Table Of Contents
Overview
This is weakness or paralysis of the facial muscles due to pathology of the facial nerve.
Course of the facial nerve
| Segment | Description |
|---|---|
| Intracranial | The motor nucleus is situated in the pons and emerges through the cerebellopontine angle to be joined by nerves intermedius (contains the sensory and autonomic components of the facial nerve). It enters the internal acoustic meatus which is located in the petrous part of the temporal bone. No branches are given at this point. It travels with the following in the IAM: Superior and inferior vestibular nerves, cochlear nerve, labyrinthine artery, vestibular ganglion |
| Intratemporal | This spans its course from the internal acoustic meatus to its exit through the stylomastoid foramen. It can be further divided into: labyrinthine segment (IAM to geniculate ganglion/first Genu). Narrowest portion of the nerve thus most sensitive to injury. Gives off the greater petrosal nerve. Tympanic segment ( geniculate ganglion to second genu). Mastoid segment ( second genu to stylomastoid foramen). Nerve to stapedius and chorda tympani branches leave at this point. |
| Extracranial | Spans from the stylomastoid foramen to the its terminal branches in the parotid gland. |
Branches of the facial nerve
For easy understanding you can revisit the distribution of these branches to understand the clinical presentation.
| Branch | Innervation |
|---|---|
| Greater petrosal nerve | Parasympathetic innervation to the lacrimal, palatine and nasal glands |
| Chorda tympani | Parasympathetic innervation of the submandibular and sublingual glands. Sensory innervation to the anterior two thirds of the tongue. |
| Nerve to stapedius | Motor to stapedius |
| Branches to occipitals, digastric, stylohyoid muscles | Motor to occipitals, digastic, and stylohyoid muscles |
| Temporal branch | Motor to frontalis to raise eyebrows |
| Zygomatic branch | Motor to orbicularis oculi to close eyes |
| Buccal branch | Motor to buccinator to puff cheeks |
| Mandibular branch | Motor to show bottom teeth |
| Cervical branch | Platysma to tense neck |
Functions of the facial nerve
Causes of facial nerve palsy by anatomic region
| Classification | Cause |
|---|---|
| Central | Brain abscess, pontine gliomas, poliomyelitis, multiple sclerosis, stroke or TIA |
| Intracranial | Acoustic neuroma, meningioma, congenial cholesteatoma, metastasis, meningitis |
| Intratemporal | Idiopathic (Bell palsy), Infections (acute and chronic otitis media), trauma (accidental, iatrogenic), neoplasms |
| Extracranial | Malignancy of parotid, injury to parotid gland |
| Systemic disease | Diabetes, hypothyroidism, uraemia, leukaemia |
- Patient History
- How long has the paralysis been present?
- Was the onset sudden or slowly progressive?
- Does it affect all nerve distribution or only part of the face?
- Associated symptoms: ear pain, fever, preceding viral illness, vascular symptoms (stroke or TIA), trauma, parotid mass
- Physical examination
- Full head and neck examination (including ears)
- Palpation of the parotid gland and face for masses
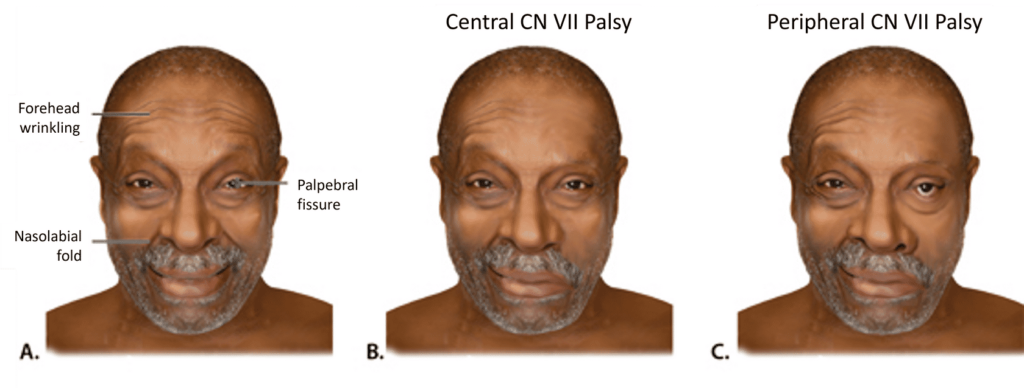
- Cranial nerve examination (emphasis on facial nerve and facial muscle function): wrinkling of the forehead, keep eyes closed against resistance to opening, smile to show teeth, and frown
- Clinical tests
- Blink test – tapping on the patient’s labella should stimulate blinking. Palsy will prevent that
- Schirmer test – testing for lacrimation using blotting paper
- Stapedial test – sensitivity to loud sounds. Done using tympanometry
- Salivary test – salivation rate is assessed from a submandibular duct following stimulation with a 6% citric acid solution.
- Taste test – using salt sweet, sour, and bitter tastes along the lateral aspects of the anterior two-thirds of the tongue.
