- Name the type of papillae on the dorsal surface of the tongue and state their respective locations on the tongue
- Filiform papillae: anterior dorsal tongue
- Fungiform papillae: Tip of the tongue
- Circumvallate papillae: Anterior to the sulcus terminalis
- Foliate papillae: Lateral edges of the tongue
- Name the cell types of the taste bud
- Neuroepithelial (Sensory) cells: Elongated cells that have microvilli on their apical surface and are connected with afferent endings of CN VII, CN IX and CN X at their base
- Supporting cells: Similar to sensory but they do not synapse with afferent nerve endings.
- Basal cells: Stem cells for sensory and supporting cells.
- Describe the histological structure of the ductal and secretory part of a mixed salivary gland
- Secretory part: Mucous cells with Serous demilunes (Fr. half-moon)
- Ductal part
- Intercalated ducts
- Low cuboidal lining
- Bicarbonate secretion and Cl- absorption
- *Carbonic anhydrase activity
- Striated ducts
- simple cuboidal lining that gradually becomes columnar
- Na+ reabsorption
- K+ and bicarbonate secretion
- Excretory ducts
- simple cuboidal → pseudostratified columnar/ stratified cuboidal → stratified squamous lining
- Opens into the oral cavity
- Intercalated ducts
- Describe the histological structure of the oesophagus
- Mucosa
- Non-keratinizing stratified squamous epithelium
- Diffuse lymphatic tissue the in lamina propria
- Muscularis mucosa (longitudinal smooth muscles)
- Submucosa
- Dense irregular connective tissue
- Submucosal (Meissner’s) plexus
- Muscularis Externa
- Longitudinal and circular muscle layers
- Myenteric (Auerbach’s) plexus
- Adventitia (thoracic part) or Serosa (Visceral peritoneum in the abdominal part)
- Mucosa
- Describe the histological appearance of the parenchyma of the parotid gland
- Acinus
- Serous acini
- Pyramid shaped serous cells
- Intercalated duct
- Well developed
- Low cuboidal epithelial cells
- Striated duct
- Well developed
- Simple cuboidal epithelium that gradually becomes columnar as it approaches the excretory duct – basal infoldings w/elongated mitochondria and basolateral folds
- Excretory duct
- simple cuboidal → pseudostratified columnar/stratified cuboidal → stratified squamous epithelium
- Acinus
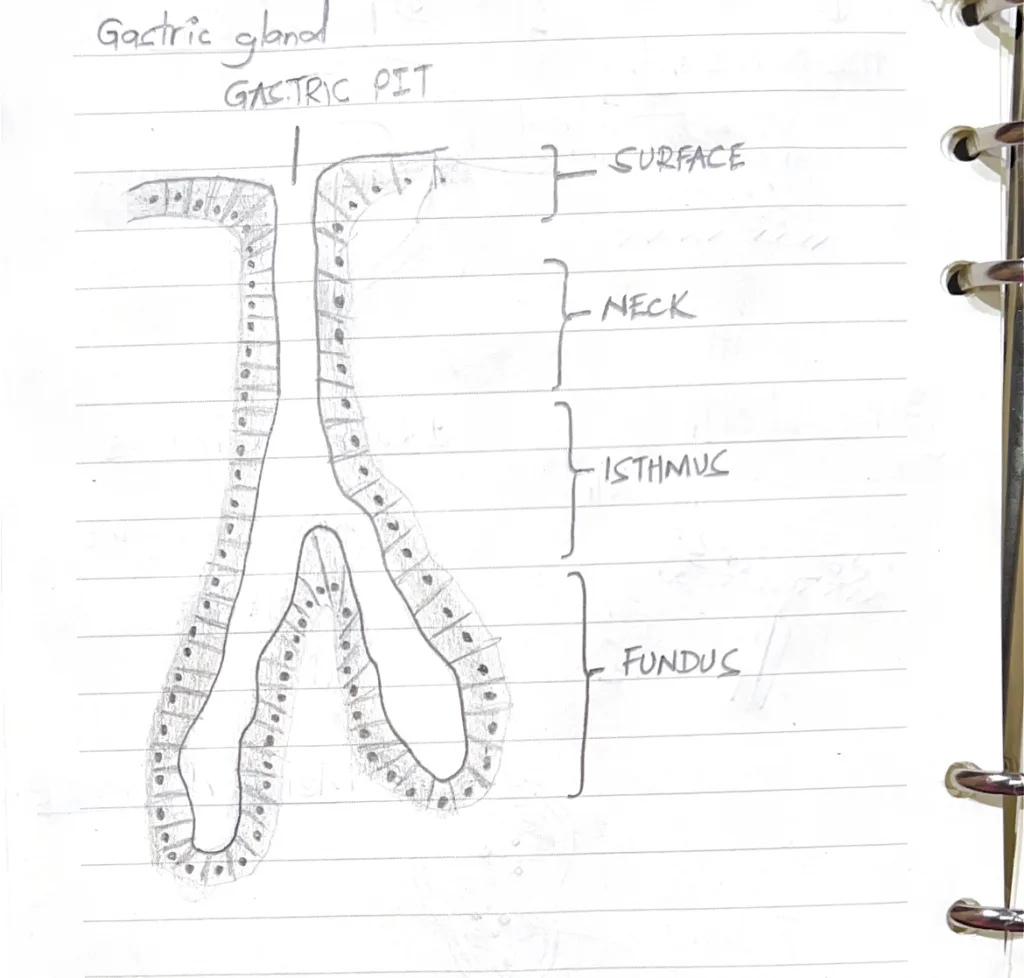
- Describe the gastric pit and gland with reference to the distribution of cells and function
- Gastric pits (foveolae) are openings visible on the stomach mucosa at higher magnifications.Surface:
- Surface mucous cells: Mucin secretion
- Undifferentiated adult stem cells: regeneration
