Approach to Chest pain with Shortness of Breath
- Differentials for Chest pain + Shortness of breath (respiratory distress)
- Pulmonary embolism (pleuritic chest pain)
- Community-Acquired Pneumonia (pleuritic chest pain + fever + adventitious breath sounds)
- Pleurisy (pleuritic chest pain)
- Anemia (increased respiratory drive, no chest pain)
- Pneumothorax (will have absent breath sounds)
- Arrhythmia (because of tachycardia)
- Myocardial infarction (Zebra – familial hypercholesterolemia, coagulopathy – if miss you can get sued, must exclude MI with chest pain)
- Congestive heart failure
- Dissecting aneurysm (tearing chest pain)
- Pancreatitis (Stabbing chest pain)
- Initial management and investigations for chest pain+ respiratory distress (Shortness of breath, Tachypnea)
- SOB
- Supplemental Oxygen and pulse oximetry
- CXR
- ABG
- BMP
- Chest pain
- EKG
- CXR
- Cardiac enzymes
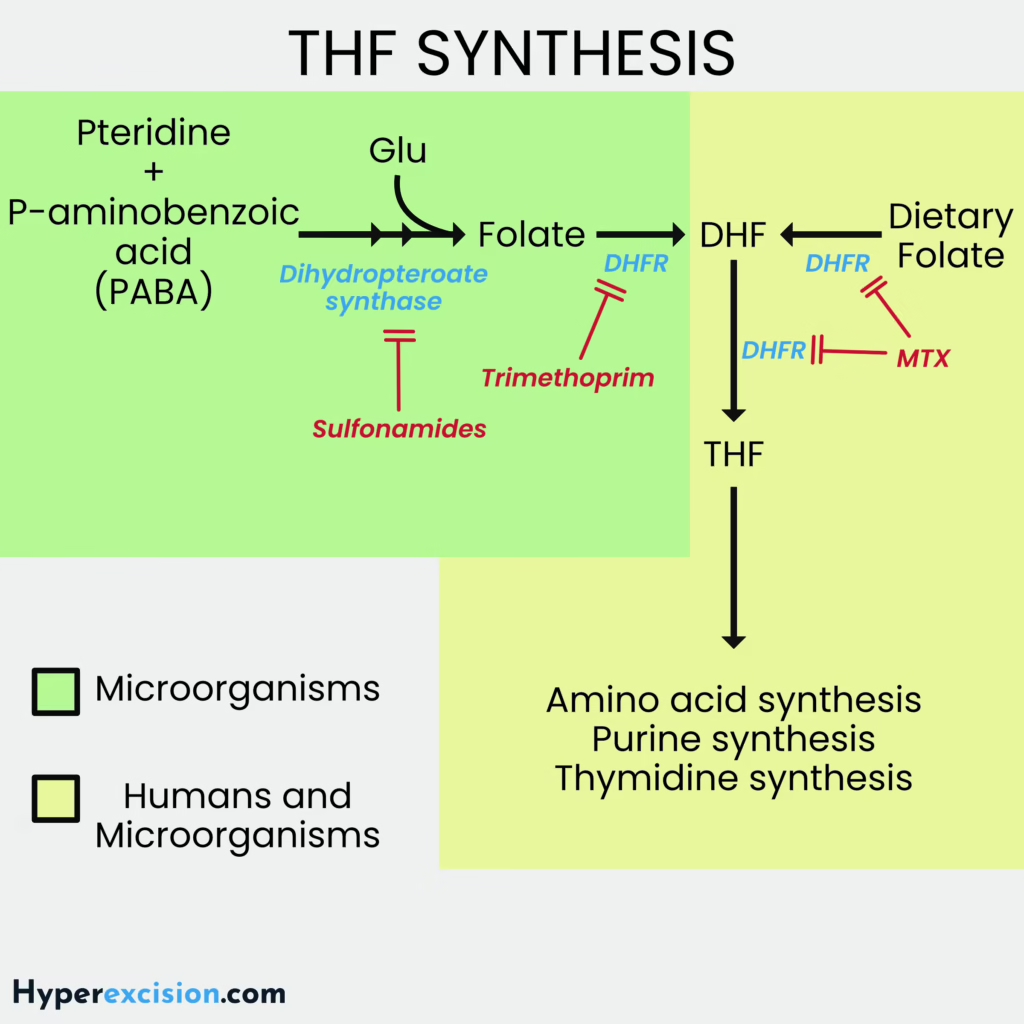
- Suspected Embolism
- D-dimer (Highly sensitive)
- BNP (right heart has to pump higher)
- SOB
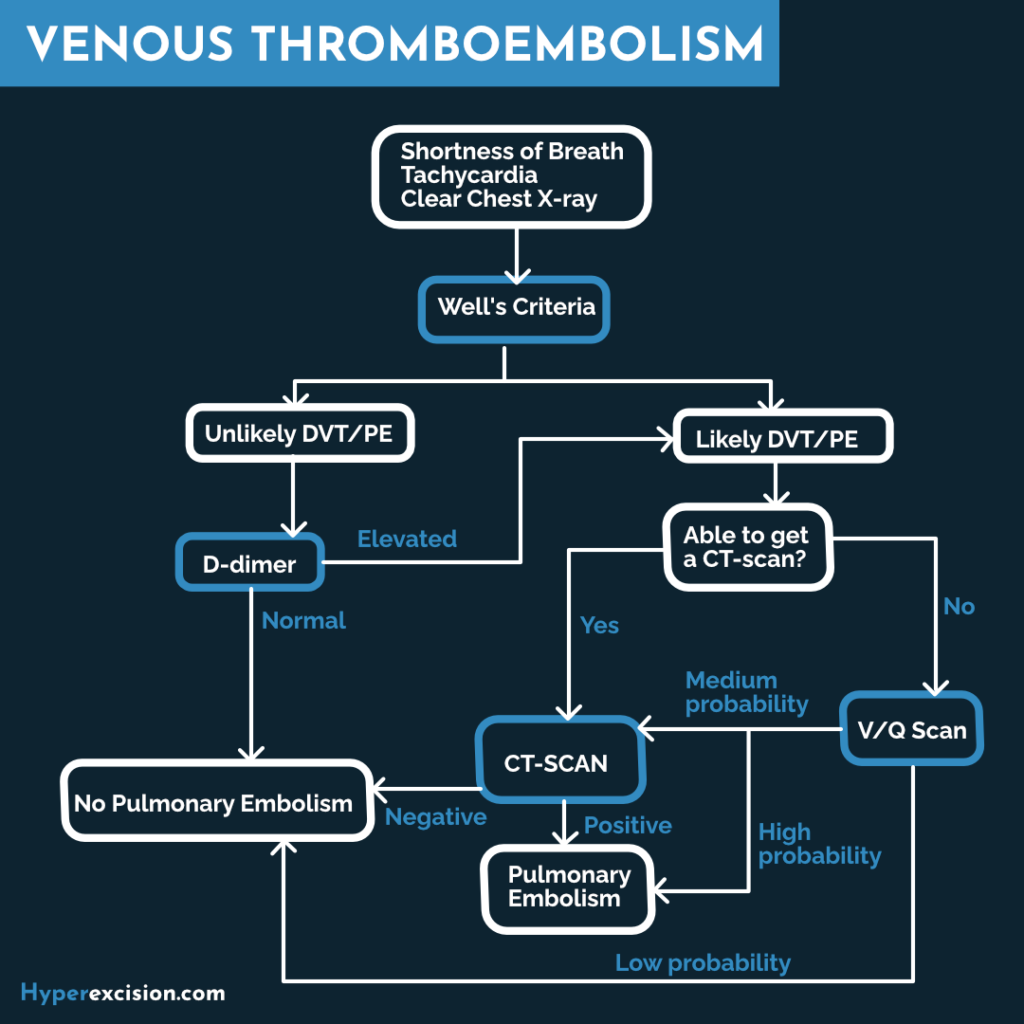
Wells score: pretest clinical probability scoring for DVT
| Criteria | Points each |
|---|---|
| PE most likely diagnosis (sx of DVT) | 3 |
| Heart rate > 100 | 1.5 |
| Immobilization | 1.5 |
| Surgery within 4 weeks | 1.5 |
| Hemoptysis | 1 |
| Malignancy | 1 |
| History of DVT or PE | 1.5 |
Well’s score for V/Q san interpretation
| Well’s Score | Intervention |
|---|---|
| < 2 | Small probability |
| 2 – 6 | Moderate probability |
| > 6 | High probability |
Well’s score for doing a CT Scan
| Well’s score | CT scan? |
|---|---|
| < 4 | No |
| > 4 | Yes |
Deep Vein Thrombosis (DVT)
DVT is the formation of a clot in a deep vein (thigh > calf > upper extremity). 50-70% of DVTs form PEs. May present coincidentally with PE (in this case make a presumptive diagnosis for PE and get spiral CT). Should eventually work up for hypercoagulability disorders (especially if risk factors are present)
- Risk factors
- Independent factors
