What are the differences between prokaryotes and eukaryotes?
| Prokaryotes | Eukaryotes |
|---|---|
| Circular DNA without proteins | Complex of DNA with proteins |
| Nucleoid and plasma | Nucleus and mitochondrial DNA |
| Ribosomes are absent | Ribosomes are present |
| Cytoplasmic organelles are absent | Cytoplasmic organelles are present |
| Cell wall is present | Cell wall is absent |
| Reproduce by binary fission | Reproduce by mitosis and meiosis |
What are the differences between gram positive and gram negative bacterial cell wall
| Gram positive cell wall | Gram negative cell wall | |
|---|---|---|
| Peptidoglycan | Thick | Thin |
| Teichoic acid and Lipoteichoid acid | Present | Absent |
| Lipopolysaccharide | Absent | Present |
| Outer membrane | Absent | Present |
| Periplasm | Absent | Present |
| Porins | Absent | Present |
Compare and contrast bacterial endotoxin and exotoxin
| Endotoxin | Exotoxin | |
|---|---|---|
| Source | Gram positive and gram negative bacteria | Outer cell membrane of gram negative bacteria |
| Secreted | Yes | No |
| Structure | Polypeptide | Lipid A component of Lipopolysaccharide that is released when lysed |
| Gene | Plasmid or bacteriophage | Bacterial chromosome |
| Toxicity | High | Low |
| Clinical effect | Varies | Fever, Shock, DIC |
| MOA | Varies | Induces TNF, IL-1 and IL-6 production |
| Antigenicity | Induced high-titre antibodies called antitoxins | Poorly antigenic |
| Vaccines | Toxoids | No vaccine available |
| Heat stability | Destroyed rapidly at 60 C (except heat stable toxins) | Stable at 100 C for I hour |
| Typical diseases | Tetanus, Botulism, Diphtheria, Cholera | Sepsis |
- Describe the definition of facultative anaerobic bacteria
- Bacteria that can use oxygen for ATP generation but may switch to anaerobic metabolism when necessary
- Examples: Staphylococcus, Streptococcus, Gram-negative bacteria in the gut
- What are the possible mechanisms of acquired penicillin (cell wall antibiotic) resistance of bacteria? Mention at least 3 mechanisms
- Production of penicillinase: This is an enzyme that breaks down penicillin, making it ineffective against the bacteria that produce it.
- Alteration of penicillin-binding proteins: Penicillin works by binding to certain proteins in the bacterial cell wall, and bacteria can acquire resistance by altering the structure of these proteins so that the penicillin cannot bind to them.
- Efflux pumps: These are proteins that are present in the cell membrane of some bacteria, and they can actively pump penicillin out of the cell, reducing its effectiveness against the bacteria.
- Changes in the structure of the cell wall: Some bacteria can acquire resistance to penicillin by making changes to the structure of their cell wall, which makes it more difficult for the antibiotic to penetrate and attack the bacteria.
- Genetic mutation: Bacteria can also acquire resistance to penicillin by undergoing genetic mutations that alter their susceptibility to the antibiotic
- Mention 4 groups of antibiotics inhibiting protein synthesis of bacteria
- 30S ribosomal subunit:
- Aminoglycosides e.g. gentamicin, streptomycin, neomycin
- Tetracyclines e.g. tetracycline, doxycycline
- Glycylcyclines e.g. tigecycline (Tetracycline derivative)
- 50S ribosomal subunit:
- Macrolides and ketolides e.g. erythromycin, clarithromycin, azithromycin
- Lincosamides e.g. clindamycin
- Streptogramins e.g. quinupristin-dalfopristin
- Oxazolidinones (linezolid)
- Amphenicols (chloramphenicol)
- 30S ribosomal subunit:
- Mention groups of antibiotics inhibiting cell wall synthesis of a bacteria
- Beta-lactams
- Penicillins
- Cephalosporins
- Carbapenems e.g. imipenem, meropenem
- Monobactams e.g. aztreonam
- Glycopeptides e.g. vancomycin
- Epoxides e.g. fosfomycin
- Lipopeptides e.g. daptomycin
- Beta-lactams
- Describe Antimicrobial resistance (AMR), including the mechanisms of resistance and factors that influence resistance.
- Antimicrobial resistance occurs when microbes develop mechanisms that can protect them from antimicrobials.
- It can be inherent (natural) or acquired (Vertical or horizontal spread).
- Horizontal spread of AMR is via transformation, conjugation and transduction
- Mechanisms involved are Genetic (chromosomal, plasmid-mediated) and Non-genetic (inactivating enzymes, efflux pumps, altered permeability, target alteration).
- AMR is influenced by antimicrobial misuse and lack of enforcement of legislation over antimicrobial use.
- The lac operon contains 3 structural genes that code for enzymes involved in lactose metabolism, describe these genes.
