Overview
Hypertensive Retinopathy is a disease of the retinal and choroidal vasculature due to severe acute or chronic hypertension.
Chronic hypertensive retinopathy is more common and is predominantly seen in older patients.
| Disease Process | Cause | Patients |
|---|---|---|
| Acute hypertensive retinopathy | Sudden, severe hypertension (commonly secondary hypertension) | Patients of any age |
| Chronic hypertensive retinopathy | Longstanding hypertension and atherosclerosis. Atherosclerosis causes retinal arterioles to expand and compress venules leading to branch retinal vein occlusion. | Older patients |
- Regulation of the retinal and choroidal vasculature
- The retinal vasculature is autoregulated. It loses it autoregulation as diastolic blood pressure exceeds 110-115 mmHg.
- The choroidal vasculature is regulated by the sympathetic nervous system
Acute Hypertensive Retinopathy
Acute hypertensive retinopathy is seen in patients with hypertensive crisis (BP > 200/110). Elevated blood pressure damages the retinal and choroidal blood vessels through fibrinoid necrosis and ischemic necrosis.
- Ophthalmoscopic findings
- Cotton wool spots: Ischemia to nerve fibers
- Uniform narrowing of arterioles and Tortuosity: uniform narrowing since all vessels are affected (unlike in chronic hypertensive retinopathy)
- Flame hemorrhages and dot blot hemorrhages: Necrosis and bleeding
- Papilledema (disc edema): Leakage from the arterioles supplying the optic disk. The optic disk appears confluent with the rest of the retina.
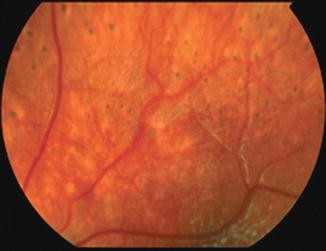
- Elsching spots: Damage to the retinal pigment epithelium
- Treatment
- Manage the hypertensive crisis.
- Avoid a steep reduction in BP as it can worsen damage
- Complications
- Retinal detachment: Due to damage and exudates in the choroid and Retinal pigment epithelium. Causes traction/exudative retinal detachment. Signs and symptoms – Acute change in vision, photopsia, floaters
- Optic neuropathy: ischemia of the optic nerve head due to vasoconstriction. Signs and symptoms – blurred disk margin, papilledema, flame hemorrhages
Chronic Hypertensive Retinopathy
Chronic hypertensive retinopathy is an end-organ manifestation of hypertension. Chronic hypertension accelerates the development of atherosclerosis. Atherosclerosis decreases the radius of arterioles. These arterioles expand to down-regulate resistance to flow and as the expand they compress the venules. Advanced forms of chronic hypertensive retinopathy causes a loss in visual acuity.
- Risk factors for chronic hypertensive retinopathy
- Age
- Black race
- FHx
- Smoking
- Obesity
- Stress
- Sedentary lifestyle
- Excessive alcohol consumption
- What additional risks do patients with chronic hypertensive retinopathy have?
- Stroke (7x)
- Myocardial infarction (4x)
- Coronary artery disease (3x)
- Peripheral artery disease (2x)
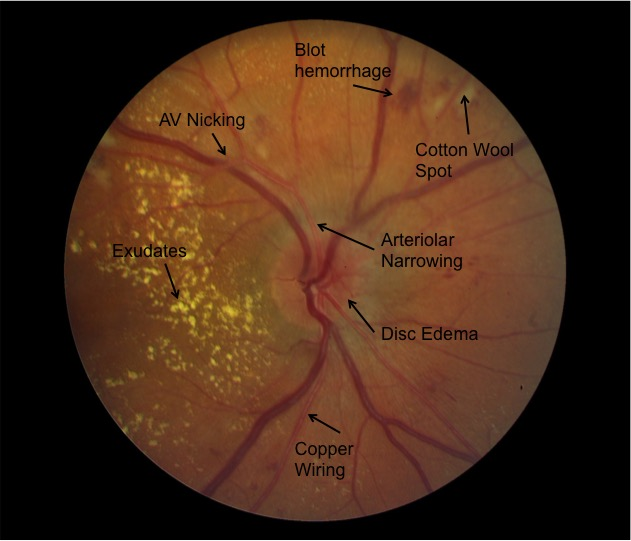
- Ophthalmoscopic findings
- Focal to Uniform narrowing of the arterioles
- AV nicking and AV crossing: due to arterioles compressing the venules. This is a hallmark finding of chronic hypertensive retinopathy
- Flame hemorrhage and dot-blot hemorrhage
- Copper-wiring and silver wiring: narrowing of the vascular lumen due to atherosclerosis
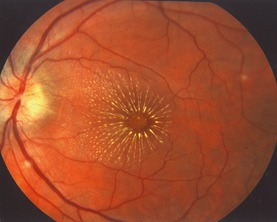
- Macula star: exudation around the macula in advanced chronic hypertensive retinopathy
- Treatment
- Manage the underlying hypertension
- Complications
- Branch retinal vein occlusion/ Central retinal vein occlusion: due to AV nicking/occlusion
- Retinal detachment: due to vascular fibrosis (tractional RD)
- Optic nerve atrophy: due to chronic optic disk swelling. Leads to decreased visual acuity.