- Age – increase in incidence is noted from age 30 to age 80
- Venous stasis
- Major surgery in last 4 weeks
- Obesity
- Immobility for longer than 3 days such as prolonged bed rest
- Polycythaemia rubra vera
- Thrombocytosis
- Dehydration
- Injury to the vessel wall
- Trauma
- Surgery
- Peripherally inserted venous catheters
- Previous DVT
- Intravenous drug abuse
- Hypercoagulability
- Drugs: Oral contraceptive pills (OCPs), exogenous hormones e.g. Estrogen
- Genetic deficiencies: Anticoagulation proteins C and S, antithrombin III deficiency, factor V Leiden mutation
- Autoimmune causes: Antiphospholipid syndrome, Systemic Lupus Erythematosus
- Pregnancy
- Malignancy
- Heparin induced thrombocytopenia
- Inflammatory Bowel Disease
- COVID 19 infection
- Nephrotic syndrome
- Sepsis
- Large burns
- Cardiovascular disease – myocardial infarction, heart failure, hypertension
- Smoking
- Diabetes
- Obesity
- Patient history
- Immobilized
- Post-op
- Prolonged sitting (long-distance travel)
- Acquired or inherited Hypercoagulability (OCPs, pregnant, inherited, hormones)
- Signs and symptoms
- Leg swelling and pain (measure 10 cm below tibial tuberosity)
- Warmth and edema of skin over the leg
- Pitting edema
- Homan sign (not usually performed since it might risk dislodging the embolus)
- Staging
- Provoked: Due to acquired states (surgery, oral contraceptives, trauma, immobility, obesity, cancer)
- Unprovoked: Due to idiopathic or endogenous reasons; more likely to suffer recurrence if anticoagulation is discontinued
- Proximal: Above the knee, affecting the femoral or iliofemoral veins; much more likely to lead to complications such as pulmonary emboli
- Distal: Below the knee
- Differentials
- All of these may coexist with DVT
- Cellulitis
- Erythema and skin warmth localised to a well-demarcated area; fever
- Evidence of skin breakage such as skin injuries, surgical incisions, intravenous site punctures, fissures between toes, insect bites, animal bites
- Ruptured Baker’s cyst – pain is sudden; visualised on ultrasound