- Parietal cell: HCl and Intrinsic factor secretionMucous neck cells: Mucin secretionEnteroendocrine cells: Hormone secretion
- Chief cells: Zymogen secretionParietal cellsEnteroendocrine cells
- Gastric pits (foveolae) are openings visible on the stomach mucosa at higher magnifications.Surface:
- Describe the parts and respective functions of the ductal system of salivary glands
- Intercalated ducts: Leads from the acinus
- Low cuboidal lining
- Bicarbonate secretion and Cl- absorption
- *Carbonic anhydrase activity
- Striated ducts: because of the presence of striations in the basal aspect
- simple cuboidal lining that gradually becomes columnar
- Na+ reabsorption
- K+ and bicarbonate secretion
- Excretory ducts: larger ducts that empty into the oral cavity
- simple cuboidal → pseudostratified columnar/ stratified cuboidal → stratified squamous lining
- Opens into the oral cavity
- Intercalated ducts: Leads from the acinus
- Name the cell types of the gastric gland epithelium and state their respective functions
- Mucous neck cells – mucin secretion
- Chief cells – pepsinogen and weak lipase secretion
- Parietal cells – HCl and intrinsic factor secretion
- Enteroendocrine cells – hormone secretion
- Undifferentiated adult stem cells – regeneration
State the structural differences in parietal cells between its active and inactive forms
| Active parietal cell | Inactive parietal cell | |
|---|---|---|
| Microvilli in canaliculi | Increased | Decreased |
| Tubulovesicular system | Reduced in number or disappear as they are inserted into the cell membrane | Present in the cytoplasm |
| Mitochondria | Numerous with complex cristae | Reduced in number |
- Name the cell types of the duodenal epithelium and state their respective functions
- Enterocytes – absorption
- Goblet cells – mucin secretion
- Paneth cells – antimicrobial substance secretion
- Enteroendocrine cells – produce various paracrine and endocrine hormones
- M cells (Microfold cells) – selective endocytosis of antigens and transport to intraepithelial lymphocytes and macrophages which then travel to lymphoid tissue to mount immune responses
- Describe the lamina propria of the small intestine
- Mucosal glands: extend into the lamina propria
- Blood and lymphatic vessels: Fenestrated capillaries and lymphatic capillaries that absorb metabolites, lipids, and proteins
- Lymphatic tissue: Lymphocytes, plasma cells, macrophages, eosinophils, mast cells
- Diffuse lymphatic tissue (GALT): Diffusely arranged Lymphocytes and plasma cells
- Peyer’s patches: Aggregated lymphocytes that occupies the lamina propria and submucosa.
