Bronchiolitis is an infectious, inflammatory process of the bronchioles. Primarily a disease of the very young (95% of cases occur in children < 2 years old). Always viral. Most commony caused by the Respiratory syncitial virus (RSV). Other causes include parainfluenza, adenovirus, metapneumovirus, bocavirus.
Diagnosis is clinical. The transient feature of bronchiolitis is wheezing which unfortunately has a long list of differentials. The patient’s age, history, symptoms, and clinical history wil give you a clue. The risk of respiratory distress is higher the younger the patient is.
Your first responsibility when seeing a child with “wheezing” or any other symptoms consistent with difficulty getting air in or out is to check the respiratory status which is done during the Px by determining the RR and SpO2. Treatment involves symptom relief to maintain hydration and oxygenation
- Risk factors
- Maternal smoking
- LBW/prematurity
- Perinatal complicaitons
- Perinatal or neonatal Antibiotic exposure
- Chronic disease
- Poor nutrition in nutero
- Environmental allergens/smoke
- Crowded conditions
- Poor Socioeconomic Status
- Risk factors for severe (complicated) bronchiolitis
- Preterm
- LBW/Preterm
- Age ≤ 12 weeks
- Chronic pulmonary disease
- Anatomic defect of the airway
- Hemodynamically significant Congenital Heart Disease
- Immunodeficiency
- Neurologic disease
- Patient History
- Prenatal/birth Hx
- Preterm
- NICU
- Intubated
- Maternal infections
- Maternal smoking
- PMHx
- Comorbid conditions
- FHx
- Immunodeficiencies
- Contacts w/recent RTI
- SHx
- Daycare
- Smokers in home
- Pets
- Home environment (dust, mould etc.)
- Prenatal/birth Hx
- Signs and symptoms
- Wheezing
- Sneezing
- Clear rhinorrhea
- Reluctance to feed
- Low-grade fever in some cases
- Severe Sx: Respiratory distress (Tachypnea, wheezy cough, dyspnea, irritability, apnea)
- Physical examination
- Monitor RR, Spo2
- Signs of respiratory distress (retractions, nasal flaring)
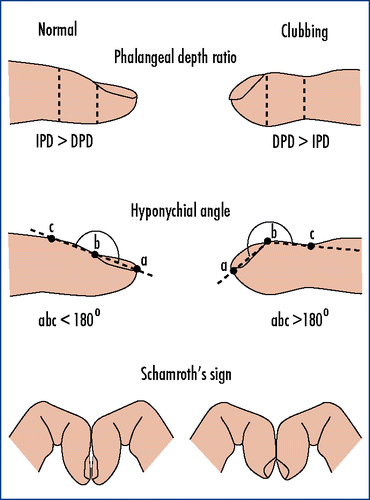
- Sx of chronic hypoxia? (digital clubbing, indicates repeated bouts of Respiratory tract infections)
- Auscultation:
- Wheezing (Monophonic or polyphonic?)
- Prolonged expiratory phase
- Is there stridor?
- Are the adventitious sounds lounder in the neck?
- Differentials
- Asthma: recurs, worse than most RSV episodes, look in pts Hx, if cannot be excluded try SABA (Albuterol). If does not resolve sx, do not continue use.
- Acute bronchitis: Similar Sx but cough predominates. Nasal discharge/sputum begins as clear then purulent then clear again. Self-limiting. Can occur in older children.
