Overview
Dacyrocystitis is an inflammation of the lacrimal sac usually as a result of obstruction of the nasolacrimal duct. It is the most frequent disorder affecting the lower lacrimal system and usually occurs unilaterally.
It may present acutely or chronically as well as in acquired or congenital forms.
Bimodal distribution in age with it occurring mostly in newborn infants ( congenital forms) or adults older than 40 years of age. Most common in women with 70-83% of cases occurring in females. More common among Caucasian individuals than Black due to anatomic differences such as a narrower nasolacrimal ostium and longer lacrimal canal in Caucasians.
- Risk factors
- The nasolacrimal duct is continuous with conjunctival and nasal mucosa which are colonised by bacteria making the duct prone to infection.
- Brachycephalic skulls – have a narrower inlet into the nasolacrimal duct, narrow lacrimal fossa and a longer nasolacrimal duct
- Flat nose and narrow face shapes – narrow osseous nasolacrimal canal
- Females are at greater risk due to their narrower duct diameter as compared to males
- Older age leads to the narrowing of the punctual openings, slowing tear drainage
- Dacryoliths; often idiopathic, are a collection of shed epithelial cells, lipids, and amorphous debris within the nasolacrimal system
- Nasal septum deviation, rhinitis, and turbinate hypertrophy
- Damage to the nasolacrimal system due to trauma of the nasoethmoid, maxillary (midfacial) bones or endonasal or maxillary procedures (e.g. maxillectomy)
- Neoplasm intrinsic or extrinsic to the system causing secondary nasolacrimal duct obstruction
- Systemic diseases such as granulomatosis with polyangiitis (GPA; formerly Wegener’s granulomatosis), sarcoidosis, and Systemic Lupus Erythematosus (SLE), or lacrimal sac tumors
- Medications such as timolol, pilocarpine, idoxuridine, and trifluridine or radioactive iodine which predispose to nasolacrimal duct obstruction
- Lacrimal drainage system
- Tears are produced by the lacrimal gland, found supero-laterally on the frontal bone lodged in the lacrimal fossa.
- After washing over the eye, the fluid is collected by the superior and inferior puncta found the medial surface of the eye.
- It flows through the superior and inferior canaliculi then further onto the common canaliculi.
- It crosses the valve of Rosenmuller into the lacrimal sac.
- It drains into the nasolacrimal duct, through the Valve of Hasner and into the nasal cavity.
Acute Dacryocystitis
Acute Dacryocystitis is acute inflammation of the lacrimal sac with symptoms occurring over several hours to several days. Diagnosis can be made clinically.
- Etiology Mostly caused by an infection by the following microorganisms
- Staphylococcus aureus
- Staphylococcus epidermis
- Streptococcus pneumoniae
- Haemophilus influenzae
- Pseudomonas aeruginosa
- Repeated trauma such as facial fractures
- Surgeries such as endonasal procedures
- Topical medication such as Timolol, pilocarpine
- Systemic medication such as fluorouracil
- Neoplasms such as primary lacrimal sac tumors and benign papillomas
- Pathophysiology
- First, there is obstruction of the nasolacrimal duct leading to retention and stagnation of tear fluid.
- The retained tear fluid creates a conducive environment for pathological microorganisms to invade and infect leading to the inflammatory state characteristic of the condition.
- Signs and symptoms
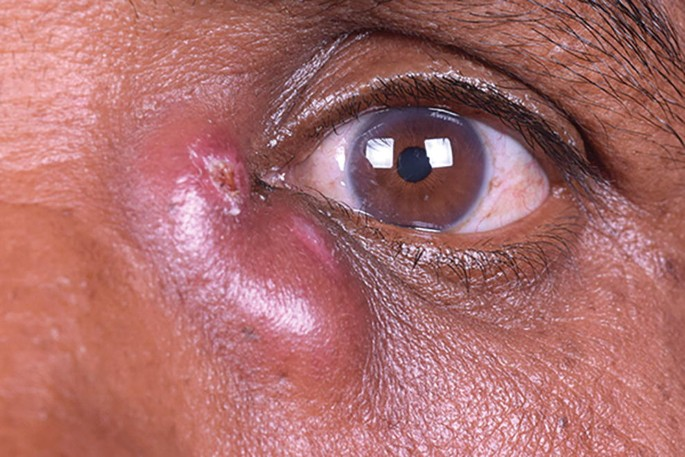
- Painful swelling in the infero-medial portion of the eye. The pain may be referred to the forehead, nose, cheek and upper teeth.