- What is a “collagen table’ in the large intestines? State its significance
- A thick layer of collagen and proteoglycans that lies between the basal lamina of the epithelium and that of the fenestrated absorptive venous capillaries
- Regulates water and electrolyte transport from the intercellular compartment of the epithelium to the vascular compartment
- Describe the mucosa of the rectum and give one clinical correlate
- Glands: Straight, tubular intestinal glands
- Epithelium: Simple columnar epithelium
- Lamina propria: Has a collagen table, pericryptal fibroblast sheath, GALT and lymphatics
- Clinical correlate: Colorectal cancer
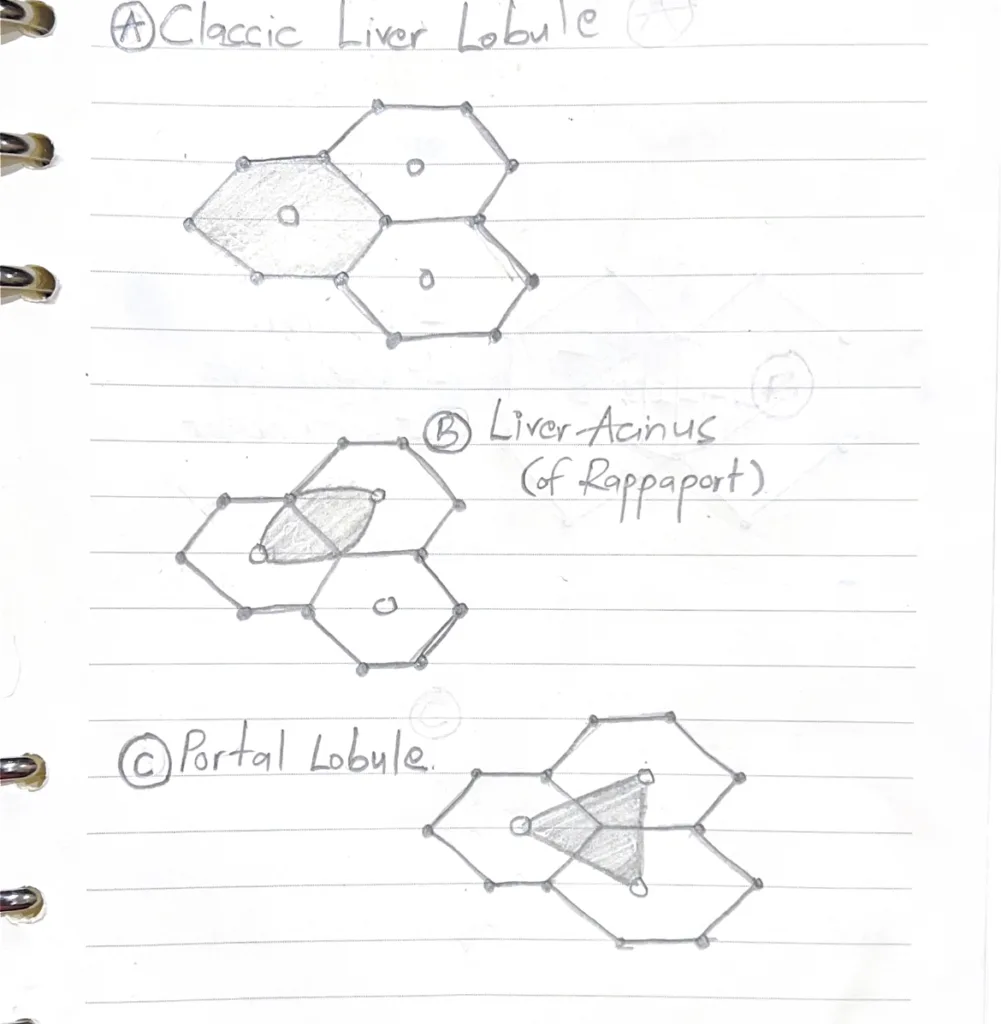
With the aid of diagrams outline the classification of liver lobules
- Classic Liver Lobule (A): Based on blood flow pattern, with the central vein as the axis
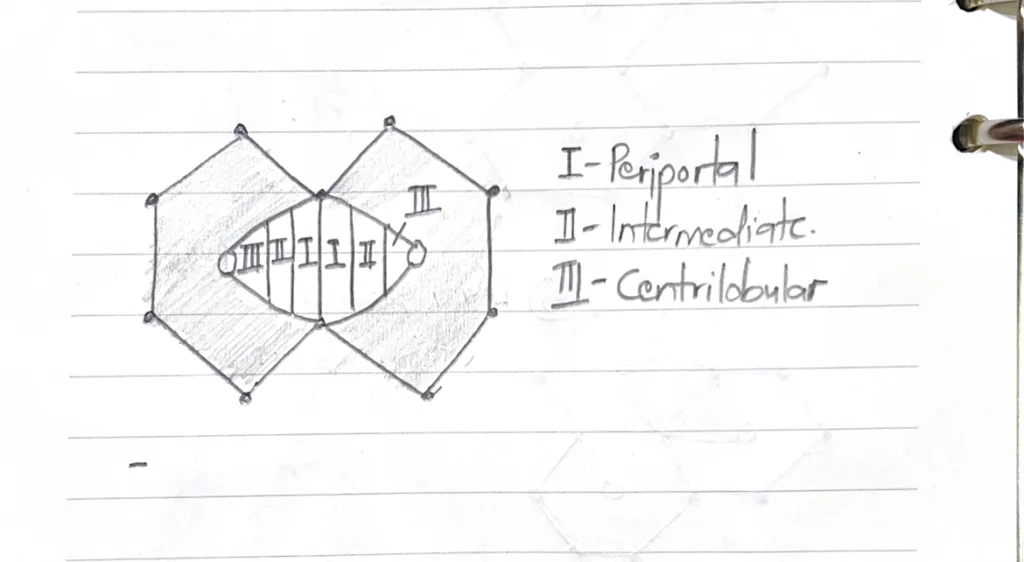
- Liver acinus (B): Based on susceptibility to injury. Has 3 zones
- Portal lobule (C): Based on biliary drainage, with the portal triad as the axis
Illustrate the zonation of a liver acinus
- Describe the following regarding the liver: Space of Disse, Kupffer cells, Ito cells, Glisson’s Capsule, Space of Mal
- Space of Disse: Perisinusoidal space. Found between the hepatocytes and sinusoids
- Kupffer cells: Phagocytic macrophages within the lumen of liver sinusoids
- Ito cells: Hepatic stellate cells that store vitamin A, and differentiate into myofibroblasts during pathological conditions (eg. cause bridging fibrosis by secreting collagen – a feature of liver cirrhosis)
- Glisson’s capsule: Fibrous connective tissue enclosing the liver
- Space of Mal: Periportal space between the stroma of the portal canal and outermost hepatocytes
- What are the histological peculiarities of the gall bladder wall
- Absent muscularis mucosae
- Absent submucosa
- Rokitansky-Aschoff sinuses extend through the muscularis externa. They are pathological changes.
- Smooth muscle bundles in muscularis externa are randomly oriented
- Name the principal cell types of the islets of Langerhan and state their respective secretions
- A cells – Glucagon production
- B cells – Insulin production
- D cells – Somatostatin production
- PP cells (F cells) – pancreatic polypeptide secretion
- D1 cell – Vasoactive intestinal polypeptide secretion
- EC cell – secretin, motilin and substance P production
- Epsilon cell – Ghrelin production