Intrauterine contraception (IUDs)
Levonorgestrel-releasing intrauterine system (LNG-IUS, Mirena): may be left upto 5 years
Copper T380 A IUD (Paragard T380): may be left in for up to 10 years
- Contraindications
- Pregnant
- Vaginal bleeding of unknown etiology
- Acute infection of reproductive tract
- Prior ectopic pregnancy
- History of STI in past 3 months
- Anatomic anomaly or fibroid uterus
- Menorrhagia (ParaGard)
- Current breast cancer (Mirena)
- Copper allergy, Wilson’s disease (ParaGard)
- Benefits
- Highly effective
- Good for “poorly compliant” patients
- Lasts several years
- Periods eventually stop or lighten
- Drawbacks
- Insertion and removal requires a trained provider
- Perforation and Pelvic inflammatory disease can occur
- Method failure can lead to ectopic pregnancy
- Can cause cramping and increased/prolonged bleeding

Progestin implants
Etonorgestrel subdermal implant (Implanon, Nexplanon): single-rod progestin implant, placed in the biceps groove. Covered in a polymer to prevent fibrosis reaction. Lasts for 3 years.
Levonorgestrel subdermal implant (Jadelle): 2-rod progesitin implant. Approved for 5 years
- Contraindications
- Pregnancy
- Current or past history of thrombosis or thromboemblic disorders
- Liver tumor (benign or malignant)
- Active liver disease
- History of breast cancer or current breast cancer
- Benefits
- Highly effective
- Good for “poorly compliant” patients
- Lasts for three years
- Less risk of expulsion
- Drawbacks
- Unexpected bleeding profile
- Spontaneous “Silent” expulsion
- More cumbersome to implant/replace

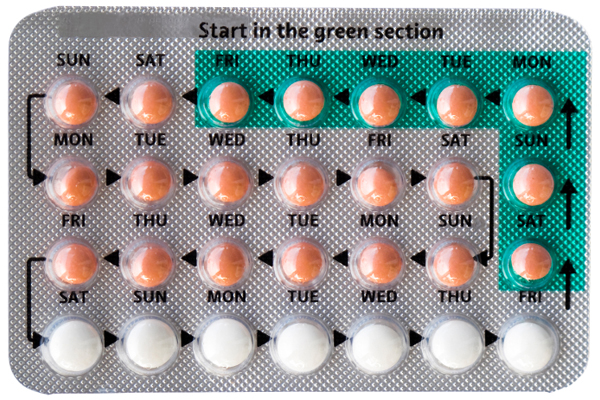
Combined oral contraceptive pills
Contains Estrogen and Progestin components which are taken in cycles. 30-35 ethinylestradiol; levenogestrel, norhestirone
Monophasic: Fixed dosage pill, followed by plaebos to induce withdrawal bleeding (i.e. 3 weeks on, 1 week off)
Multiphasic: Variable dosage pills, exposes to less hormones thereby reducing adverse effects
- Mechanism
- Anovulation
- Impaired follicular development
- Cervical mucus (progesterone)
- Endometrial hypoplasia (progesterone)
- Contraindications
- Pregnancy *or *nursing
- History of Thromboembolism/pulmonary embolism
- History of Coronary artery disease
- History of CVA
- Smoker > 35 years of age
- History of breast or endometrial cancer
- Unexplained vaginal bleeding
- Abnormal liver function
- Severe cholesterol or triglyceride elevations
- Migraines
- Seizure disorder (can interfere with seizure medications)
- High risk for vascular disease and over the age of 40 ** ****
- Hypertension
- Diabetes
- Complications
- Deep venous thrombosis
- Pulmonary embolism
- Cerebrovascular accident
- Myocardial infarction
- Hypertension
- Cholelithiasis
- Cholecystitis
- Hepatic adenoma
- Benefits
- Highly effective when take appropriately
- Reduces risk of endometrial and ovarian cancer
- Reduces risk of osteoporosis
- Treats a variety of disorders
- Drawbacks
- Must take pill daily
- Preparations may be confusing
- Long list of contraindications
- Long list of drug interactions
- Increased risk of cervical dysplasia and cancer
- Increased risk of gallbladder disease
- Increased risk of benign hepatic tumours (especially adenoma)
- Side effects: Nausea, headache, breakthrough bleeding, weight gain
Progestin-only pills
Small doses of progesterone taken daily without estrogen (taken every day of the cycle = no placebo leak). Missing a pill renders fertility for 48 hours.
- Side effects
- Irregular ovulatory cycles
- Breakthrough bleeding
- Increased formation of follicular cysts
- Acne
- Breast tenderness
- Risk of ectopic pregnancy
- Benefits
- May be take by women when oestrogen containing contraceptives are contraindicated
- Disadvantages
- Less effective (failure rate of 8%)
- Must take at same time every day
- Irregular menses
Injectable progestins
Depot-Medroxyprogeserone Acetate (DMPA, Depo-Provera): most common preparation. Administered every 90 days IM. Adverse effects and contraindications are similar to progestin-only pills.
- What is the most problematic side effect with injectable progestins?
- Bone demineralisation (maximum effect at 1 year then increases gradually with more years of use. Should take Vitamin D and do weight-bearing exercises)
- Benefits
- Highly effective
- Injections only needed every 3 months
- Reduces risk of endometrial, ovarian cancers
- Useful in treatment of menorrhagia, dysmenorrhea, endometriosis
- May be used in patient where oestrogen containing contraceptives are contraindicated
- Disadvantages
- Side effects: Irregular menses, depression/mood disorders, weight gain, may worsen premenstrual syndrome, premenstrual dysphoric disorder
- Bone demineralization
- Increased risk of cervical carcinoma in situ
- Delay in return of regular ovulation when discontinued (median of 10 months)
Patches
Norelgestromin/Ethinyl estradiol transdermal (Ortho Evra Patch): Applied for three weeks then taken off (analogous to COCs). Similar adverse effect and contraindication profile. Usage has declined due to litigation, but there is no evidence supporting increased morbidity with patch vs. other combined hormonal contraceptive methods.
Vaginal ring
Etonorgestrel/ethinylestradiol (NuvaRing)