- Erythema and edema over the medial canthus
- Malaise and fever
- Regional lymph node swelling
- Mucopurulent discharge upon exerting pressure over the medial canthus
- Epiphora
- Investigations Blood cultures are specifically indicated in patients presenting with toxic symptoms and visual changes.
- Complete blood count – check for leukocytosis
- Blood and pus culture – help determine causative microorganism and antibiotic treatment.
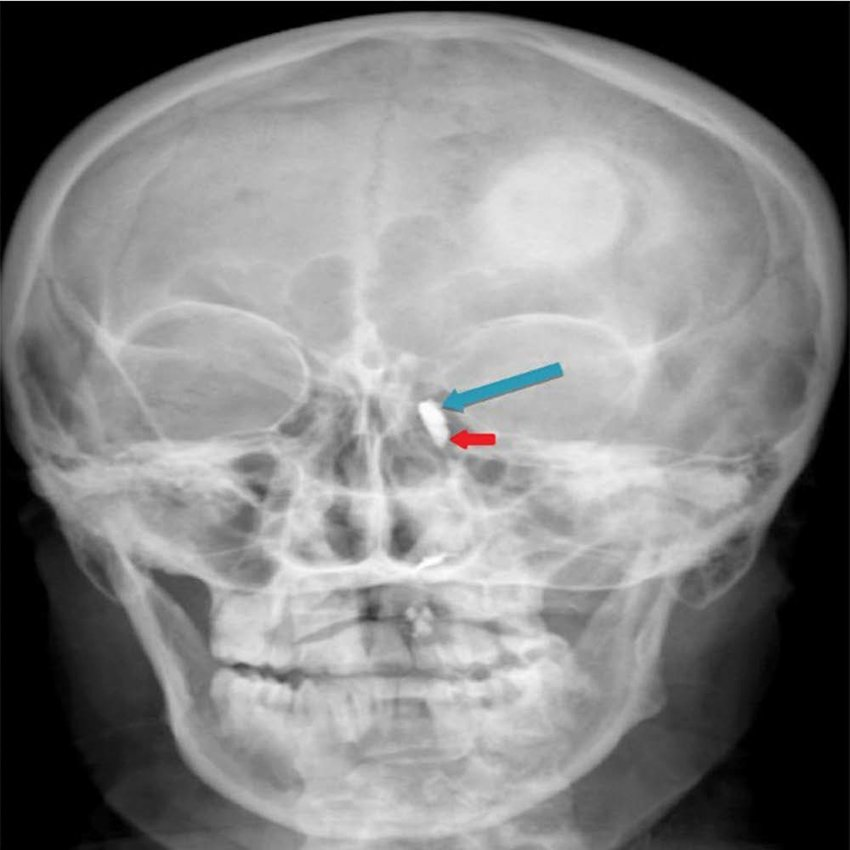
- CT scan if trauma was involved and if extensive infection is suspected.
- Dacryocystography – check for anatomical abnormalities
- Nasal endoscopy – rule out hypertrophy of the inferior turbinate, septal deviation and inferior meatal swelling.
- Fluorescein dye disappearance test (DDT) – administration of dye over the eye followed by slit lamp examination. If the dye persists for longer than five minutes it points to an obstruction in the lacrimal drainage system.
- Treatment Start by reducing the acute symptoms using antibiotics, pus drainage and warm compresses. Once they have subsided consider surgery for persistent relief.
- Oral antibiotics with gram positive coverage
- Warm compresses and Crigler massage
- Surgical – preferred is dacryocystorhinostomy (DCR). Balloon dacryoplasty can be done alternatively.