- Superficial thrombophlebitis – palpable, indurated, cord-like tender subcutaneous venous segment can be felt on palpation
- Compartment syndrome
- Pain on passive flexion
- Lymphedema
- Firm, non-pitting; skin becomes scaly and thick (cobblestone appearance) and develops blisters with lymph fluid leaking.
- History of: familial involvement, malignancy, cancer treatment, injuries, severe burns, oncologic surgical procedures such as axillary lymph node dissection, Wuchereria bancrofti infection
- Chronic venous insufficiency
- Prominent varicosities
- Skin changes and hair loss
- Causes of fluid overload:
- Heart failure, cirrhosis, nephrotic syndrome
- Consider because generalised fluid overload may present with asymmetrical (and therefore apparently unilateral) edema.
- Lower limb fracture
- Cellulitis
- Investigations
- Whole blood clotting time
- Prothrombin time index (PTI0) and International Normalized Ration (INR)
- Dopple ultrasound
- Activated partial thromboplastin time (aPTT)
- Venography: confirmatory
- D-dimer: elevated
- Supportive Treatment
- Control pain
- Promote venous drainage
- Elevate involved limb
- Slightly elevated the foot of the bed (Trendelenburg position)
- Apply warm packs around the involved limb
- Encourage limited extension and flexion of the limb
- Encourage early ambulation as soon as pain and inflammation has resolved
- Graduated compression stocking to prevent post-phlebitic changes (pain, swelling, and skin changes seen in 10-30% of patients)
- Definitive Treatment LMWH > UFH. Use UFH in renal failure, or increased risk of bleeding. The dose will be guided by aPTT. Warfarin is started at the same time as heparin, and heparin is stopped once INR is 2-3 times the control. Warfarin is started at the same time as Heparin.
- Acute Phase Treatment
- LMWH (Enoxaparin) 1.5mg/kg/24H SC or Fondaparinux, or Dalteparin 200IU/kg/day SC OR
- Unfractionated Heparin 80 IU/kg IV bolus then 18 IU/kg/hour IV continuous for 2 – 5 days.