- Lac Z: Beta-galactosidase gene: Cleaves lactose into galactose and glucose
- Lac Y: permease gene: Transports lactose through the cell membrane
- Lac A: transacetylase gene: Degrades toxic substances, which are transported with lactose in the cell
- Describe the architecture of the bacterial cell wall
- Murein layer (Peptidoglycan)
- Overlapping lattice of two sugars: N- acetylmuramic acid (NAM) and N- acetylglucosamine (NAG) interlinked by peptide bridges
- Attached to each NAM is a side chain of 4 amino acids: L- alanine, D- alanine, D- glutamic acid, Diamino pimelic acid. Cross- linked by transpeptidase.
- Present in al bacteria except Mycoplasma.
- AFB have mycolic acid, a LBCFA bound via polisaccharide to the peptidoglycan (Stained by Z-N staining)
- Gram positive bacteria have Lipoteichoic acids in their cell walls.
- Destroyed by autolysins and lysozymes.
- Murein layer (Peptidoglycan)
- Describe the microbial capsule, including staining and serologic methods for its detection ****
- Bacterial structure composed of an organised layer of polysaccharides
- May contain polypeptides (B.anthracis has poly- D- glutamate )
- Highly charged and hydrophilic
- Protects the bacteria from phagocytosis, mediates adherance, forms biofilms and is used to form conjugate vaccines
- Outline various capsule demonstration methods used in microbiology.
- Special capsular staining methods:
- Welch method
- Mc Fadyean Stain for B.anthracis
- Negative staining: India ink for Cryptococcus
- Serology: Quellung reaction for rapid identification of capsular serotypes eg. for S.pneumoniae, N.menengitidis, H.influenzae, Yersinia, Bacillus
- Special capsular staining methods:
- List encapsulated microorganisms.
- Encapsulated bugs (Yes some killer bacteria have pretty nice capsules)
- Yersinia pestis
- Streptococcus pneumonia, Streptococcus agalacticiae and Staphylococcus aureus
- Klebsiella pneumoniea
- Bacillus anthracis and Bordeterlla pertusis
- Haemophilus influenzae
- Pseudomonas aeruginosa
- Neisseria meningitidis
- Cryptococcus neoformans
- Encapsulated bugs (Yes some killer bacteria have pretty nice capsules)
- What are pili/fimbriae?
- Bacterial structure composed of pilins, mostly found in gram-ve bacteria,
- Ordnary pili are for adherence
- Sex pili are for conjugation
- Fibmriae are shorter and more numerous than pili, found in gram positive bacteria
- Bacterial structure composed of pilins, mostly found in gram-ve bacteria,
- What are flagellae?
- Bacterial structure composed of flagelin that confers motility and antigenicity (eg. H-antigen for Salmonella typhi along with O antigen)
- The bacteria may be monotrichous, lophotrichous, amphitrichous, peritrichous or amphilophotrichous
- What are spores?
- Spores are highly resistant resting stages formed during periods of starvation and other adverse conditions.
- Dipicolinic acid confers heat resistance to spores
- Spores are destroyed by autoclaving (steamed at 121 *C for 15 minutes)
- Spore forming bacteria include: Clostridium spp, Bacillus spp., and Coxiella burnetti
- Spores convert into a germinative state (germination) via the stages activation, initiation, and growth
- Spore morphology include:
- Non-bulging: Oval central, spherical central, oval subterminal
- Bulging: Free spore, spherical terminal, oval terminal and oval subterminal
- B.anthracis is used a bioterrorism agent while B.sterothermophilus is used as a biological indicator for autoclaving
- List the factors required for bacterial growth.
- Oxygen
- Temperature
- pH
- Nutrients
- Classify bacteria according to their oxygen growth requirements.
- **Obligate aerobes (**Nagging Pests Must Breath)
- Norcardia
- Pseudomonas aeruginosa
- Mycobacterium tuberculosis
- **Obligate anaerobes (**Anaerobes Can’t Breathe Air)
- Clostridium
- Bacteroides
- Actinomyces
- Microaerophilic
- Helicobacter
- Campylobacter
- **Facultative anaerobes (**Most pathogenic bacteria)
- Eschericia coli
- Aerotolerant anaerobes
- Lactobacillus plantarum
- Capnophilic
- Brucella abortius
- **Obligate aerobes (**Nagging Pests Must Breath)
- Classify bacteria according to their temperature growth requirements.
- Thermophiles (>40*C): B. stearothermophilus
- Mesophiles (20 – 40 *C): Most pathogens
- Psychrophhiles (0-20*C) : Soil and water saprophytes
- Classify bacteria according to their pH growth requirements.
- Alkalophiles (>8.5)
- Neutrophiles (5-8)
- Acidophiles (<5.5)
- Classify bacteria according to their nutritional growth requirements.
- Carbon sources (autotrophs and heterotrophs)
- Hydrogen donor (Organotrophs and lithotrophs)
- Energy sources (Phototrophs and chemotrophs)
- List the classes of B-Lactam antibiotics.