- Investigations
- Nerve conduction studies
- Complete Blood Count
- C-reactive protein
- U/E/Cs
- VZV antibody titres
- Immunoglobulin titres (elevated in Lyme disease)
- Imaging studies: Ultrasound, CT or MRI
- Audiogram if there is hearing loss
- Imaging studies (CT-scan, MRI): for trauma or malignancy
- Conservative treatment
- Eye care: use of artificial tears, taping the eye closed as night
- Facial muscle therapy and massage
- Medical treatment
- Bell’s palsy: 50mg Prednisolone for 10 days, analgesia
- Ramsay Hunt syndrome: steroids, analgesia, antivirals (acyclovir)
- Treat ear infections appropriately
- Surgical treatment
- Facial nerve decompression
- Facial nerve repair and grafting
- Poor prognostic factors
- Age >50 years
- Complete palsy
- Loss of acoustic reflex
- Ramsay Hunt Syndrome
- Poor electrophysiological test results
- No signs of recovery after three weeks of treatment
- Associated comorbidites such as hypertension, diabetes, pregnancy
- Complications
- Exposure keratitis
- Disfigurement
- Hemifacial spasm
- Synkinesis – voluntary movement followed by involuntary movement
- Bell’s palsy
- Idiopathic cause of facial palsy. Presents as a unilateral lower motor neuron lesion.
- Risk factors include: Viral infection (HSV, CMV, EBV), diabetes mellitus, pregnancy
- Seen in 70% of cases. Should be a diagnosis of exclusion.
- Trauma
- Can be accidental or secondary to iatrogenic injury during surgery of surrounding structures.
- Fractures of the petrous part of the temporal bone should alert one to the possibility of a palsy. Associated symptoms include: battles sign, nystagmus, hemotympanum.
- Facial wounds transecting the nerve.
- Seen in 10-23% of cases
- Infection
- Viral (4.5%- 7%)
- Herpes zoster infection of the geniculate ganglion (Ramsay Hunt syndrome) causing facial paralysis as well as vesicular eruptions in the ear and soft palate due to CN IX involvement.
- Vertigo may be present due to CN VIII
- Bacterial
- Acute otitis media
- Meningitis
- Cholesteatoma
- Necrotising otitis externa
- Lyme disease
- Viral (4.5%- 7%)
- Neoplasia (2.2%-5%)
- An insidious onset of paralysis should alert you to malignant causes:
- Acoustic neuroma
- Parotid malignancies
- Meningioma
- Arachnoid cysts
- Pontile tumors
- Facial neuroma
- Metastatic lesions
- An insidious onset of paralysis should alert you to malignant causes:
- Special considerations Facial nerve palsy in children Can be acquired (similar causes as mentioned above) or congenital:
- Traumatic birth – forced delivery (causing facial injury), CS, high BWT, prematurity
- Syndromic causes – craniofacial abnormalities such as Arnold Chiari malformations
- Genetic causes – hereditary myopathies such as myasthenia gravis
- Lyme disease
- Guillan Barre syndrome
- Diabetes
- Sarcoidosis
Another way of classifying :
- Upper motor neuron lesion (forehead sparing) – stroke, subdural hematoma, multiple sclerosis, neoplasms
- Lower motor neuron lesion (forehead paralysis) – infective causes, trauma, idiopathic, neoplasms
Clinical presentation
Generally:
- Facial muscle weakness and paralysis
- Unable to close eyes, raise eyebrows, smile, show teeth, puff cheeks
- Hyperacusis
- Metallic taste on tongue
- Reduced lacrimation
Additional symptoms:
- Prodromal viral symptoms
- Vesicular eruptions in ear and soft palate
- Otalgia, hearing loss, otorrhea, tinnitus
- Masses – malignancy
House Brackman grading system – Normal Function to complete paralysis
| Grade | Description |
|---|---|
| I | Normal, symmetrical function |
| II | Slight weakness obvious on close inspection, slight asymmetry of smile |
| III | Obvious, non-disfiguring weakness, complete eye closure |
| IV | Obvious, disfiguring weakness, inability to completely close eyes and lift eyebrows. Normal facial symmetry at rest |
| V | Barely perceptible facial motion; asymmetry at rest |
| VI | Complete paralysis |
| Grade | Function level | Symmetry at Rest | Eye(s) | Mouth | Forehead |
|---|---|---|---|---|---|
| I | Normal | Normal | Normal | Normal | Normal |
| II | Mild | Normal | Easy and complete closure | Slightly asymmetrical | Reasonable function |
| III | Moderate | Normal | With effort, complete closure | Slightly affected with effort | Slight-to moderate movement |
| IV | Moderately severe | Normal | Incomplete closure | Asymmetrical with maximum effort | None |
| V | Severe | Asymmetry | Incomplte closure | Minimal movment | None |
| VI | Total paralysis | Total paralysis | Total paralysis | Total paralysis | Total paralysis |