- Adjust dose to achieve aPTT 1.5-2.5 times the control
- Long-Term Anticoagulation
- Warfarin 10mg OD for 2 days. Adjust subsequent doses until INR 2-3 times the control for two continuous
- For calf DVT: continue warfarin for 3 months
- For proximal DVT: continue warfarin for 3 – 6 months
- Extend up to 6 months in patients with life-threatening clot at presentation
- Direct oral anticoauglants (DOACs – Dabigatran, Apixaban, Rivoraxaban): simpler dosing and monitoring and reduced bleeding risk
- Warfarin 10mg OD for 2 days. Adjust subsequent doses until INR 2-3 times the control for two continuous
- Acute Phase Treatment
- Duration for long-term anticoagulation
- Provoked: 3 months then assess risk-benefit profile
- Unprovoked: > 3 months if there is no identifiable risk factor
- Malignancy: for 6 months or until cured
- Pregnancy: LMWH until delivery or termination of pregnancy
- Why is warfarin started together with LMWH (Bridging anticoagulation)?
- Initial treatment using LMWH, UFH, Fondaparinux should continue for at least 5 days and until the international normalized ratio (INR) is 2 or higher for at least 24 hours. A vitamin K antagonist (VKA) such as warfarin should be initiated together with LMWH, UFH, or fondaparinux on the first treatment day.
- Warfarin interrupts the production of vitamin K–dependent coagulation factor production by the liver (Clotting factors II, VII, IX, X, proteins C and S).
- The effect is delayed by 72 hours until the existing circulating coagulation factors are cleared or used.
- The initial effect creates a hypercoagulable state because vitamin K–dependent anticoagulants (protein C and S) are cleared first from the body while vitamin K–dependent procoagulants continue to circulate.
- During this period, heparin anticoagulation is important to prevent worsening thrombosis. An international normalized ratio (INR) maintenance at 2-3 is recommended; higher ratios do not improve effectiveness, and lower ratios do not reduce bleeding complications.
- Preferred anticoagulant in malignancy
- Low Molecular Weight Heparin
- Absolute contraindications of anticoagulation
- Intracranial bleeding
- Severe active bleeding
- Recent brain, eye, or spinal cord surgery
- Malignant hypertension
- DVT prophylaxis
- Heparin 5000IU SC BD until the condition is treated, or
- Clexane 40mg/day SC
- Complications
- Post-thrombotic syndrome
- Manifests months to many years after the initial event
- Symptoms range from mild erythema and localized induration to massive extremity swelling and ulceration, usually exacerbated by standing and relieved by elevation of the extremity.
- The only current treatment is use of a compression stocking and leg elevation.
- Pulmonary embolism
- Bleeding from the use of anticoagulants
- Post-thrombotic syndrome
Warfarin dosage and target INR
| INR | <2 | 2 | 2.5 | 2.9 | 3.3 | 3.6 | 4.1 |
|---|---|---|---|---|---|---|---|
| 3rd dose | 5mg | 5mg | 4mg | 3mg | 2mg | 0.5mg | 0mg |
| Maintenance | ≥ 6mg | 5.5mg | 4.5mg | 4mg | 3.5mg | 3mg | Miss a dose then give 1-2 mg next dose. If INR > 4.5 miss 2 doses |
What to do when INR is too high?
| INR | Intervention |
|---|---|
| INR 5-8, no bleed | Withold 1-2 doses. Restart warfarin at lower maintenance dose once INR < 5 |
| INR 5-8, minor bleed | Stop warfarin and admit for urgent IV Vitamin K. Restart warfarin when INR < 5. |
| INR > 8, no bleed | Stop warfarin and consult hematology |
| INR > 8, minor bleed (e.g. epistaxis) | Stop warfarin and admit for urgent IV Vitamin K. Check INR qd and repeat Vitamin K if INR is too high after 24 hours. Restart warfarin when INR < 5. |
| Major bleed (including intracranial hemorrhage) | Stop warfarin. Give prothrombin complex concentrate 50 units/kg or FFP 15ml/kg ~ IL for 70kg man and add 5-10 mg Vitamin K. Consult hematology. |
Pulmonary Embolism (PE)
A pulmonary embolism is a clot that is lodged in the pulmonary arterial circulation. Various severity (between pleuritic chest pain to dropping dead…) Present with desaturation, elevated A-a gradient, and Right Heart symptoms (elevated jugular venous pressure, edema). The cornerstone of treatment is cardiopulmonary support, anticoagulation, and reperfusion (if necessary). Hemodynamically stable PE is treated with Direct Oral Anticoagulants. Unstable PE is treated with thrombolytics.