- Complications
- Preseptal cellulitis
- Orbital cellulitis
- Orbital abscess
- Lacrimal fistulas
- Lacrimal abscess
- Meningitis
- Cavernous sinus thrombosis
- Vision loss
- Differentials
- Hordeolum – small, circumscribed, non-mobile swelling
- Preseptal cellulitis
- Orbital cellulitis – eye movements will be limited
- Canaliculitis
- Dacryoadenitis
- Frontal, maxillary and ethmoid sinusitis
- Infected sebaceous cysts
- Lower eyelid ectropion
- Punctal ectropion
- Allergic rhinitis
- Lacrimal sac or sinonasal tumor

Chronic dacryocystitis
Chronic dacryocystitis is characterised by an insidious onset of symptoms due to nasolacrimal obstruction secondary to chronic inflammation of the nasal mucosa or connective tissue surrounding the region.
- Etiology Occurs due to systemic diseases such as:
- Wegener granulomatosis
- Sarcoidosis
- Systemic lupus erythematosus
- Repeated infections in the lacrimal system
- Dacryoliths
- Signs and symptoms
- Excessive tearing – Initial symptom
- Formation of a mucocele
- Release of mucopurulent material upon applying pressure on the lacrimal sac
- Mattering – collection of eye debris in the corner of the eyes
- Conjunctival injection
- Decrease in visual acuity due to accumulated tear film
- Investigations Apart from the investigations mentioned under Acute Dacryocystitis the following serological tests are carried out to rule out systemic conditions:
- Antineutrophilic cytoplasmic antibody (ANCA) testing – granulomatosis with polyangiitis (Wegener granulomatosis)
- Antinuclear antibody testing (ANA) and double stranded DNA (dsDNA) – systemic lupus erythematosus
- Treatment Mostly treated surgically:
- Lacrimal probing and irrigation is the first line treatmentPatients progress to need further surgical treatment: Balloon dacryoplasty, nasolacrimal intubation, nasolacrimal stenting. If these therapies fail, consider dacryocystorhinostomy (DCR)

Congenital Dacryocystitis
This is the inflammation of the lacrimal sac occurring in newborn infants secondary to nasolacrimal duct obstruction. Also known as dacryocystitis neonatorum or infantile dacryocystitis.
Occurs in 1 out of 3884 live births

- Etiology
- Occurs typically due to membranous occlusion of the valve of Hasner, which is located in the distal portion of the nasolacrimal duct.
- This obstruction of the nasolacrimal duct leads to stasis of secretions, especially amniotic fluid, which when retained becomes purulent leading to infantile dacryocystitis.
- Bacteria involved include: Staphylococcus species*, Streptococcus pneumoniae, Haemophilus influenzae, Enterobacteriaceae* species.
- Other causes are congenital non-canalisation and bony occlusion of the nasolacrimal duct.
- Signs and symptoms
- Epiphora
- Mucopurulent discharge from eye
- Medial eye swelling
- Erythema over eye
- Tenderness over eye
- Positive regurgitation test – pressure over the lacrimal sac leads to expulsion of collected fluid through one or both of the canaliculi and puncta confirming the presence of a nasolacrimal duct obstruction
- Treatment
- Mostly treated conservatively since 90% of cases resolve by one year of age.
- Warm compresses, Crigler massage (taught how do to it at home) and topical antibiotics are sufficient.
- If the disease progresses despite conservative management then consider: Lacrimal probing with a Bowman probe.
- If that fails then the following surgical techniques are recommended:
- Balloon catheter dilatation
- Dacryocystorhinostomy (DCR)
- Intubation with silicon tube
- Complications
- Lacrimal abscess
- Lacrimal fistula
- Recurrent conjunctivitis
- Brain abscess
- Meningitis
- Sepsis
- Orbital cellulitis
- Differentials
- Ophthalmia neonatorum
- Congenital glaucoma
- Foreign body
- Corneal infection
- Corneal dystrophies
- Prognosis
- 90% of cases resolve under conservative management after one year.
- Prompt diagnosis and treatment are key to a good prognosis as seen above there are many complications that may prove fatal if the disease is left to progress.
Resources
https://eyewiki.aao.org/Dacryocystitis
https://www.ncbi.nlm.nih.gov/books/NBK470565/#:~:text=Dacryocystitis is an inflammatory condition,discharge from the tear duct.
https://emedicine.medscape.com/article/1210688-overview
Lang, Ophthalmology textbook