- Penicillins
- Cephalosporins
- B-lactam + B-lactamase inhibitors
- Carbapenems
- Monobactams
- Classify antibiotics according to their site of action.
- Cell wall-intracellularly: fosfomycin, cycloserine
- Cell wall-membrane: Bacitracin
- Cell wall- formation: B-lactam antibiotics, vancomycin
- Inhibition of mycolic acid synthesis: Isoniazid
- Cytoplasmic membranes: Polymixins, Gramicidins, Lipopeptides
- Nucleic acids: Rifamycins, Fluoroquinolones, Nitromidazoles, Nitrofuran
- Ribosomes 30s: Aminoglycosides, Tetracyclines, Glycylglycines
- Ribosomes 50s: Chloramphenicol, Macrolides, Ketolide, Lincosamides, Oxazlidinones, Streptogramins, Mupirocin, Fusidone
- Inhibition of folic acid synthesis: Sulfonamides, Trimethropim
- List the steps involved in identification of bacteria.
- Proper patient history
- Obtain an appropriate specimen
- Macroscopic examination of specimen
- Cell morphology (Staining)
- Culture morphology (Colony)
- Biochemical tests
- Serologic tests: Direct slide agglutination, Latex agglutination, Flocculation, ELISA, Immunochromatography
- Phage typing
- Genetic (DNA) typing
- Antibiotic susceptibility testing
- What are the steps involved in gram staining?
- Primary stain (crystal violet)
- Mordant (Gram’s iodine)
- Decolorizer (Alcohol or acetone)
- Counterstain (Sarfranin or Carbol-fuschin )
- Gram positive are purple
- Gram negative are pink
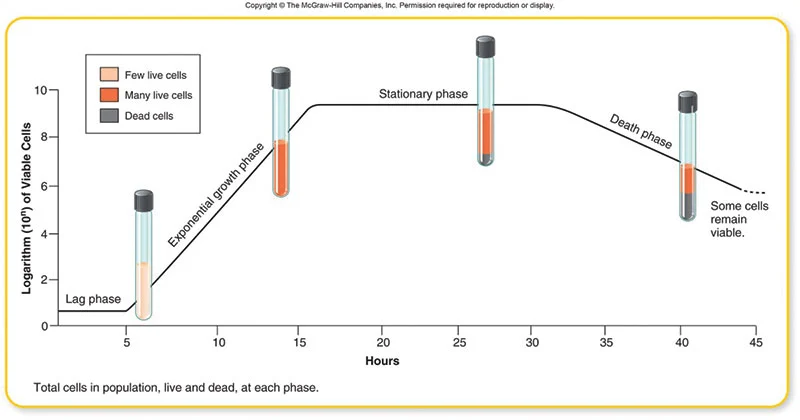
- Describe the bacterial growth curve.
- Generation time is the time (t) required for bacteria to give rise to 2 daughter cells
- E. coli and most medically important bacteria have a generation time of 20 min
- Tubercle bacili has a generation time of 20h
- Tubercle leprae has a generation time of 20 days
- Generation time is the time (t) required for bacteria to give rise to 2 daughter cells
- Describe the different categories of culture media.
- Basal media: Culture non-fastidious bugs. Examples: Nutrient agar, nutrient broth
- Enriched media: Contain nutrients required for growth. Examples: CBA, BA, Eaton agar
- Selective media: Inhibit growth of certain bugs to increase concentration of the other. Examples: MSA, McConkey, Thayer martin VCN, Lowensterin-Jensen, TCBC
- Indicator (differential) media: organisms change colour of indicator. Examples: McConkey, MSA, TCBS, BA, SS-agar
- Enrichement media: broth media with selective properties to increase concentration before plating. Examples: selenite F, alkaline peptone water
- Transport media: Amie’s media
- Anaerobic media: Robertson cooked media (RCM)
- Describe the methods of genetic variation and gene transfer in bacteria.
- Transposons
- Class I and Class II transposons
- Programmed rearrangement
- Causes antigenic variation in Neisseria gonorrhoea, B. recurrentis and T. brucei
- Transformation
- Transfer of DNA from one cell into another; occurs during the late log phase or sporulation
- Seen in H. Influenzae, Pneumococci and Bacillus spp.
- Transduction
- Transfer of DNA between cells by bacteriophages
- Includes Generalized transduction and specialized transduction
- Conjugation
- Infectious spread of a plasmid via sex pilus
- The F-lac plasmid of E.coli can transfer lac operon genes to non-lactose fermenting organisms
- Transposons
- Describe the classification of gram positive bacteria (algorithm). NO STRESS OVRPS – Viridans is optochin resistant, pneumoniae is sensitive B-BRAS – Group B strep is bacitrain resistant, Group A strep is bacitracin sensitive)



