs
- CBC
- Urine hCG
- Urinalysis + culture
- Vaginal/Cervical culture
- Imaging
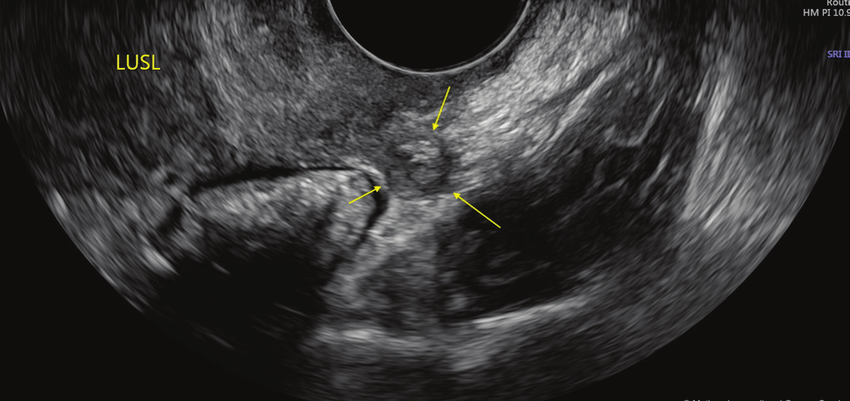
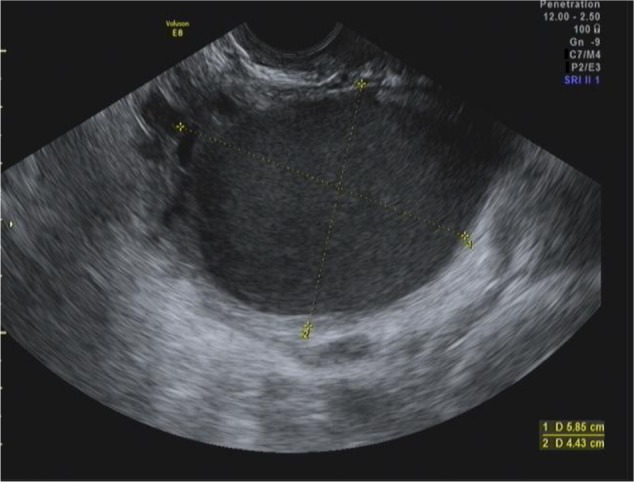
- Transvaginal ultrasound
- Uterine is not enlarged (generally, unlike adenomyosis)
- Chocolate cysts
- Nodules
- CT, MRI
- Transvaginal ultrasound
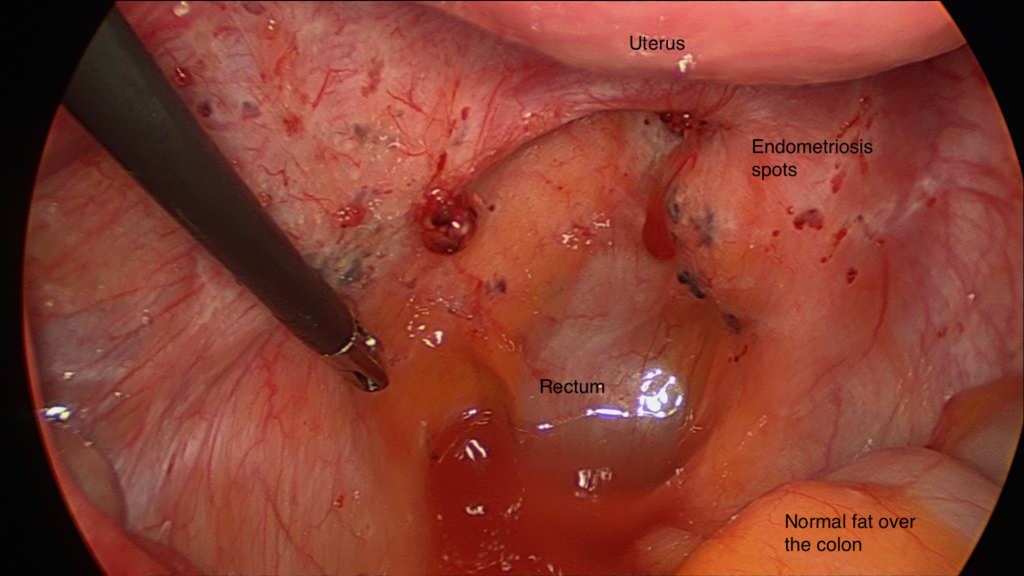
- Diagnostic laparoscopy: definitive dx
- Labs
- Medical Treatment
- NSAIDS (Ibruprofen, Naproxen): First-line Tx for primary dysmenorrhoea, pelvic pain prior to laparoscopy, or confirmed endometriosis w/mild sx
- Combined oral contraceptives (COCs)
- Progestins
- DMPA (decreases BMD)
- Norethindrone acetate (very effective with Leuprolide)
- Levonorgestrel IUD (Mirena)
- Ulipristal acetate(Ella)
- Mifepristone (off-label)
- Norethisterone
- Androgens (Danazol, Gestrinone; have a significant adverse effect profile)
- GnRH agonists (Leuprolide, Goserelin, Nafarelin)
- Aromatase inhibitors (Anastrozole, Letrozole; second-line tx)
- Surgical Treatment
- Lesion ablation w/ adhesiolysis
- Endometrioma resection
- Presacral neurectomy
- Hysterectomy w/ BSO: most definitive surgical tx. Considered in women who are done bearing children.