- Symptoms
- Signs of DVT (70% of pts)
- Pleuritic chest pain (worse on breathing)
- Respiratory distress/dyspnea
- Tachycardia
- Elevated jugular venous pressure
- Hemoptysis
- Investigations
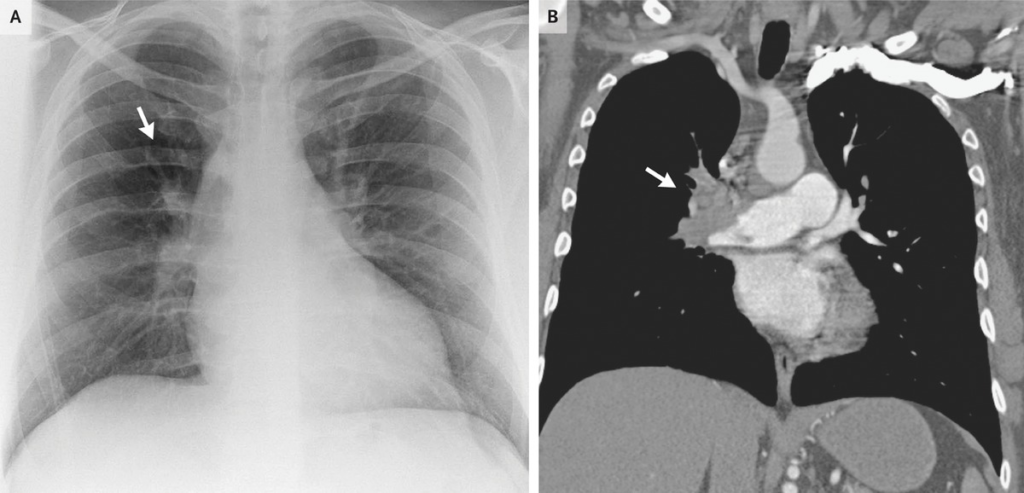
- Chest X-ray
- Dilated pulmonary arteries
- Linear atelectasis
- Small pleural effusion
- Westermark’s sign: wedge-shaped hyperlucency
- Hampton hump: Opacity with base at pleural edge secondary to infarction
- ABGs: respiratory alkalosis
- A-a gradient: elevated
- D-dimer: elevated
- BNP: elevated
- CT angiogram (Spiral CT): next best step to confirm embolism ****
- Angiography: most accurate but very dangerous (0.55 mortality); rarely done
- V/Q scan: done if there is a contraindication to CT (anaphylactic reaction to contrast, pregnant patient)
- Lower extremity doppler: if findings are consistent with DVT
- Echocardiography: to assess right heart strain
- Chest X-ray
- Signs of a hemodynamically unstable patient
- Hypotension despite fluids
- Hypoxia (cyanosis)
- Right heart strain on echo
- Treatment
- Admit (with continuous telemetry)
- Continue supplemental oxygen
- Hemodynamically unstable patient
- Thrombolytic (Alteplase)
- Mechanical clot removal
- Hemodynamically stable
- Unfractionated Heparin or LMWH for 5 days
- Start DOAC (Rivaroxaban, Apixaban, Dabigatran) or Warfarin (after stopping heparin when INR 2-3)
- Pregnant patient
- LMWH (Enoxaparin)
- Situations where anticoagulation is contraindicated
- Surgery for Pulmonary embolectomy and placement of IVC filter
- Continue long-term anticoagulation for at least 6 months after discharge
- Refer to hematology for hypercoagulation workup (suspected Factor V Leiden; affects long-term management)
- If the patient is older, workup for malignancy
- Contraindications to giving thrombolytics
- Absolute
- Prior intracranial hemorrhage
- Ischemic stroke < 3 months
- Suspected dissection
- Recent head trauma
- Recent surgery
- Bleeding diathesis
- Relative
- Age >75 years
- Pregnancy
- Current anticoagulants
- Cardiopulmonary resuscitation >10 minutes
- Uncontrolled hypertension (180/110 mmHg)
- Recent internal bleed (2-4 weeks)
- Absolute

Embolism vs thrombosis
| Embolism | Thrombosis | |
|---|---|---|
| Cardiac arrhythmia | Yes | No |
| Sudden onset | Yes | Sudden or slow onset |
| Severity | Severe | Less severe |
| History of claudication | No | Yes |
| Risk factors for PVD | No | Yes |
| Contralateral pulse exam | Normal | Abnormal |
| Exam findings of chronic limb ischemia | No | Yes |