- Bacterial pneumonia: High-grade fever, looks toxic. Elevated CBC → CXR shows lobar consolidation. Sputum/blood cx should be performed
- Viral pneumonia: looks like bronchiolitis. Tachypnea is more common. RSV is a major cause of viral pneumonia in children 3 weeks-4yrs. NP swab is a diagnostic
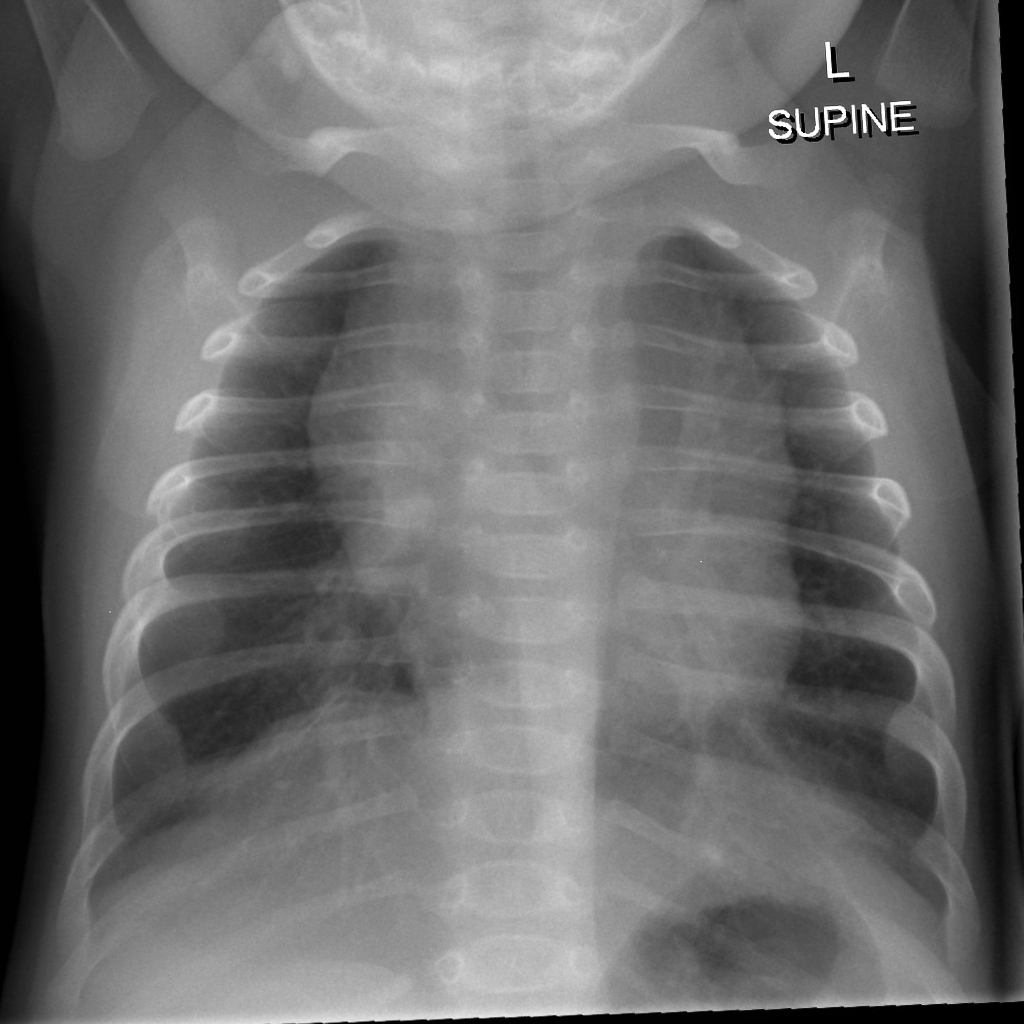
- CXR findings ***Not necessary in uncomplicated, straightforward cases. Always order AP and lateral
- Hyperinflation (≥ 9 posterior ribs in children, ≥ 11 posterior ribs in adults)
- Flattening of the diaphragm
- Patchy atelectasis
- Wall thickening
- Peribronchial cuffing w/air bronchograms
- Increased AP diameter
- Treatment
- RR and SpO2 monitoring
- Supplemental O2 (mandatory if SpO2 <90%)
- ABGs (wait and watch in uncomplicated cases)
- Nasopharyngeal swabbing for RSV analysis
- Nasal and oral suctioning
- IV fluids if dehydrated and cannot tolerate PO fluids
- When to admit children with bronchiolitis
- < 3mos. old
- Persistent resting SpO2 <92%
- RR > 70-80 rpm
- Any sx of respiratory distress: Especially AMOR use, cyanosis
- Pre-existing chronic lung disease
- Congenital heart defect
- Prematurity
- Inability to maintain PO hydration
- Intractable feeding difficulties
- Home care issues
- ATS/AACP recommendations for bronchiolitis
- Dx based on clinical findings (Hx, Px, Vitals) not lab/radiographic findings
- Risk factors should be assessed
- Beta-agonists should not be routinely usedl if used, continue using only if there is a positive clincial response
- Supplemental O2 necessary for pts w/SpO2 <90%
- Assess hydration and ability for PO intake
- Never use antibiotics
- Steroids should not be used
- Ribavirin should not be used
Finger clubbing
| Grade | Findings |
|---|---|
| Grade I | Nail bed fluctuation |
| Grade II | Obliteration of lovibond angle |
| Grade III | Parrot beaking (increased curvature of the nail) |
| Grade IV | Hypertrophic osteoarthropathy (HOA, drum stick appearance) |